KARELNOPPE/ISTOCK/GETTY IMAGES PLUS
KARELNOPPE/ISTOCK/GETTY IMAGES PLUS
Improving Dental Appointments with Hypnotherapy
This alternative modality can be used to enhance overall patient comfort while reducing fear and anxiety in the dental setting.
This course was published in the October 2020 issue and expires October 2023. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Describe early uses of hypnosis in dental settings, as well as applications for hypnotherapy.
- List key steps in the hypnosis process and potential concerns when using this form of therapy.
- Discuss the role of hypnosis in reducing clinicians’ reliance on pharmacological interventions.
The word “hypnosis” usually conjures images of show business hypnotists mesmerizing audience members to perform embarrassing acts on stage. Although there are misconceptions associated with hypnosis, it offers many benefits in the dental setting. Hypnotherapy is the term used to describe the therapeutic use of hypnosis, and can be traced to the early 1800s in the dental field. One of the first documented cases of hypnodontics, or hypnosis in dentistry, was performed in 1829 to assist with analgesia and ease fear during a tooth extraction.1 This led to pioneers in hypnodontics promoting it as an effective and reliable treatment alternative for patient management. Within dentistry, hypnosis can be used as a nonpharmacological intervention to enhance overall patient comfort and reduce dental anxiety.
Additional uses include (but are not limited to) controlling pain, bleeding, and swelling; reducing bruxism, gagging, and salivary production; providing analgesia and anesthesia; and promoting effective self-care habits.2 As such, oral health professionals are ideally positioned to be trained in the principles of hypnosis, including uses, benefits, limitations, and special considerations. Hypnosis does not have a standard definition.3,4 It is popularly defined in the medical literature as a “special trancelike state in which the subject’s attention is focused intensely on the hypnotist, while attention to other stimuli is markedly diminished.”5,6
Dental fear can be transformed and managed by shifting the patient’s focus of attention with hypnotic techniques. A significant component of relieving patient anxiety is through the use of iatrosedation or managing the patient through the oral health professional’s behavior.5 Iatrosedation is a form of communication between the provider and patient that can foster trust and build confidence. Besides hypnotherapy, there are multiple iatrosedation techniques, and most require some level of training.
- Acupressure is an alternative medicine technique involving the stimulation of pressure points. In dentistry, acupressure has been shown to help manage various conditions—in particular, pain control and anxiety.7–10
- Acupuncture acts by changing the way the nervous system processes pain signals while releasing natural painkillers.11,12 This approach has been used to manage a variety of dental conditions, including pain.11
- Aromatherapy is the use of essential oils that can invoke a variety of emotions through the sense of smell. In dentistry, lavender has been recommended for its aromatic effects on patient relaxation.13
- Audioanalgesia is the use of white noise (via earphones) to distract patients from perceived pain while decreasing dental anxiety.14 It can be used in conjunction with instrumental music or as a single modality.
- Biofeedback therapy uses electrodes to measure respiration, heart rate, muscle tension, skin temperature, blood flow, and blood pressure.15 Although it has been used to treat various conditions, anxiety relief is one of the most common applications.
- Electronic dental anesthesia involves transcutaneous electrical nerve stimulation, which has been used to help control chronic pain.16 Devices used in dentistry have been suggested as a promising alternative to traditional local anesthesia injection techniques.17
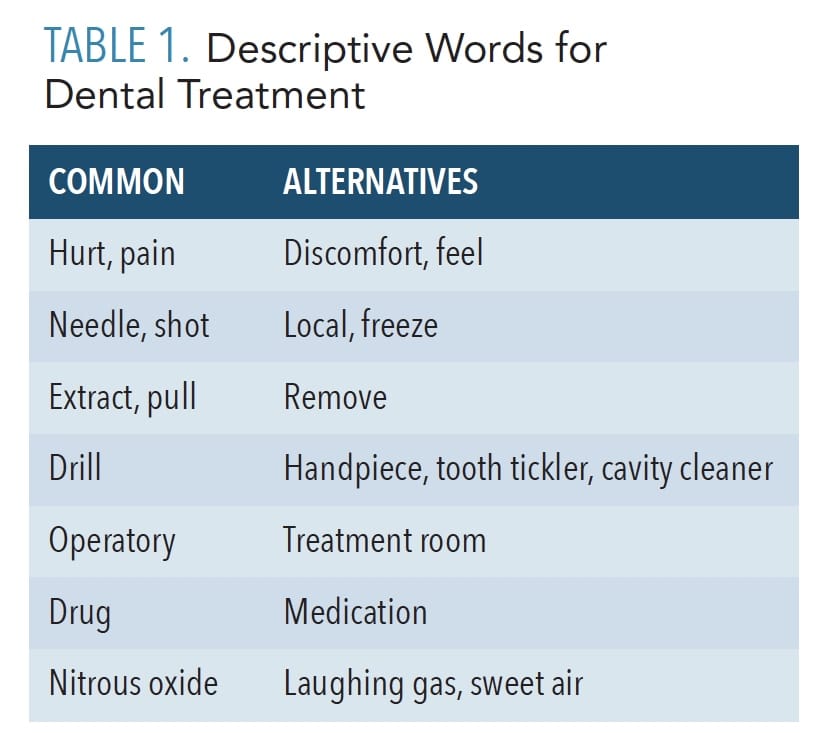 Before the merits and techniques of therapeutic hypnosis are introduced to patients, the entire dental team should be mindful of the importance of effective communication. The language used clinically can be intimidating for patients, especially those with dental anxiety. The thoughtful substitutions of words used to describe treatment can help alleviate such fear (Table 1). Through these processes, effective communication can create a climate of trust.
Before the merits and techniques of therapeutic hypnosis are introduced to patients, the entire dental team should be mindful of the importance of effective communication. The language used clinically can be intimidating for patients, especially those with dental anxiety. The thoughtful substitutions of words used to describe treatment can help alleviate such fear (Table 1). Through these processes, effective communication can create a climate of trust.
A prominent goal for all iatrosedation techniques and euphemistic language is to eliminate or reduce the patient’s need for pharmacologic intervention. Although there are proven benefits with pharmacologic supplementation, disadvantages include patient compliance, prolonged latent period, incomplete drug absorption, inability to titrate, and prolonged duration.5
MYTHS SURROUNDING HYPNOSIS
When introducing hypnotherapy to patients, oral health professionals should demystify the negative emotions and images associated with hypnotic techniques. Educating the patient about the truths of therapeutic hypnosis should be done early in the appointment to dispel fear and build trust.
First, it is important to realize that all hypnosis is considered self-hypnosis, and everyone can be hypnotized to some degree.18 The hypnotherapist is only acting as a guide or teacher during the session.18 The patient is always in control and can end a session at will. Even in the deepest trance, a patient will disengage from the trance once a sleep cycle has been initiated and ended. Another key point is that a patient cannot be forced to do or say something that he/she does not wish to. Educating the patient at the introductory appointment will help the individual realize that a therapeutic alliance can be formed.
THE HYPNOSIS PROCESS
The inclusion of rapid induction techniques can help minimize the time required for hypnotherapy. With rapid induction techniques, a patient may be induced in less than 3 minutes. To further enhance the experience, the entire dental team should be educated on the principles of hypnosis in order to support its incorporation into patient care. Team members need to be aware of how hypnosis can help treatment, how they can explain hypnosis to patients, and how the patient may act during a procedure.
The hypnosis process typically consists of explaining the merits of hypnosis and securing the patient’s permission; hypnotic induction; therapeutic utilization; and, finally, disengagement or reorientation to the environment.
Explaining Merits and Securing Permission. In addition to addressing misconceptions, the oral health professional should explain the merits of hypnotherapy, such as diminished need for pharmaceuticals; benefit of a therapeutic alliance with the provider; and the realization that hypnosis places patients in control over their anxieties, fears, and habits. Informed consent must be obtained, and should include consent to undergo hypnotherapy, as well as permission for the provider to use appropriate touching to deepen a trance.
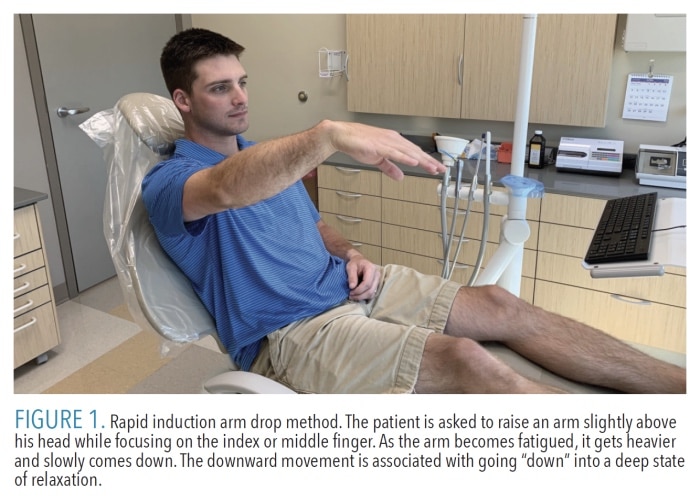
Hypnotic Induction. There are likely hundreds of ways to begin a formal induction with a patient. Besides traditional techniques (like the famous swinging pocket watch), therapists may use more modern rapid induction methods, such as the arm/hand pull or drop method (Figure 1). Regardless of the induction method used, the goal is to influence the areas of the brain responsible for associated behaviors, while allowing the patient to “let go.” This is best done by having some form of muscle tension buildup, followed by tension release. The most practical and timesaving method in the dental office is the eye-roll countdown technique. In this method, the patient is told to keep his or her eyes wide open and roll them up as high as possible. The patient is distracted by using a tapping method with a forefinger on top of the patient’s head, combined with a countdown from five to one. After the countdown, the patient will close the eyelids and “let go.”4
Therapeutic Utilization. Because successful induction will automatically relax the patient, it is usually unnecessary to incorporate specific fear-reduction scripts into the session. If the patient still seems nervous or tense, however, the provider may suggest that he or she go to a happy place while actual treatment begins. Every patient’s happy place is personal and can be achieved with the help of guided imagery. Once the patient is in a trance (often confirmed with rapid eye movement beneath the eyelids), other therapies may be incorporated based on need. These include anesthesia, pain control, management of edema or bleeding, and any of the aforementioned uses.2,4,5,19
There may be circumstances where scripts are helpful, as written instructions, scenarios, and use of metaphors can increase confidence between patients and providers.19 A common therapeutic script used in dentistry revolves around a computer programming metaphor.19 This metaphor serves to help the patient program out all pain-related behaviors, while programming in behaviors associated with comfort and control.19
Another popular therapeutic script is the iced hand. This involves suggesting the patient envision his or her hand being submerged repeatedly in ice water or snow.19 This will eventually restrict blood flow to the hand and alter the need for anesthesia.19 This intense cold or numbness is exaggerated to the fingertip, and whatever that fingertip touches will consequently freeze or become numb. This is helpful in anesthetizing soft tissue or as a substitution for topical anesthetic in preparation for an injection.19
Disengagement and Reorientation. After treatment is complete, disengaging the hypnosis session is best accomplished by using the reverse method of induction.4 If counting down from five to one was used to induce, counting up from one to five is a quick and easy method to disengage the session. Following disengagement, the patient is usually relaxed and can easily be reoriented to his or her environment. Although rare, some patients may experience time distortion. Others may not feel any change whatsoever, or may not be able to put the experience into words.
CONSIDERATIONS FOR USE
Provided it falls within their scope of practice, hypnosis may be used by licensed oral health professionals. Some dental schools include the principles of hypnodontics in their pain control curricula.5 However, most oral health professionals will need to pursue additional training to become comfortable using hypnosis as a safe and effective alternative for patient management. Organizations such as the American Society of Clinical Hypnosis and Society of Clinical and Experimental Hypnosis offer additional training for licensed professionals, including workshops, e-learning, consultation, ethics, and independent practice.20,21
Although certification may not be required, patients should be informed about the provider’s academic and clinical training in this field. According to the American Society of Clinical Hypnosis, most areas have a state or local professional society that can be contacted to vet qualified professionals who are competent to use hypnotherapy.22 Furthermore, patients should be proactive in educating themselves about hypnosis and its application in dentistry.
The potential difficulties that arise with the use of hypnosis—regardless of the profession or procedure—often result from a lack of formal education and not knowing one’s limits when providing therapeutic interventions.4 This is not unique to hypnosis. As with any practice, dental professionals must recognize the legal and ethical implications that could arise from engaging in hypnotherapy without merit.
![hypnotherapy figure 1. Patient in chair with arm raised]() POTENTIAL CONCERNS
POTENTIAL CONCERNS
As with any technique in dentistry, there are potential concerns with hypnotherapy, especially when misapplied. These include spontaneous regression (patient regressing to when fear was prevalent); abreactions (experiencing unpredictable emotions); symptom substitutions (experiencing anesthesia in an area not anesthetized); confabulations (imagining that something took place in the dental office that did not occur); and failure to remove suggestions (eg, patient may continue to feel numb in an area).4 For most of these concerns, re-inducing and disengaging the patient resolves the issue. Confabulations can be minimized or eliminated by having a witness in the treatment room or an authorized video recording of the treatment. Additionally, informed consent should be part of every hypnosis experience to further reduce undesirable effects, such as confabulations.
After successful hypnosis treatment, patients inevitably want to know more about the process. They may ask about nondental uses of hypnosis, such as chronic pain management, ego strengthening, or addressing sexual dysfunction or addiction disorders. Dental team members must properly refer patients to external resources for treatments outside of their scope of practice.
Contraindications to hypnotherapy involve patients who are unable to maintain concentration long enough to be induced or move to a trance-like state, such as patients with severe psychiatric or psychotic disorders or cognitive difficulties.
CONCLUSION
Hypnosis has many beneficial uses within the dental setting. When done within the proper context—and with appropriate education and training—hypnotherapy can be a valuable adjunct to traditional methods of patient management. Oral health professionals, including dental hygienists, can be trained in different levels of hypnosis techniques. Learning these techniques and using them as part of the provider’s treatment toolbox may enhance overall patient comfort, while reducing fear and providing alternative methods of behavior modification.
In order for hypnosis to gain greater acceptance within dentistry, outlets for increasing training must be created. This can be accomplished through dental and dental hygiene curricula design, continuing education opportunities, and professional organizations within this field. Oral health professionals may also have the opportunity to partner with a licensed hypnotherapist to provide hypnosis for their patients. Dental team members must build on their current skill sets and explore alternative methods—such as hypnotherapy—to positively influence patient behaviors that ultimately impact oral health.
Acknowledgement: The authors would like to thank Julie H. Schiavo, MLIS, AHIP, and Michael Austin White for their assistance with this manuscript.
References
- Abdeshahi SK, Hashemipour MA, Mesgarzadeh V, Shahidi Payam A, HalaJ Monfared A. Effect of hypnosis on induction of local anaesthesia, pain perception, control of haemorrhage and anxiety during extraction of third molars: A case-control study. J Craniomaxillofac Surg. 2013;41:310–315.
- American Society of Clinical Hypnosis. Hypnosis in Psychotherapy and Behavioral Medicine. Available at: asch.net/Public/GeneralInfoOnHypnosis/UsesOfHypnosisInDentistry.aspx. Accessed September 3, 2020.
- Lynn S, Rhue J. Theories of Hypnosis: Current Models and Perspectives. New York: Guilford Press; 1991.
- Yapko MD. Trancework: An Introduction to the Practice of Clinical Hypnosis. 3rd ed. New York: Brunner-Routledge; 2003.
- Malamed S. Sedation: A Guide to Patient Management. 6th ed. St. Louis: Elsevier; 2017.
- Patel B, Potter C, Mellor AC. The use of hypnosis in dentistry: a review. Dent Update. 2000;27:198–202.
- Rohmetra A, Tandon R, Singh K, Jaiswal A. Acupressure therapy in orthodontics: A review. Int J Orthod Rehabil. 2017;8:26–30.
- Wang SM, Kain ZN. Auricular acupuncture: a potential treatment for anxiety. Anesth Analg. 2001;92:548–553.
- Wang SM, Peloquin C, Kain ZN. The use of auricular acupuncture to reduce preoperative anxiety. Anesth Analg. 2001;93:1178–1180.
- Zijlstra FJ, van den Berg-de Lange I, Huygen FJ, Klein J. Anti-inflammatory actions of acupuncture. Mediators Inflamm. 2003;12:59–69.
- Naik PN, Kiran RA, Yalamanchal S, Kumar VA, Goli S, Vashist N. Acupuncture: An alternative therapy in dentistry and its possible applications. Med Acupunct. 2014;26:308–314.
- Fang J, Jin Z, Wang Y, et al. The salient characteristics of the central effects of acupuncture needling: Limbic-paralimbic-neocortical network modulation. Hum Brain Mapp. 2009;30:1196–1206.
- Jimson S, Malathi L, Devi GN, Sankari SL. Aromatherapy in dentistry—a review. Biomed Pharmacol J. 2016;9:827–828.
- Ramar K, Hariharavel VP, Sinnaduri G, Sambath G, Zohni F, Alagu PJ. Effect of audioanalgesia in 6- to 12-year-old children during dental treatment procedure. J Contemp Dent Pract. 2016;17:1013–1015.
- Foundation for Peripheral Neuropathy. Biofeedback Therapy. Available at: foundationforpn.org/living-well/integrative-therapies/biofeedback-therapy/. Accessed September 3, 2020.
- Angelo Z, Polyvios C. Alternative practices of achieving anaesthesia for dental procedures: a review. J Dent Anesth Pain Med. 2018;18:79–88.
- Munshi AK, Hegde AM, Girdhar D. Clinical evaluation of electronic dental anesthesia for various procedures in pediatric dentistry. J Clin Pediatr Dent. 2000;24:199–204.
- Goldberg B. Self Hypnosis: Easy Ways to Hypnotize Your Problems Away. Franklin Lakes, New Jersey: Career Press; 2006:13–34.
- Garver RB. Chronic pain syndrome. In: Hammond DC, ed. Hypnotic Suggestions and Metaphors. New York: Norton; 1990.
- American Society of Clinical Hypnosis. ASCH Certification Program. Available at: asch.net/Certification/CertificationUpdate.aspx. Accessed September 3, 2020.
- Society for Clinical and Experimental Hypnosis. SCEH Certification Programs. Available at: sceh.us/certification. Accessed September 3, 2020.
- American Society of Clinical Hypnosis. Selecting a Qualified Professional. Available at: asch.net/Public/GeneralInfoOnHypnosis/SelectingaQualifiedProfessional.aspx. Accessed September 3, 2020.
From Dimensions of Dental Hygiene. October 2020;18(9):26-28, 31.