Treating Burning Mouth Syndrome
How to help patients deal with this painful, chronic, and enigmatic condition.
This course was published in the December 2009 issue and expires December 2012. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define burning mouth syndrome.
- Identify various systemic, local, psychogenic, and neuropathic factors associated with burning mouth syndrome.
- List various treatments options for patients with burning mouth syndrome.
- Describe the role of dental health care workers in helping patients cope with burning mouth syndrome.
Burning mouth syndrome (BMS) is a chronic, painful condition with no clear etiology or specific, proven treatment. BMS is also known as burning tongue syndrome, glossodynia, glossopyrosis, stomatodynia, stomatopyrosis, and oral dysesthesia.1,2 The syndrome is characterized by burning and/or painful sensations of the mouth, usually in the absence of clinical or laboratory findings.3 It can occur anywhere in the mouth. However, the most frequently affected sites are the tip and anterior two-thirds of the tongue followed by the lower lip and hard palate.4 Patients typically report no pain in the morning with increased discomfort as the day progresses. The prevalence rate of BMS in the general population varies from 0.7% to 15%. It is more common in women (5.5%) than men (1.6%).5-7
DIAGNOSIS
There is no clear consensus on the etiology, pathogenesis, or treatment of BMS.8 Most patients usually consult several clinicians, often without a clear explanation or appropriate diagnosis for their painful condition.9 Diagnosis of BMS is dependent on a detailed history of clinical signs and symptoms; a thorough intraoral and extraoral examination; and an assessment of local, systemic, and environmental factors. Clinical signs and symptoms of BMS may include a burning sensation of the tongue; pain; xerostomia; sialorrhea; tongue ulcers; dysphagia; dysgeusia; sensation of a lump in the throat; parafunctional habits, such as bruxism and tongue thrusting; and malodor.7,10
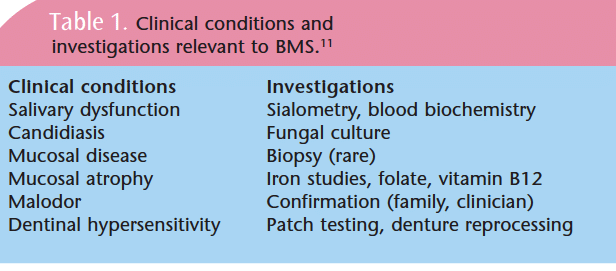
For some patients, there may be a link between BMS and other conditions such as Sjögren’s syndrome or fungal infections. Therefore, local, systemic, and environmental factors need to be investigated (Table 1).11 If the cause can be identified, the disorder is referred to as secondary BMS.10 If no cause of symptoms can be identified, the diagnosis is primary or idiopathic BMS.10
ETIOLOGY
The etiology of BMS is unknown with much debate appearing in the literature, which poses a problem for clinicians who are trying to diagnose the condition and may lead to significant frustration for patients.12 The average patient visits approximately three practitioners before being correctly diagnosed.9 Various systemic, local, psychogenic, and neuropathic factors are associated with BMS.
SYSTEMIC FACTORS
Systemic conditions linked to the symptoms of BMS include menopause, diabetes, and nutritional deficiencies.12 Hormonal changes are important factors in BMS. Women are approximately seven times more likely to be affected than men, and approximately 90% of the women participating in BMS studies are post-menopausal.8,12 The onset of pain tends to range from 3 years prior to menopause to 12 years after menopause, and BMS has been reported in 10% to 40% of women presenting for treatment of menopausal symptoms.8,12 However, estrogen replacement therapy does not relieve pain in all cases.12
Nutritional deficiencies—particularly in vitamins B1, B2, B6, and B12—may be present in patients who have BMS.8,12 Low blood serum levels of iron have also been implicated.12 However, nutritional supplementation does not always provide symptom relief.12
There is some evidence that type 2 diabetes may contribute to the development of BMS but the correlation is still controversial. Some researchers believe that a link exists between the type of insulin used and the symptoms of BMS, while others surmise that complaints of burning mouth among people who have diabetes are probably caused by candidiasis.12 BMS symptoms in these patients may also be related to neuropathy, which is a common complication of type 2 diabetes.12
 Case reports have also linked burning mouth symptoms and loss of taste sensation to the use of angiotensin-converting enzyme inhibitors (medications used for the treatment of hypertension and congestive heart failure). Symptoms tend to subside within several weeks of discontinuing these medications.8
Case reports have also linked burning mouth symptoms and loss of taste sensation to the use of angiotensin-converting enzyme inhibitors (medications used for the treatment of hypertension and congestive heart failure). Symptoms tend to subside within several weeks of discontinuing these medications.8
LOCAL FACTORS
Many local conditions have been implicated in symptoms of BMS including: candidiasis, lichen planus, xerostomia, allergic reactions, geographic tongue, recent dental treatment, and galvanic currents between dissimilar metals.8,12,13 Some local factors that show stronger evidence include local nerve trauma, oral parafunctional habits, and salivary gland dysfunction.12
Peripheral nerve injury may play a role in the symptoms of BMS because the symptoms show a pattern similar to those observed in some inflammatory neural conditions.12 Several studies also suggest that parafunctional habits, such as tongue thrusting, bruxism, and clenching, are more common in patients who have BMS.12,13 These activities are often related to anxiety, which is more prevalent in patients who have BMS.10,12
Patients who have BMS experience a higher incidence of xerostomia, therefore, salivary gland dysfunction is suspected to play a role in the symptoms.8,12 Reduction in salivary flow may be due to radiation therapy, systemic disease, or side effects of different medications.12 Candidiasis has also been proposed as a cause of BMS, and while it can cause burning pain, it is not more prevalent in patients who have BMS.8
PSYCHOGENIC FACTORS
Evidence suggests that many BMS patients show signs of psychological problems, including mood changes, anxiety, depression, personality disorders, and an increased tendency toward somatization (the chronic and persistent complaint of physical symptoms that have no identifiable etiology) leading some researchers to believe that psychogenic factors may lead to BMS.10,13 However, these symptoms may be secondary to living in chronic pain and the frustration of visiting one practitioner after another, rather than the cause of BMS. Psychological problems are common in patients who experience chronic pain.8,10 In one study, patients who had BMS reported adverse life events more frequently, such as having a difficult childhood, poor adaptation to school and work, loss of a loved one, divorce, retirement, or difficulty in understanding, processing, or describing emotions (alexithymia).13
NEUROPATHY
Patients with BMS often exhibit taste changes and sensory dysfunctions, suggesting that there may be a neuropathic basis to the condition.12 An underlying disorder of the autonomic innervation of the oral cavity may be present, leading to abnormal pain perception, raised trigeminal nerve sensitivity, alterations in nerve transmission, and disturbances of the mucosal neurovascular microcirculatory system.12
More than two-thirds of patients who have BMS complain of altered taste sensation, often described as a spontaneous metallic taste.14 Results of a 2007 study suggest that BMS may be a form of neuropathic pain related to dysfunction of the chorda tympani nerve, which is responsible for taste sensation in the anterior two-thirds of the tongue.13
TREATMENT
Successful treatment of BMS is dependent on a number of factors including ascertaining a correct diagnosis followed by diagnosis confirmation, patient acceptance and understanding of the likely clinical course, and patient participation in the development of a treatment strategy.11 Patient compliance and feedback during treatment and the ongoing interest of the clinician are also important.11
Treatment options vary from no treatment (the most common) to physical therapy to laser therapy (seldom used).11 Pharmaceuticals such as anti-anxiety drugs and antidepressants are often prescribed. Tricyclic antidepressants in particular have proven helpful for some patients but not all.11 Other treatments include topicals, such as capsaicin; relaxation programs; exercise programs; alternative medications, such as alpha-lipoic acid; formal psychotherapy; cognitive behavior therapy; and alternative therapies, such as acupuncture and massage.11
Although only a limited number of properly constructed treatment trials have been conducted, treatments proven effective in controlled double-blind studies are cognitive behavior therapy; clonazepam, an anticonvulsant and muscle relaxant used either topically or systemically; and the nutritional supplement alpha-lipoic acid, which is a fatty acid found naturally inside every cell in the body that produces energy for the body’s everyday functions.11 One study found that 11 out of 31 patients reported benefit from taking 600 mg per day of alpha-lipoic acid in divided doses.15 However, this study was not a randomized, controlled, double-blind study, but rather subjective follow-up collected through phone surveys. A randomized, double-blind, placebo-controlled trial evaluated the effects of taking the plant species Hypericum perforatum extract or St. John’s Wort systemically in patients who have BMS and found no significant difference between patients who received a placebo and those who received the extract.16
A Cochrane Review looked at nine trials including the interventions of alpha-lipoic acid (three trials), anticonvulsants (one trial), antidepressants (two trials), cognitive behavior therapy (one trial), analgesics (one trial), and hormone replacement therapy (one trial).5 Only three interventions demonstrated a reduction in BMS symptoms: alpha-lipoic acid, the anticonvulsant clonazepam, and cognitive behavior therapy.5 The Cochrane Review concluded there is insufficient evidence to show the effect of pain killers, hormones, or antidepressants in treating BMS but there is some evidence that learning to cope with the disorder, anticonvulsants, and alpha-lipoic acid may help.5
GLOSSARY OF TERMS
Alexithymia: a clinical feature common in posttraumatic stress disorder characterized by the inability to identify and articulate feelings
Dysesthesia: abnormal sensations of the mouth, such as a feeling of numbness, tingling, prickling, or burning
Dysgeusia: impairment or perversion of taste so that normal tastes are interpreted as being unpleasant or completely different from the characteristic taste of a particular food
Dysphagia: inability to or difficulty in swallowing
Glossodynia: pain in the tongue
Glossopyrosis: a burning sensation of the tongue
Neuropathy: disorders of the nerves of the peripheral nervous system
Sialorrhea: excessive secretion of saliva
Stomatodynia: pain in the mouth
Stomatopyrosis: a burning sensation in the mouth
Source: Venes D, ed. Taber’s Cyclopedic Medical Dictionary. 19th ed. Philadelphia: F.A. Davis Co; 2001.
DENTAL PRACTICE CONSIDERATIONS
Addressing BMS has implications for all members of the dental team and includes individualized assessment and treatment; empathy; palliative care; treatment of underlying factors, such as xerostomia; and helping patients learn to cope. The daily prescription of .25 mg to 2 mg of clonazepam may be considered for short-term relief of pain. Patients should be prescribed the lowest dose initially with the dose then increasing by .25 mg per day until burning is relieved or side effects occur. As the dosage increases, the medication should be taken in three divided doses.8 Recommending an alpha-lipoic acid supplement may also be considered. The dose is 200 mg three times a day to be taken with food.17 If candidiasis is present, an anti-fungal should be prescribed.
After the medical history is reviewed, the dental hygienist should follow-up on medications the patient may be taking in relationship to BMS. Morning appointments may work best for patients because the pain increases as the day progresses. A thorough intraoral exam may reveal xerostomia, candidiasis, and/or possible signs of allergic hypersensitivity to dental materials.
The traditional treatment considerations for xerostomia are appropriate for patients who have BMS, including mechanical salivary stimulation through the use of sugarless gums and lozenges,18,19 saliva substitutes,18,20 mouth rinses, and other products made specifically for dry mouth.18 Strategies such as adequate hydration and taking frequent sips of water;19 using a cool air humidifier, particularly at night;19 using home fluorides, such as a prescription strength gel and toothpastes with 5,000 ppm;20 changing patients’ medication regimen; and prescribing medications for the relief of dry mouth, such as pilocarpine or cevimeline, may be helpful.18-20 Further recommendations include avoiding the use of mouthrinses and beverages containing alcohol, avoiding overly salted foods, avoiding foods and drinks high in sugar, and encouraging the practice of meticulous oral hygiene.20
The dental office may want to develop a referral list of other health care providers who can assist patients with nutritional assessment, behavioral modification, and alternative therapies to treat BMS.
Although the etiology and treatment for BMS is challenging for clinicians and frustrating for patients, the dental team is integral to helping patients cope with this painful oral syndrome.
REFERENCES
- Haveles EB. Applied Pharmacology of the Dental Hygienist. 5th ed. St. Louis: Mosby; 2007:264.
- Perno M. Burning mouth syndrome. J Dent Hyg. 2001;75:245-252.
- Terai H, Shimahara M. Tongue pain: burning mouth syndrome vs candida-associated lesion. Oral Diseases. 2006;13:440-442.
- Amenabar JM, Pawlowski J, Hilgert JB, et al. Anxiety and salivary cortisol levels in patients with burning mouth syndrome: case-control study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:460-465.
- Zakrzewska JM, Forssell H, Glenny AM. Interventions for the treatment of burning mouth syndrome (review). Cochrane Database Syst Rev. 2005;25:CD002779.
- López-Jornet P, Camacho-Alonso F, Lucero-Berdugo M. Quality of life in patients with burning mouth syndrome. J Oral Pathol Med. 2008;37:389-394.
- Scardina GA, Pisano T, Carini F, Valenza V, Messina P. Burning mouth syndrome an evaluation of in vivo microcirculation. J Am Dent Assoc. 2008;139:940-946.
- Grushka M, Epstein JB, Gorsky M. Burning mouth syndrome. Am Fam Physician. 2002;65:615-620.
- Mignogna MD, Fedele S, LoRusso L, Leuci S. The diagnosis of burning mouth syndrome represents a challenge for clinicians. J Orofac Pain. 2005;19:168-173.
- Karim K. Diagnosis and management of burning mouth syndrome. Nurse Prescribing. 2007;5(6):239-244.
- Savage NW, Boras VV, Barker K. Burning mouth syndrome: clinical presentation, diagnosis and treatment. Australas J Dermatol. 2006;47:77-83.
- Scala A, Checchi L, Montevecchi M, Marini I, Giamberardino MA. Update on burning mouth syndrome: overview and patient management. Crit Rev Oral Biol Med. 2003;14:275-291.
- Gao J, Chen L, Zhou J, Peng J. A case-control study on etiological factors involved in patients with burning mouth syndrome. J Oral Pathol Med. 2009;38:24-28.
- Eliav E, Kamran B, Schaham R, Czerninski R, Gracely R, Benoliel R. Evidence of chorda tympani dysfunction in patients with burning mouth syndrome. J Am Dent Assoc. 2007;138:628-633.
- Steele JC, Bruce AJ, Drage LA, Rogers RS 3rd. Alpha-lipoic acid treatment of 31 patients with sore, burning mouth. Oral Dis. 2008;14:529-532.
- Sardella A, Lodi G, Demarosi F, Tarozzi M, Canegallo L, Carrassi A. Hypericum perforatum extract in burning mouth syndrome: a randomized placebo-controlled study. J Oral Pathol Med. 2008;37:395-401.
- Suarez P, Clark GT. Burning mouth syndrome: an update on diagnosis and treatment methods. J Calif Dent Assoc. 2006;34: 611-632.
- Spolarich AE. Medication use and xerostomia. Dimensions of Dental Hygiene. 2005;3(7):22-24.
- Zunt S. Re-establishing a normal salivary flow. Dimensions of Dental Hygiene. 2006;4(5):30-32.
- Nanne, SM. Salivary substitutes and oral lubricants—providing patients with relief from xerostomia. The Journal of Practical Hygiene. 2007;16(1):17-19.
From Dimensions of Dental Hygiene. December 2009; 7(12): 36-39.



