The Role of Implants in Maintaining Oral Health
Dental hygienists need to understand the role dental implant fixtures play in the overall health and quality of life for patients.

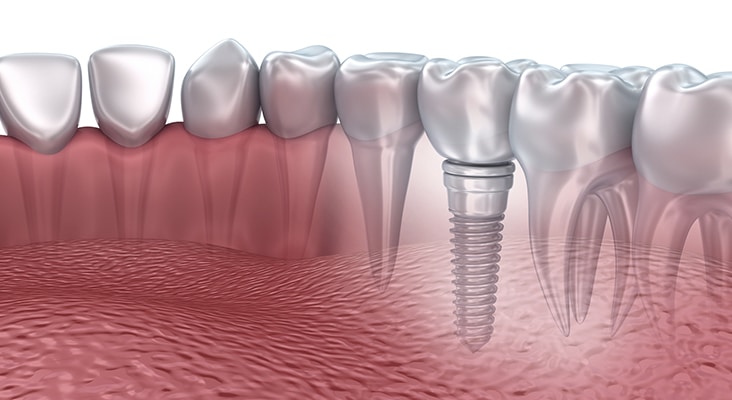
Dental hygienists need to understand the role dental implant fixtures play in the overall health and quality of life for patients. Endosseous, or endosteal, dental implants are screw-shaped, placed into the maxilla or mandible, and function as a tooth root to be restored with a crown, achieving the look and feel of natural tooth replacement. In addition to replacement of one or more teeth, dental implants also provide support for fixed or removable prostheses, with restorations that can be screw retained, cement retained, or a combination of both. The risk of bone loss in the mandible increases with the amount of time a tooth is missing, therefore, dental implants are also important for alveolar ridge preservation. Dental implant placement is an important consideration for daily function, proper occlusion, speech, mastication, nutrition, facial shape, quality of life, and overall health and well-being.
Photo Credit: sujit kantakad / iStock / Getty Images Plus

Implant Maintenance
Dental hygienists play an integral role in the early detection of dental implant diseases and providing individualized patient care in the maintenance protocol. Despite the high survival rate for dental implants—96.33%—the risk for complications remains possible. Dental hygienists must be equipped to provide treatment in all aspects of dental implant placement including the healing phase, surgical, prosthetic, and maintenance periods. Research suggests that ongoing dental hygiene care, both professional and patient-driven, is essential in efforts to prevent implant failure and irreversible destruction.
Photo Credit: AlessandroPhoto / iStock / Getty Images Plus

Biofilm Removal
Professional dental hygiene care includes the removal of biofilm and calculus at each maintenance visit, while avoiding implant abutment damage as much as possible. In an effort to reduce such bacterial load, studies have suggested that the hardness of the scaler tip may prove to be more detrimental than the actual application method itself. It is widely accepted that local debridement of implants be performed with instruments that are softer than titanium. However, a study by Huang et al9 tested the abilities of instruments to alter both titanium and zirconia implant abutment surfaces and then looked at bacterial adhesion. They concluded that the use of a titanium curet led to deep linear carving marks in titanium abutments, allowing for significant surface changes, increased abutment roughness, and higher optical density of adhered bacteria. The authors suggested that titanium curets be used with care on titanium abutments. Conventional metal, such as stainless steel, remains contraindicated for use with implants, as more surface damage creates ideal niches for biofilm accumulation and bacterial adhesion. Studies suggest these instruments allow for contamination of the titanium implant surface with other metal ions over time, therefore, are contraindicated for regular therapeutic use. Plastic scalers, although safe on implant surfaces, have poor cleaning properties and may leave fragments. Plastic instruments reinforced with graphite and gold-plated curets have been suggested, however, they may breakdown.
Photo Credit: Milos Dimic / E+
xxxxx
Periodontal Probing
Periodontal probing is an assessment tool for evaluating peri-implant tissues; however, current studies suggest that less force exertion must be exercised. Gulati et al found that junctional epithelial attachment zones differ in their strength attachment to the implant as compared to a natural tooth. Periodontal probing—using a metal or plastic probe—may be helpful in peri-implant assessment and should be performed at maintenance appointments using light pressure; however, Gulati et al suggest it should be avoided during the first 3 months after abutment connection to assure proper healing and establishment of the soft tissue seal. Research concludes that progressively deepening probing depths and bleeding on probing may be more significant than solely using probing depth values of ≥ 4 mm or 5 mm. As such, documentation is fundamental from baseline (when possible) through each maintenance visit.
Photo Credit: AlessandroPhoto / iStock / Getty Images Plus
Implant Failure
Dental implant failure has two stages: early and late. Early failure occurs within the first few weeks to months, consisting of bone necrosis, bacterial infection, initial inadequate stabilization, surgical trauma, early occlusal load, and properties within the host tissue. Late failure occurs subsequently and can arise due to functional loading and infection resulting from pathological processes. Even after a dental implant has osseointegrated, a number of variables can contribute to implant failure. A break in osseointegration can result from an etiological factor and lead to a late failure. A severe inflammatory reaction can occur rapidly in the presence of a foreign body invasion, like that of excess residual cement from placement of the prosthetic crown. Exploration and radiographic surveys can aid in the detection of excess residual cement, although only certain types of cements are visible radiographically.
Photo Credit: alex-mit / iStock / Getty Images Plus

Periodontal Assessment
Routine assessment of peri-implant tissue changes and mechanical biofilm removal with the use of appropriate armamentarium that will avoid damage to abutment surfaces are key to implant health. Reinforcing proper oral hygiene instruction and self-care regimens are essential. Continual reinforcement of tobacco cessation must be included in patient education as smoking weakens bone structure and inhibits the initial healing process. Clinical assessment of bleeding, inflammation, mobility, probing comparisons, and inquiry regarding pain or daily complications will help the assessment process, as well as radiographic assessment.
Photo Credit: baona / iStock / Getty Images Plus

Oral Hygiene
Oral hygiene instruction should include interproximal brushes and cleaners, end-tufted brushes, water flossers, soft manual toothbrushes and gentle power brushes, floss, and threader floss. Some of these aids may leave behind residue, therefore, careful mechanical demonstration and instruction are crucial. The use of a rubber tip stimulator can aid in mechanical biofilm removal. During implant healing stages, chemotherapeutic agents, such as chlorhexidine 0.12%, have been recommended as a mouthrinse or carefully applied to the area with a cotton tip applicator when mechanical removal is temporarily contraindicated.

