Relationship Between Oral and Heart Health
Over the past 25 years, it has become apparent that oral infections/inflammation processes are associated with systemic diseases or pathologic conditions, but clear-cut causative mechanisms have not yet been established.

Over the past 25 years, it has become apparent that oral infections/inflammation processes are associated with systemic diseases or pathologic conditions, but clear-cut causative mechanisms have not yet been established. The most common oral infections/inflammatory processes are gingivitis, periodontitis, and periapical periodontitis. In particular, chronic periodontitis has been linked to atherosclerotic cardiovascular diseases (ACVD).
Photo Credit: fruttipics/ISTOCK/GETTY IMAGES PLUS

What the Evidence Says
The association between periodontitis and ACVD prompted the editors of the American Journal of Cardiology and the Journal of Periodontology in 2009 to publish an editors’ consensus that the two diseases were linked, but that the mechanisms behind this association were unknown. Updated reviews and a joint European-American workshop concluded in 2013 came to the same conclusion. So while the two conditions are clearly associated and the epidemiological evidence shows that periodontitis always precedes ACVD events, there is insufficient evidence on a causative role of periodontitis for ACVD.
Photo Credit: PeopleImages/E+
Causative Relationship
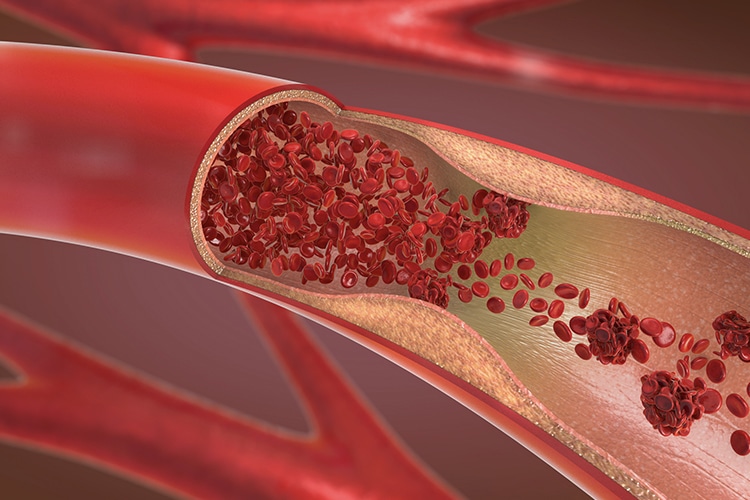
The possible causative relationship between periodontitis and ACVD is based on the fact that the inflamed periodontal pocket epithelium forms an open wound, creating a port of entry for subgingival and oral bacteria to enter the bloodstream. A healthy and intact periodontal ligament has an estimated surface area of 31 square inches to 35 square inches. The wound surface, or periodontal inflamed surface area, among individuals with periodontitis is estimated to be as large as 2 square inches to 8 square inches. In fact, the presence of daily occurring, short-lived bacteremias has been reported in many studies. Oral bacteria have been found after toothbrushing and after eating, but also spontaneously in periodontitis patients. Oral and periodontal bacteria have also been found in atherosclerotic lesions and arterial biopsies. The hypothesis is that these microorganisms in the systemic circulation may have a variety of effects, which may play a causative role in the pathophysiology of ACVD.
Photo Credit: Christoph Burgstedt/ISTOCK/GETTY IMAGES PLUS

Pro-Inflammatory Markers
The presence of a consistent pro-inflammatory state among individuals with periodontitis is another factor currently being investigated. The most studied biomarker for the pro-inflammatory state is C-reactive protein (CRP), an acute phase protein generated in the liver in response to bacterial infection and other pro-inflammatory mediators. These biomarkers must currently be regarded as “surrogate” markers for ACVD and whether they have a causative role or just “reporter” function is currently not clear. Originally, levels of CRP greater than 2.1 mg/L may have increased the risk for an ACVD event; more recent publications show levels >3 mg/L. Therefore, this pro-inflammatory state may play a role in the link between periodontitis and ACVD.
Photo Credit: Nerthuz/ISTOCK/GETTY IMAGES PLUS

Role of Inflammation
Yet another explanatory mechanism could be related to a prothrombotic state in periodontitis. Coagulation factors are normally generated in the liver, but, in periodontitis, increased levels of these coagulation factors are present. This may result in a pro-thrombotic state, increasing the risk for ischemic events. Inflammation in general, as well as bacteremia, can trigger dyslipidemia (abnormal amount of lipids in the blood). In periodontitis, an aberrant lipid metabolism can occur, elevating levels of low-density cholesterol and reducing levels of high-density cholesterol. This imbalance between the “bad” and “good” cholesterol commonly occurs in patients with ACVD and is widely prevented with medication.
Photo Credit: Mutlu Kurtbas/E+

Effects of Treatment
Given the associations of arterial stiffness and endothelial dysfunction with periodontitis, the question of whether cardiovascular health is improved after treatment of periodontitis must be asked. In other words, are there changes in the levels of endothelial dysfunction or arterial stiffness after basic periodontal therapy (scaling and root planing)? The body of evidence is small, but, in general, studies have shown that patients with periodontitis who receive nonsurgical periodontal therapy experience improvement in arterial function and/or reduced severity of atherosclerosis. Individuals with periodontitis should undergo periodontal therapy to improve their cardiovascular risk profile, thereby possibly reducing the risk of ACVD events. Additionally, dental professionals should discuss ACVD risk factors with their patients as part of their periodontal treatment protocol.

