Strategies to Prevent Implant Complications
Dental implants are becoming more standard in replacing single or multiple teeth and are a predictable way of maintaining a healthy smile.

Standard of Care in Supporting Implant Health
Dental implants are becoming more standard in replacing single or multiple teeth and are a predictable way of maintaining a healthy smile. Placement has become more predictable with routine use of cone-beam computed tomography and bone augmentation. Peri-implant care is becoming more common and requires the clinician and patient to maintain periodontal health for long-term success. Functional success of a dental implant includes that it has no mobility, absence of bleeding on probing, lack of peri-implant bone loss, and a probing depth < 5 mm. To increase longevity, the early signs and symptoms of peri-implant disease must be noted.
Photo Credit: Bet_Noire / iStock / Getty Images Plus
Implant Complications
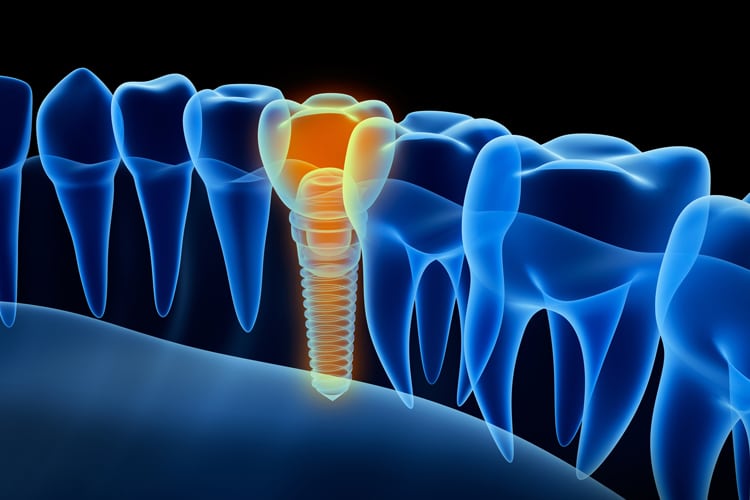
Peri-implant disease has two manifestations: peri-implant mucositis and peri-implantitis. In December 2017, the Proceedings of the World Workshop on Classification of Periodontal and Peri-Implant Diseases and Conditions were released. These definitions describe diagnostic criteria of implant disease. Peri-implant mucositis is inflammation in the surrounding gingival tissue with no signs of loss of supporting bone following initial placement. Peri-implantitis is a plaque-associated inflammatory disease occurring around a dental implant. Clinical signs of peri-implantitis are inflammation of the mucosa surrounding the dental implant and progressive bone loss.
Photo Credit: Talaj / iStock / Getty Images Plus

Assessment
Assessment of the dental implant is an essential part of the dental hygiene care plan. Clinical signs of inflammation must be included in evaluating the implant at each appointment. Early detection of inflammatory disease is the best method for prevention and contributes to successful outcomes. Any redness, enlarged tissue, and suppuration should be noted and seen as a sign of peri-implant disease. Mobility of a dental implant is considered a failed implant, as the threads should be osseointegrated, which does not allow for any movement. The presence of biofilm and calculus accumulation needs to be noted. Biofilm indicates high risk for an inflammatory reaction and must be removed.
Photo Credit: RyanKing999 / iStock / Getty Images Plus

Determine Disease Risk
Determining disease risk is an integral part of the assessment phase. No absolute list of risks has been developed. There is some evidence that several physical and medical conditions affect peri-implant disease. Outcomes of the risk assessment will help determine individual supportive care. The goal of treatment should be longevity of the implant. Understanding the risks involved with disease progression is integral to that process.
Photo Credit: Bet_Noire / iStock / Getty Images Plus
Treatment Plan
Assessment of the dental implant will determine the nonsurgical treatment choices. Peri-implant mucositis can be treated successfully, while peri-implantitis treated nonsurgically has limited effectiveness. At the first sign of inflammation, treatment should be initiated. The main goal of nonsurgical therapy is to eliminate inflammation through the removal of calculus and biofilm. Any sign of inflammation should be treated quickly, as the risk of peri-implantitis is great in the presence of inflammation. A treatment plan must be tailored to the individual patient. There is no standardized protocol for nonsurgical treatment of peri-implant disease, yet all assessments should be considered when treatment is initiated.
Photo Credit: alex-mit / iStock / Getty Images Plus

Implant Maintenance
Improved outcomes are associated with supportive care every 3 months to 6 months. Supportive care appointments include clinical assessment of the implant, professional removal of biofilm and calculus, and individualized self-care for the implant. The implant should be assessed every 3 months in the first year and then adjusted according to patient needs. Preventing peri-implantitis is key. Long-term success is dependent on the health of the supporting peri-implant tissues.

