
The Art of Dental Radiography
Take this quiz to evaluate your radiographic diagnostic skills.
Dental radiography is both an art and a science. “Art” is defined as a skill acquired by experience, study, or observation, while “science” is defined as a technique that is tested through scientific method. The science of dental radiography requires sophisticated equipment to produce an X-ray image, while the principles of geometry are used to acquire accurate images with minimal distortion (eg, paralleling technique).1
Once a dental image has been produced, the art of dental radiography comes into play. It involves the observer’s ability to interpret black and white images that, quite frankly, resemble Rorschach ink blots to the lay person. Interpretation involves the application of the observer’s knowledge, cognitive skills, and accumulated experience.1–5 The best technology cannot correct for visual miscues.
The role of the dental hygienist often includes exposing radiographs, assessing the quality of the resultant images (ie, technique errors) and finally, detecting dental anomalies on those radiographic images.

INTERPRETATION OF RADIOGRAPHS
In general, oral health professionals often focus solely on the teeth when interpreting radiographs. Consequently, they may fail to see pathological alterations to the surrounding structures, even when the anomaly is obvious. Oral health professionals who view radiographic images should develop their own sequential pattern for examining the entire field—whether it is an extraoral or an intraoral radiograph. This should reduce the number of osseous pathology cases that are overlooked. The likelihood of a clinician failing to recognize a blatantly large lesion is unlikely. It is the small, innocuous lesions located away from the dentition that tend to be missed. Regardless of whether a clinician is observing an intraoral or extraoral radiograph, he or she should focus on the surrounding structures first and leave the examination of the dentition until the end. This will help to avoid many missed diagnoses.
When interpreting extraoral radiographs (Figure 1), oral health professionals should initially evaluate the following:1
- Maxillary sinuses
- Orbits
- Border of the mandible
- Temporomandibular joint
- Border of the maxilla
They should be looking for deviations from the expected norm. As mentioned earlier, the dentition should not be diagnosed until after everything else has been assessed. Bilateral examination of anatomical landmarks (eg, those visible on a panoramic radiograph, Figure 1) can eliminate misinterpretation of normal anatomy as pathology. For example, a developing third molar in the mandibular right quadrant in a teenager may be easily misinterpreted as pathology. The mandibular left quadrant should be compared to the right quadrant. If both right and left quadrants show a similar radiographic appearance and knowing the patient’s young age, the diagnosis of pathology is unlikely. A clinician would conclude that both questionable areas are probably the normal development of the third molars.1
Most cases of osseous lesions appear either single in number or generalized throughout the mandible and/or maxilla.1,6 This applies to lesions not directly associated with teeth (eg, periapical pathology). The incidence of osseous oral pathology occurring bilaterally is rare. Cherubism—a genetic disorder that appears as multilocular radiolucencies typically located bilaterally at the angle and ramus of the mandible—is an example of a bilateral osseous lesion.1,7
When examining intraoral radiographs, such as periapical images, the entire image should be scanned twice.1,8 Scan from the top of the image to the bottom or vice versa. Focus should remain on the surrounding tissues first and then return to observe the teeth for pathology.
In summary, regardless of whether intraoral or extraoral radiographs are being reviewed, developing a sequential pattern for scanning the image(s) and leaving the interpretation of the teeth and the obvious larger lesions to the end will improve diagnostic proficiency.

X-RAY PUZZLE
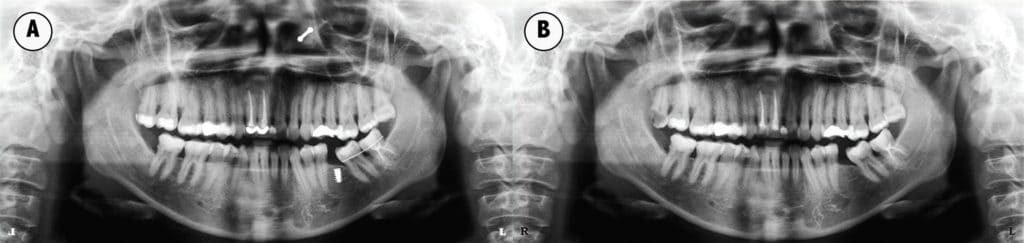
Visual puzzles that show two photographs side by side and ask the reader to find the differences are popular in magazines and online. Similarly, the object of the following radiographic exercise is for the clinician to locate seven subtle differences on two panoramic radiographs (Figure 2). The changes are highlighted in the answer key (Figure 3). This exercise demonstrates that a thorough analysis of every image is critical to finding all of the anomalies.
CONCLUSION
In summary, the sequential radiographic interpretation recommendations and the X-ray puzzle presented here will help support oral health professionals in the critical examination of every radiograph to improve their diagnostic skills. It is unreasonable to expect clinicians to determine a definitive diagnosis of all osseous pathology. Composing a differential list of pathological lesions is often the best that can be achieved with the limited information available at the time of the clinical and radiographic examination. A biopsy report is frequently required to confirm a diagnosis of an isolated osseous lesion, unlike a lesion that is directly attached to a tooth, such as a dental abscess. However, identifying an anomaly and differentiating normal from abnormal are critical first steps.
REFERENCES
- Hubar JS. Fundamentals of Oral and Maxillofacial Radiology. Hoboken, New Jersey: Wiley Blackwell; 2017.
- Mawani F, Lam EW, Heo G, McKee I, Raboud DW, Major PW. Condylar shape analysis using panoramic radiography units and conventional tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:341–348.
- Fallon SD, Fritz GW, Laskin DM. Panoramic imaging of the temporomandibular joint: an experimental study using cadaveric skulls. Oral Maxillofac Surg. 2006;64:223–229.
- Schmitter M, Gabbert O, Ohlmann B, et al. Assessment of the reliability and validity of panoramic imaging for assessment of mandibular condyle morphology using both MRI and clinical examination as the gold standard. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:220–224.
- Koong B. Cone beam imaging: is this the ultimate imaging modality? Clin Oral Implants Res. 2010;21:1201–1208.
- El-Mofty SK. Fibro-osseous lesions of the craniofacial skeleton: an update. Head Neck Pathol. 2014;8:432–444.
- Papadaki ME, Lietman SA, Levine MA, Olsen BR, Kaban LB, Reichenberger EJ. Cherubism: best clinical practice. Orphanet J Rare Dis. 2012;7(Suppl 1):S6.
- Tarcin B, Gumru B, Iriboz E, Turkaydin DE, Ovecoglu HS. Radiologic assessment of periapical health: comparison of 3 different index systems. J Endod. 2015;41:1834–1838.
From Dimensions of Dental Hygiene. February 2018;16(2):30-33.

