The Evolution of Ultrasonic Therapy
Advancements in power driven instrumentation have strengthened its role in progressive periodontal therapy.
FOR GENERATIONS, clinicians have struggled with the definition of debridement and the devices used in the debridement process. O’Leary1 created the following terminology:
Scaling: Instrumentation to remove supragingival uncalcified and calcified accretions and all gross subgingival accretions.
Root Planing: Instrumentation to remove the microbial flora on the root surface or lying free in the pocket, all flecks of calculus, and all contaminated cementum and dentin.
After debridement is finished, the anticipated end result is that the sulcus is completely devoid of all irritants including plaque, calculus, endotoxin, and necrotic cementum. However, the primary protocol is the periodic removal or dissolution of an established biofilm.2 The question is what category of instrumentation—manual or mechanical—is the most effective in achieving periodontal health?
 |
Figure 1. Cavitation activity of ultrasonic tip with implosion of particulates. |
MANUAL VS MECHANICAL INSTRUMENTATION
The advent of power-driven instrumentation, both sonic and ultrasonic therapy, ushered in a new era for mechanical debridement. However, the acceptance of ultrasonic therapy in periodontal therapy has been fraught with controversy. The initial debate was over the potential damage to root surfaces with ultrasonic devices. Evidence demonstrated that this power (a magnetostrictive device at 18 kHz to 42 kHz) could create root roughness when compared to manual instrumentation. The tips used in these early devices were large in diameter and primarily for gross calculus removal.
However, even though studies demonstrated increased root roughness with these devices, the degree of inflammation was less when compared to manual instrumentation.3 A manual instrument decreases periodontal pathology through the mechanical removal of plaque and calculus and by detoxifying the root by decreasing the levels of endotoxin. An ultrasonic device possibly affects the microbial population through cavitation (Figure 1). Walmsley demonstrated that ultrasonic machines with water irrigation decreased the biomass by five to eight times versus no water irrigation.4 In addition, studies show that periodontal pathogens are negatively affected by ultrasonification.5
In the early 1980s, Holbrook suggested modifying ultrasonic tips to a decreased diameter. Since fabricating tips was a technique sensitive task, this action led to breakage and discomfort, especially when used in autotunable equipment. When manufacturers began producing tips with quality control and when tips were coordinated to specific generators, the use of ultrasonic therapy became more widely accepted, including implementation in academic settings (Figure 2).
Likewise, studies began to show positive effects of power-driven instrumentation. Dragoo demonstrated in an in vivo study that modified ultrasonic tips of decreased diameter were more effective than large diameter ultrasonic tips and that manual curets with the modified tips achieved root smoothness. 6
In a study of recare patients, Copulus showed that ultrasonic therapy maintained attachment levels compared to handheld curets with a significantly reduced timeframe.7 With instrumentation of furcations, Leon and Vogel suggested that ultrasonic tips were more effective than manual instrumentation in accessing class II and class III furcations.8 This is primarily because many curets have blade face widths that are larger than the apex width of most furcations. However, curets designed with mini-blades9 or manual diamond coated instruments can effectively access furcation anatomy. Hallmon’s and Rees’ review comparing mechanically driven instrumentation with manual instrumentation suggested that both are comparable in affecting improved clinical outcomes. The parameters included probing depths, clinical attachment levels, bleeding on probing, and recession.10 However, experienced clinicians appreciate the synergy that occurs when power-driven instrumentation and manual curets are used in conjunction with one another.
|
|
|
|
| Figure 2. Placement of a thin diameter
ultrasonic tip in a periodontal pocket. |
Figure 3. Comparison of Gracey 15/16,
11/12, 13/14 curets. All possess thin face widths. |
Figure 4. Similarities of shape and diameter for periodontal diagnostic instruments and ultrasonic tips. |
ADVANTAGES AND DISADVANTAGES
Adistinct advantage of power-driven instrumentation is decreased operator fatigue. Some authors suggest a decrease of approximately 25% in overall time with power-driven instrumentation compared to manual debridement.8
Recently, many manufacturers have developed handles made of silicone. The main advantage is the decreased repetitive motion and stress placed physically on the operator. With most power-driven instruments having tips cycling in a 25,000-30,000 kHz frequency, the mechanical action of the tip is disrupting calculus, thus leading to decreased physical stress and such conditions as carpal tunnel syndrome. Traditional finger rests, which were once exclusively intraoral, are now becoming more extraoral in nature.
Disadvantages do exist for mechanical instrumentation. A level of aerosol is delivered during instrumentation and in vitro and in vivo evidence does demonstrate the possibility of blood borne pathogens in the droplets outside of the oral cavity. Studies suggest that decreased power and frequency will decrease the amount and travel distance of the contamination.11 Recommendations include: protective eyewear, a well-fitting mask and protective shield, a large bore high volume evacuator, and an antimicrobial prerinse prior to instrumentation. The effects of noise and vibration on the operator have undergone limited study. All power-driven instrumentation generates noise during therapy. However, the noise of a 25 kHz insert is at a decibel range still below the Occupational Safety and Health Administration’s recommended standard.
Reduced tactile sensitivity is another drawback of the ultrasonic instrument, especially with increased power settings and larger tips. The clinician can supplement the debridement process by using manual curets with a narrower blade face and shorter blade length (Figure 3).
THE GENERATOR
There are two categories of equipment: sonic and ultrasonic. Piezoelectric and magnetostrictive are the two types of ultrasonics. Sonic devices operate at a comparatively low frequency of 3 kHz to 8 kHz and the energy is air driven from the dental unit. The stroke range is significant in distance and is orbital in tip action. Sound and decreased clinical power limit their use in versatile dental practices.
The piezoelectric units use a quartz crystal that expands and contracts in a horizontal range of motion, thus providing a linear action of the tip. Little heat is generated and water is not necessary to cool the elements. The tip activity is in a comparatively high range of frequency at 24 kHz to 45 kHz (cycles per unit of time). Proponents of piezoelectric equipment suggest that with a tip moving in a linear pattern along a tooth, the tip never leaves the tooth surface, decreasing root roughness and gingival distention with enhanced patient comfort. Comparative studies of most equipment designs do not support or refute these concepts and are limited by the study designs and number of subjects.
Magnetostrictive units were the pioneers in power-driven instrumentation and have gone through significant transformations since 1957. Originally designed for tooth cavity preparation, they quickly lost favor with the advent of high-speed dental turbine devices. Magnetostrictive devices were primarily manually tuned instruments and, due to the nature of the tip size, were indicated for supragingival calculus removal. Autotuning devices were developed a decade later to enhance the ease of use without constantly retuning the instrument. Due to difficulty with subgingival access using large tips, Holbrook advocated thin tips, especially for periodontal therapy.12 Companies developed thin tips to work in autotune magnetostrictive devices but fracture from metal fatigue is still a significant problem due to stress.
Magnetostrictive units convert alternating electrical current into mechanical energy at a vibration frequency of 25 kHz to 35 kHz with an action that is elliptical in nature. All sides of the tip are active with the very end of the tip having the highest intensity. With this versatility of the tip, more surface area can be covered on the root surface, especially in concavities as furcations with minimal hand/wrist movement.13 A water coolant passing through the coils of the insert is mandatory to offset the heat generated. The positive side effect is a preheated lavage to enhance the antimicrobial activity of the device. 4
DESIGNING EFFECTIVE INSERTS
With patent restrictions ending on original magnetostrictive inserts, many companies now manufacture and market a wide variety of devices. A common physical characteristic is the smaller diameter size for subgingival access.
In the late 1980s, a series of slim ultrasonic inserts were introduced. The tips ranged in size, including thin, but the primary difference with other inserts is that the water delivery is exited through a small lumen in the underside of the tip itself. Thus, the irrigant aerosol range is more focused to a fixed area and is contained in the working field with the irritant directed toward the tip. The external water tubing is eliminated and the result is enhanced visibility and no water tube maintenance.
The most significant characteristic for biofilm access is the diameter of the tip. Microthin ultrasonic tips are the present and future of power-driven instrumentation. Paradoxically, many clinicians use small diameter periodontal probes (0.4 mm) to measure disease and larger therapeutic devices (>1.0 mm) to treat the disease (Figure 4, page 20). While many inserts have tips with the last 1 to 2 millimeters being 0.5 mm in diameter, few possess a dimension with the last 4 mm to 8 mm in length being less than 0.5 mm in diameter. If a periodontal pocket has depth greater than 4 mm, the insert must be thin in length to negotiate the anatomy of the pocket (Figure 5).
Future innovations for tip design will include a continued decrease in diameter of tips and diamond coating for time efficiency. Several manufacturers have developed products with various diamond grit grades. Fine diamond coatings should be selected to prevent root damage.
|
Figure 5. Diameter of inserts and corresponding procedures. |
||
|
Insert category |
Diameter at 5 mm from tip |
Procedure indication |
|
P10 |
1.0 mm to 1.5 mm |
Gross debridement |
|
P50 |
0.5 mm to 0.8 mm |
Gingival debridement Peridontal debridement |
|
P100 |
<0.5 mm |
Peridontal debridement |
PATIENT COMFORT
A true challenge in ultrasonic therapy is to match debridement effectiveness with patient comfort. We have struggled with the ability to put the three primary variables: power, frequency, and water lavage in concert with one another to create versatility in the debridement zone. When using manual frequency, thinner tips can be used at higher power ranges, but this necessitates technique sensitivity and constant management of the tuning device. Auto tuning is convenient, but a combination of a higher frequency either creates no tip activity at lower power for comfort or too much activity with discomfort at higher power ranges. To overcome this dilemma, engineers developed new magnetostrictive devices that maintain scaling/root planing effectiveness at lower power settings with patient comfort. Traditional systems have a one-direction system from the generator to the insert. With lower power settings, the stroke is reduced along with the tip’s ability to remove debris and its antimicrobial characteristics. These units use a 30 kHz shorter insert decreasing weight and audible noise levels. In addition to enhanced ergonomics, a foot control with the ability to adjust power is a must. The result is enhanced time motion effectiveness and a decrease in cross contamination activity in the workplace.
While the mission of the early developers of power-driven instrumentation was to create a device that would remove caries and gross calculus, we are fortunate that the industry has moved power-driven instrumentation into progressive periodontal therapy. It is critical that the primary goals of periodontal therapy include gaining or maintaining attachment levels to ultimately retain the dentition. With advances in equipment that will enhance access in a user-friendly mode with improved patient comfort on the horizon, the future of ultrasonic therapy remains bright.
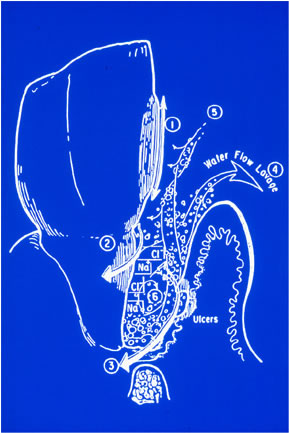 |
Figure 6. Multiple actions in ultrasonic dental instrumentation:
|
 |
Figure 7. Placement of mini-tip in furcation. |
 |
Figure 8. Comparison of large diameter handles with conventional ultrasonic grips. |
 |
Figure 9. Iodine medicaments in conjuction with micro-thin tips. |
References
- O’Leary TJ. The impact of research and scaling on root planing. J Periodontol . 1986;57:69-75.
- Sbordone L, Ramaglia L, Guletta E, Iacono V. Recolonization of the subgingival microflora after scaling and root planing in human periodontitis. J Periodontol .1990;61:579-584.
- Rosenberg RM, Ash MM Jr. The effect of root roughness on plaque accumulation and gingival inflammation. J Periodontol. 1974;45:146-150.
- Walmsley AD, Laird WRE, Williams AR. Dental plaque removal by cavitational activity during ultrasonic scaling. J Clin Periodontol . 1988;15:539-543.
- Baehni P, Thilo B, Chapuis B, Pernet D. Effects of ultrasonic and sonic scalers on dental plaque microflora in vitro and in vivo. J Clin Periodontol . 1992;19:455-459.
- Dragoo MR. A clinical evaluation of hand and ultrasonic instruments on subgingival debridement. 1. With unmodified and modified ultrasonic inserts. Int J Periodontics Restorative Dent. 1992;12:310-323.
- Copulos TA, Low SB, Walker CB, Trebilcock Y, Hefti AF. Comparative analysis between a modified ultrasonic tip and hand instruments on clinical parameters of periodontal disease. J Periodontol . 1993;64:694-699.
- Leon LE, Vogel RI. A comparison of the effectiveness of hand scaling and ultrasonic debridement in furcations as evaluated by differential dark-field micorscopy. J Periodontol . 1987;58:86-94.
- Otero-Cagide FJ, Long BA. Comparative in vitro effectiveness of closed root debridement with fine instruments on specific areas of mandibular first molar furcations. II. Furcation area. J Periodontol . 1997;68:1098-1101.
- Hallmon WW, Rees TD. Local anti-infective therapy: mechanical and physical approaches. A systematic review. Ann Periodontol . 2003;8:99-114.
- Harrel SK, Barnes JB, Rivera-Hildalgo F. Aerosol splatter contamination from the operative site during ultrasonic scaling. J Am Dent Assoc. 1998;129:1241-1249.
- Holbrook T, Low SB. Power driven scaling and polishing instruments. In: Hardin JF, ed. Clark’s Clinical Dentistry . 3rd ed. Philadelphia: JB Lippincott; 1994:1-24.
- Ultrasonic scalers-2003. CRA Newsletter . 2003;27:1-3.
From Dimensions of Dental Hygiene. September 2004;2(9):18, 20, 22-23.