
Safely Easing the Pain
John A. Yagiela, DDS, PhD, shares his expertise on the use of topical anesthetics.
Q. How are topically applied anesthetic agents effective?
A. The nerve fibers that carry painful sensations from the soft tissues have free nerve endings in the mucosa. The topical anesthetic reaches these nerve endings and renders them insensible to stimuli. Some studies have shown that high concentration agents, when used for an extended periodof time, may cause some pulpal anesthesia.1,2
Q. What application methods are available with topical anesthetics?
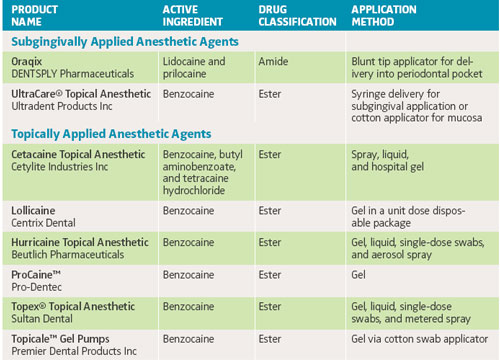
A. Lidocaine and benzocaine product formulations come in liquids, sprays, ointments, gels, lozenges, and single-dose swabs, as well as patches. New subgingivally applied products are inserted into the sulcus or periodontal pocket.
Q. Are some topical anesthetic products a combination of anesthetic drugs?
A. Benzocaine can be mixed with other ingredients, such as butamben and tetracaine hydrochloride. Here the benzocaine produces a quick onset whereas the tetracaine may improve the anesthetic effect and extend the duration of action. Tetracaine is very lipid soluble and is absorbed into local tissues very readily, causing a deeper penetration and a stronger effect. Lidocaine is also available in combination with prilocaine. This mixture can form a very high concentration agent in liquid form.
Q. When using topical anesthetics, how long is the duration of action?
A. The duration of action ranges between 5 and 40 minutes, depending on the exact formulation and delivery method. Duration can also depend on how exposed the anesthetic is to oral fluids that tend to wash it away. For drug products, such as the lidocaine patch, that provide a steady, continuous anesthetic uptake for some time, the longer they are kept on the tissue, the stronger the effect may become.
Q. Are there any contraindications to reapplication of topicals?
A. Published maximum dosage recommendations do not exist for most benzocaineproducts in adults.3 Benzocaine tends not to get absorbed into the blood stream. Swallowed benzocaine gets metabolized very quickly. Therefore, systemic toxicity doesn’t really exist with the normal use of benzocaine in the dental setting.
Lidocaine ointment usually has a low absorption rate. Most of it gets washed away and swallowed. Once it gets into the stomach, the drug is usually metabolized before it can reach the systemic circulation. However, if lidocaine is spread over a wide area, then absorption can be fairly rapid, particularly if it is inhaled. This is why the topical dosing of lidocaine is similar to that for injection, eg, in adults: 250 mg lidocaine base in ointment form, 4.5 mg/kg up to 300 mg lidocaine hydrochloride in topical solution. Subgingivally applied topicals do not cover broad surface areas, so the risk of toxicity is low. Sprayed-on topical anesthetics reach broad surface areas and are useful for numbing large areas and suppressing the gag reflex prior to procedures such as x-rays. A metered spray device is advised to avoid overdose. The agent can be reapplied if the total dosage is within maximum recommended limits or sufficient time has passed for the first dose to be eliminated from the blood stream.
Q. How can we identify symptoms of overdose?
A. Systemic toxicity creates a mixture of excitatory and depressive effects. Some patients may feel sedated, yawn, or have difficulty staying awake. With larger doses, excitatory symptoms may also be exhibited like agitation and hand tremor. Toxic overdoses can lead to seizure activity, unconsciousness, and respiratory arrest.
Q. What can hygienists do to guard against the risk of overdose?
A. To ensure safety, try to keep the agent on the tissue to which it was applied. Use it one quadrant at a time and when you think the drug has worked, remove the remaining agent and go on to the next quadrant. This allows the drug to be absorbed more slowly and in lower amounts.
Q. Are allergic reactions to topical anesthetics common?
A. Allergy is almost unheard of with a topical amide preparation. Almost all patients who have been diagnosed as allergic to these drugs are not truly allergic. They typically exhibit a fear reaction to the anticipation of the local anesthesia injection that gets misinterpreted. Fear responses are not usually observed with the application of a topical agent but they might happen in someone who is fearful of hygiene procedures. Benzocaine and tetracaine are esters, which have an increased potential for allergic reactions. Although absorption is slow when compared to giving a drug by injection, the possibility of anaphylaxis theoretically exists.
Anaphylaxis is an immediate and most serious type of allergic reaction. Symptoms include nausea, vomiting, and a rash (called urticaria) that consists of raised, itchy areas on the skin. The rash can appear all over the body because the reaction is a systemic effect. There may be swelling of tissues where fluid can accumulate, such as the eyelids, lips, and throat. Bronchial spasm is common in anaphylaxis. The heart rate may also increase and blood pressure decrease as fluid moves out of leaky blood vessels into the surrounding tissues. Anaphylaxis is very rare with topicals. Delayed reactions are more likely, but you won’t normally see those reactions in the dental office. These allergic reactions are usually cell-mediated allergic reactions, versus the humeral antibody etiology of anaphylaxis. Delayed reactions like eczema develop several days after drug administration, usually in the area of application.
REFERENCES
- Brook IM, Tucker GT, Tuckley EC, Boyes RN. A lignocaine patch for dental analgesia safety and early pharmacology. J Control Release. 1989;10:183–188.
- Vickers ER, Punnia-Moorthy A. Pulpal anesthesia from an application of a eutectic topical anesthetic. Quintessence Int. 1993;24:547–551.
- Yagiela JA. Injectable and topical local anesthetics. In Ciancio SG, ed. ADA Guide to Dental Therapeutics. 3rd ed. Chicago: ADA Publishing Co; 2003.
From Dimensions of Dental Hygiene. May 2005;3(5):20, 22.

