Controlling the Immune Response That Causes Periodontal Diseases
Periodontal diseases are related to an immunoinflammatory response to various types of oral biofilm. They affect approximately 42% of United States adults. Chronic periodontitis is characterized by alveolar bone loss, attachment loss, and apical migration of the junctional epithelium. Periodontal diseases result from dysbiosis: an imbalance between different organisms present in the natural microbiota of the subgingival microenvironment. Periodontal destruction can be attributed to the interaction of two main players: periodontally pathogenic biofilm and the host-mediated immunoinflammatory response to that biofilm. Current treatment guidelines for periodontitis include the physical removal of plaque biofilm and calculus by scaling and root planing. While this treatment aims to eliminate the bacterial insult, scaling and root planing does not address the host response element of periodontal diseases.
Inflammation is the body’s initial response to various types of injury via physical, bacterial, or chemical means, and is characterized by an increase in temperature, erythema, edema, pain, and loss of function.
 image_jungle / iStock / Getty Images Plus
image_jungle / iStock / Getty Images Plus
The development of periodontal diseases is initiated by a dysbiotic bacterial plaque insult and tissue destruction is propagated by the host immune response to the biofilm.
 red_moon_rise / E+
red_moon_rise / E+
Host modulation therapies are also used to treat which other chronic inflammatory diseases?
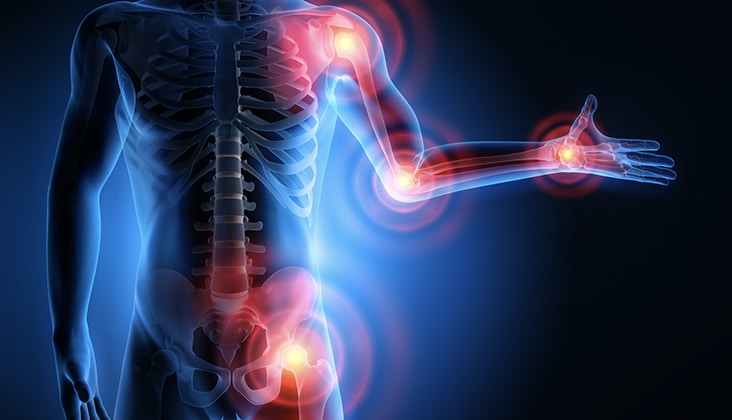 peterschreiber.media / iStock / Getty Images Plus
peterschreiber.media / iStock / Getty Images Plus
A variety of potential host-modulation therapies are available to treat periodontal diseases, including non-steroidal anti-inflammatory drugs, subantimicrobial-dose doxycycline (SDD), bisphosphonates, and cytokine inhibitors.
 sittithat tangwitthayaphum / iStock / Getty Images Plus
sittithat tangwitthayaphum / iStock / Getty Images Plus
Bisphosphonates are bone-sparing agents that modify the host response by disrupting osteoclastic activity, which inhibits bone resorption.
 Goldfinch4ever / iStock / Getty Images Plus
Goldfinch4ever / iStock / Getty Images Plus
SDD is one of many United States Food and Drug Administration-approved host modulation therapies for periodontitis.
 Fahroni / iStock / Getty Images Plus
Fahroni / iStock / Getty Images Plus
Share your Results:

