Caring for Patients With Heart Disease
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in the United States, claiming about 2,200 deaths daily or one death every 40 seconds. Globally, CVDs accounted for more than 17 million deaths, representing over 30% of all causes worldwide in 2015.

Cardiovascular Disease Prevalence
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in the United States, claiming about 2,200 deaths daily or one death every 40 seconds. Globally, CVDs accounted for more than 17 million deaths, representing over 30% of all causes worldwide in 2015. CVD encompasses a broad group of diseases and conditions, including coronary artery disease, cerebrovascular disease and stroke, heart failure, high blood pressure, disorders of the heart rhythm, peripheral artery disease, venous thromboembolism, valvular disorders, and congenital heart defects. An estimated 92.1 million US adults have at least one type of CVD, with coronary artery disease being the most common. CVD and stroke are the most costly diseases, accounting for 14% of total health expenditures in 2012 and projected to nearly triple to $918 billion by 2030, when it is estimated that 43.9% of the US population will have some form of CVD. However, the mortality attributable to CVD, which was steadily increasing until the 1980s, has since declined.
Photo Credit: PIKSEL / iStock / Getty Images Plus

Medical History
The medical history intake process requires careful consideration of the implications of conditions reported and medications taken. This analysis is complicated by the fact that many cardiovascular medications are taken for more than one indication. Additionally, cardiovascular conditions may be managed by several medications working synergistically to achieve the therapeutic effect. Even patients who dutifully take all medications according to their prescribed schedule and dosage may be variable in their knowledge of their conditions and the possible impact on dental treatment. Medication compliance, even following discharge for acute coronary events, has been historically disappointing, and sometimes deficient. Oral health professionals need to remain familiar with continuously updated CVD treatment guidelines, as they can have life-altering impact on patient health and can help to ensure safe treatment.
Photo Credit: VectorCookies / iStock / Getty Images Plus
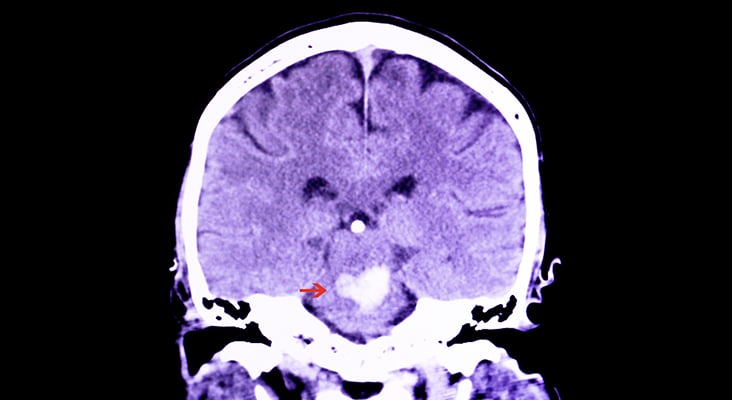
Acute Coronary Syndrome
Acute coronary syndrome is not a single disease, but rather describes a group of related higher risk conditions characterized by myocardial ischemia, which is a reduced flow of blood to the heart muscle caused by partial to full blockage of the coronary arteries. Although chronic heart conditions have similar and often co-occurring etiologies, acute coronary syndrome is distinguished by its acute nature and must be efficiently diagnosed by a medical professional as a potentially fatal risk. Symptoms include burning with radiation to jaw and left arm, but research suggests that, especially in older women, these signs may be more subtle, and include nausea, vomiting, and breathlessness. Getting a patient into emergency care is suggested when there is any suspicion of acute cardiac events.
Photo Credit: 7activestudio / iStock / Getty Images Plus
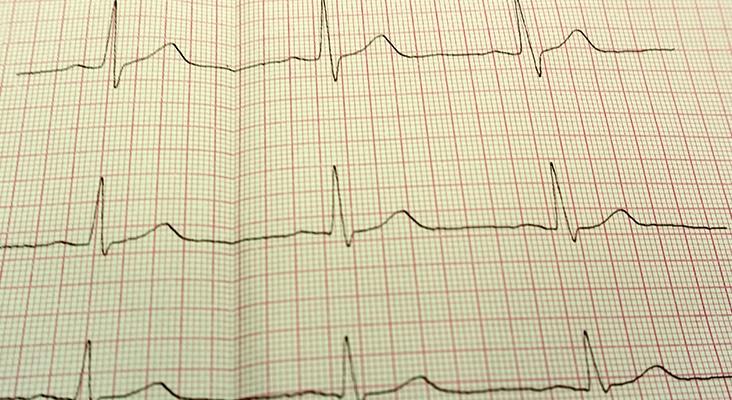
Atrial Fibrillation
Atrial fibrillation is the most common form of all cardiac arrhythmias, affecting more than 33 million people worldwide, with the highest concentration in North America. Individuals with atrial fibrillation are five times more likely to experience stroke, the second leading cause of death after heart disease worldwide. It is associated with risk for other CVDs, such as hypertension, heart failure, and acute coronary syndrome. Several categories of advancing disease states, which reflect the frequency and degree of aberration from normal heart rhythm and function, contribute to the level of morbidity and mortality risk for patients, the most serious of which is stroke.
Photo Credit: Vitaly Faritovich / iStock / Getty Images Plus

Percutaneous Coronary Intervention
Percutaneous coronary intervention (PCI) first introduced in the 1990s, has revolutionized the treatment of coronary artery disease and is now among the most commonly performed medical procedures. An estimated 492,000 patients underwent PCI in the US in 2010. The goal of this intervention is to widen the lumen of a coronary artery that is occluded by intravascular deposits to some degree and to restore the blood flow to the cardiac tissue. Initially, this was accomplished by balloon angioplasty—a technique that uses a balloon catheter compressing the intravascular deposits and thus re-opening the vessel. Unfortunately, up to 50% of patients experienced restenosis, prompting the development of new techniques to improve patient outcomes. Introduction of bare metal stents, followed by the first and second-generation drug-eluting stents (DES), have progressively reduced complication rates and dramatically improved outcomes associated with percutaneous coronary angioplasty. The two types of complications associated with stents are stent thrombosis—development of a thrombus in the stented segment of the artery, and stent restenosis—narrowing of the vessel wall due to proliferation of the vascular tissue overgrowing the stent frame. While bare metal stents lowered the rate of stent thrombosis compared to balloon angioplasty, they also caused vessel injury and inflammation, leading to stent restenosis. DES were developed to overcome this complication by using anti-proliferative drugs. However, anti-proliferative drugs released by DES naturally slow the healing of the vascular wall post-PCI, and the incomplete endothelialization contributes to early (within 30 days post-PCI) or late (beyond 30 days post-PCI) stent thrombosis. The most important method of preventing this life-threatening complication is DAPT of appropriate duration.
Photo Credit: Andrei Orlov / iStock / Getty Images Plus
Dual Antiplatelet Therapy
Dual antiplatelet therapy (DAPT) is standard in management of acute coronary syndromes and post-PCI to prevent thromboembolic events that can lead to repeat myocardial infarction, stroke, and stent thrombosis with possible fatal outcomes. Use of aspirin (75 mg to 162 mg) and another antiplatelet agent that target different pathways of platelet activation, provides additive antiplatelet effect. Combination with clopidogrel is used most frequently, unless the patient has genetic polymorphisms for the hepatic cytochrome P450 enzymes that metabolize this drug to its active form and may derive less antiplatelet effect from clopidogrel as a result. Both prasugrel and ticagrelor are more potent than clopidogrel and provide a more intensive platelet inhibition, resulting in reduced risk of ischemic events; however, this is balanced by increased bleeding risk. Prasugrel is preferred in DAPT for the first year following acute coronary syndrome or stent implantation, but due to the high risk of intracranial bleeding, subsequent DAPT may be best provided with clopidogrel.
Photo Credit: Sopone Nawoot / iStock / Getty Images Plus
Triple Antithrombotic Therapy
Patients with atrial fibrillation, or another condition, such as prosthetic heart valves, deep vein thrombosis, or pulmonary embolism, that requires long-term oral anticoagulation are at high risk for stroke and ischemic events. About 30% of them also have a diagnosis of acute coronary syndrome or undergo PCI, which necessitates DAPT. These patients can be prescribed triple antithrombotic therapy (TATT), which combines an oral anticoagulant (most frequently warfarin) with DAPT. However, the therapeutic benefits of the TATT vs a double therapy of oral anticoagulant and clopidogrel, are not clear, as rates of thrombotic and thromboembolic events in patients on oral anticoagulant+clopidogrel alone did not differ from the group on TATT, showing no benefit of adding aspirin. At the same time, patients on TATT are at significantly higher risk for major bleeding, fatal in approximately one out of 10 bleeding events.

