The Added Benefit of Antimicrobial Agents
Rebecca S. Wilder, RDH, MS, provides an update on the use of antimicrobials.
Q. Are antimicrobials still recommended for at-home use to help reduce gingivitis?
A. Yes, antimicrobials for home use are available primarily in mouthrinse and dentifrice formats. The most popular active ingredients in at-home antimicrobial dentifrices are triclosan and stannous fluoride. In mouthrinses, the most common active ingredients include essential oils; chlorhexidine (CHX), which is prescription-only; cetylpyridinium chloride (CPC); and stannous fluoride.
Q. What is the difference between an over-thecounter product that contains cosmetic vs therapeutic ingredients?
A. Typically, products deemed cosmetic claim to reduce bad breath, make teeth whiter or brighter, or create less plaque in the mouth. If the claims are cosmetic only, then the product has not gone through the Food and Drug Administration’s (FDA) regulatory process. Cosmetic-only claims may not have scientific evidence to support them.
If a mouthrinse claims that it will reduce gingivitis, including plaque reduction, it is then considered therapeutic and subject to FDA regulations. If the product carries the American Dental Association (ADA) Seal of Acceptance as well, then it has undergone additional scrutiny and met the guidelines for acceptance, which include scientific evidence for efficacy. The ADA Seal of Acceptance is now only available for over-the-counter products, not for professionally applied products. This means that a product like CHX, which previously carried the ADA Seal, will no longer have this designation—only because it is professionally dispensed. This change does not reflect any reduction in efficacy.
Q. Are antimicrobial agents effective for the control of periodontitis?
A. CHX, essential oils, CPC, triclosan, and stannous fluoride have all been shown to reduce gingivitis and to decrease plaque scores.1-3 At-home antimicrobials have very little effect on periodontitis directly. Indirectly, they control biofilm and gingivitis but we have not found an at-home product that is specifically effective for periodontitis.
At home irrigation is also a popular method for helping to reduce and control plaque and gingivitis. An irrigation device can deliver an antimicrobial or water subgingivally up to 6 mm with a subgingival tip or cannula.4 The patient can use an antimicrobial solution (eg, CHX, essential oils, sodium hypochlorite) in an irrigator, but water alone has been shown to be effective.5-7
IN-OFFICE PRODUCTS
Q. What are some of the more commonly used in-office antimicrobial products for gingivitis and periodontitis?
A. Dental hygienists use antimicrobial products in the office either as preprocedural rinses to reduce aerosolized bacteria or as agents for an irrigation procedure. In-office irrigation is applied separately (usually with a cannula) or during power instrumentation to deliver a potential added benefit of the antimicrobial action. However at this time, research does not seem to support in-office irrigation as an adjunct to scaling and root planing procedures.8 For example, CHX and essential oils are commonly used for in-office irrigation as is povidone-iodine (Betadine®) in some regions of the country. Research shows that while CHX and essential oils are excellent antimicrobial rinses for plaque and gingivitis control, their efficacy subgingivally via irrigation or with power instrumentation has produced mixed results.9 While povidone-iodine 10% has shortterm benefits in the treatment of periodontitis, large clinical trial data are still needed to fully evaluate efficacy.10
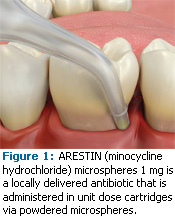
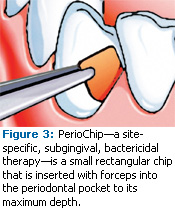
 For the treatment of periodontitis, the inoffice, site-specific locally administered anti-microbial/ antibiotics currently on the market are ARESTIN, ATRIDOX, and PerioChip (see Table 1). The reason that mouth rinses are not as effective as site-specific, locally administered antimicrobials is because the use of a rinse subgingivally through irrigation or power instru mentation in patients with moderate periodontitis does not provide the substantivity needed to make a significant change in the bacteria. Substantivity is the capacity of an oral antimicrobial agent to continue its therapeutic activity for a prolonged period of time. Nor is the concentration of the antimicrobial enough to kill or suppress the bacteria for the appropriate length of time. This is called the minimal inhibitory concentration (MIC) and it represents the concentration of antibiotic required to inhibit growth of a planktonic bacterial population. Site-specific, locally administered agents have a higher and a longer substantivity and they maintain a MIC for enough time to make a positive effect in the pocket. For example, ARESTIN has been shown to have a high MIC for 14 days to 21 days.11 The antimicrobial is placed in the pocket, it releases the drug for a certain length of time, and it kills or suppresses bacteria that are not eradicated through scaling and root planing. If dental hygienists are treating patients with periodontitis, locally administered antimicrobials are much more effective than mouthrinses subgingivally. While locally administered antimicrobials are not 100% effective, they can work quite well in some patients and sites.
For the treatment of periodontitis, the inoffice, site-specific locally administered anti-microbial/ antibiotics currently on the market are ARESTIN, ATRIDOX, and PerioChip (see Table 1). The reason that mouth rinses are not as effective as site-specific, locally administered antimicrobials is because the use of a rinse subgingivally through irrigation or power instru mentation in patients with moderate periodontitis does not provide the substantivity needed to make a significant change in the bacteria. Substantivity is the capacity of an oral antimicrobial agent to continue its therapeutic activity for a prolonged period of time. Nor is the concentration of the antimicrobial enough to kill or suppress the bacteria for the appropriate length of time. This is called the minimal inhibitory concentration (MIC) and it represents the concentration of antibiotic required to inhibit growth of a planktonic bacterial population. Site-specific, locally administered agents have a higher and a longer substantivity and they maintain a MIC for enough time to make a positive effect in the pocket. For example, ARESTIN has been shown to have a high MIC for 14 days to 21 days.11 The antimicrobial is placed in the pocket, it releases the drug for a certain length of time, and it kills or suppresses bacteria that are not eradicated through scaling and root planing. If dental hygienists are treating patients with periodontitis, locally administered antimicrobials are much more effective than mouthrinses subgingivally. While locally administered antimicrobials are not 100% effective, they can work quite well in some patients and sites.
METHOD OF ACTION
Q. How do these locally administered antimicrobials work?
A. They deliver an antimicrobial or an antibiotic to a site with the goal of improving the periodontal health of the site (reduction in pocket depth, reduced bleeding on probing, increase in clinical attachment levels). Mechanical therapy does not remove all of the bacteria from the tooth and root surface, regardless of the skill level of the dental hygienist or dentist, so locally administered antimicrobials kill or suppress the level of bacteria for longer periods of time. In some patients, periodontitis can be managed with routine debridement and scaling and root planing but others will require additional therapies. For patients with chronic periodontitis, this collective approach to therapy may increase the effectiveness of treatment.
ARESTIN, ATRIDOX, and PerioChip deliver an antibiotic to the base of the pocket (see Figures 1-3). They also all have concentrations strong enough and the sustainability to kill or inhibit bacteria for an extended period of time. Easy to place, these antimicrobials all provide good retention in the pocket and they are biodegradable.
 |
 |
 |
Q. Can you recommend a resource for additional guidance on the use of inoffice antimicrobials?
A. Last year, the Journal of Dental Hygiene published a supplement called “Rationale for Comprehensive Nonsurgical Periodontal Therapy: A Review of the Clinical Evidence and Practice Protocol.” It contains a paper I coauthored with David W. Paquette, DMD, MPH, DMSc, and Maria Emanuel Ryan, DDS, PhD, titled “Locally Delivered Antimicrobials: Clinical Evidence and Relevance” that provides an extensive review of the literature on studies to date regarding site-specific local delivery.12 Another useful paper in the supplement is “Periodontal Treatment Protocol for the General Dental Practice”by Larry Sweeting, DDS; Karen Davis, RDH, BS; and Charles Cobb, DDS, PhD.13 This paper exclusively talks about how to incorporate locally administered antimicrobials into clinical practice. The complete supplement is available at no charge to all dental hygienists at the American Dental Hygienists’ Association website (http://www.adha.org/downloads/JDH_Local_delivery_supplement.pdf).
WHAT THE FUTURE MAY HOLD
Q What do you think the future holds for the use of antimicrobials in the dental arena?
A I think we are going to see more sophisticated, target-specific antimicrobials in the future. Currently in health care, the focus is on trying to find ways to target particular diseases rather than use strategies that have an effect on the entire body. Locally administered antimicrobials do this to some degree in that we are able to treat a disease locally rather than systemically as we do with systemic antibiotics. But I think we will eventually be able to determine particular bacteria that are contributing to a patient’s disease and then have therapies that can actually target those specific bacteria rather than all of the bacteria in the patient’s oral cavity or in the pocket itself. I also think we will see advances in host modulation therapies.
REFERENCES
- Lorenz K, Bruhn G, Heumann C, Netuschil L, Brecx M, Hoffmann T. Effect of two new chlorhexidine mouthrinses on the development of dental plaque, gingivitis, and discolouration. A random ized, investigator-blind, placebo-con – trolled, 3-week experimental gingivitis study. J Clin Periodontol. 2006;33:561-567.
- Cortelli SC, Cortelli JR, Holzhausen M, et al. Essential oils in one-stage full-mouth disinfection: double-blind, randomized clinical trial of longterm clinical, microbial and salivary effects. J Clin Periodontol. 2009;36:333-342.
- Kozak KM, Gibb R, Dunavent J, White DJ. Efficacy of a high bioavailable cetylpyridinium chloride mouthrinse over a 24-hour period: a plaque imaging study. Am J Dent. 2005;18(Spec No):18A-23A.
- Braun RE, Ciancio SG. Subgingival delivery by an oral irrigation device. J Periodontol. 1992; 63: 469-472.
- Mariotti AJ, Burrell KH. Mouthrinses and Dentifrices. In: Ciancio SG, ed. ADA/PDR Guide to Dental Therapeutics. 4th ed. Chicago: ADA; 2007.
- Jolkovsky DL, Waki MY, Newman MG, et al. Clinical and microbiological effects of subgingival and gingival marginal irrigation with chlor hexidine gluconate. J Periodontol. 1990;61:663-669.
- Walsh TF, Glenwright HD, Hull PS. Clinical effects of pulsed oral irrigation with 0.2% chlorhexidine digluconate in patients with adult periodontitis. J Clin Periodontol. 1992;19:245-248.
- Greenstein G; Research, Science and Therapy Committee of the American Academy of Periodontology. Position paper: The role of supra- and subgingival irrigation in the treatment of periodontal diseases. J Periodontol. 2005;76:2015- 2027.
9. Hallmon WW, Rees TD. Local anti-infective therapy: mechanical and physical approaches. A systematic review. Ann Periodontol. 2003;8: 99-114.
10. Slots J. Selection of antimicrobial agents in periodontal therapy. J Periodontal Res. 2002; 37: 389-398.
11. Christersson LA. Tissue response and release of minocycline after subgingival deposition by use of a resorbable polymer. Warminster, Pa: OraPharma Inc; 1988.
12. Paquette DW, Ryan ME, Wilder RS. Locally delivered antimicrobials: clinical evidence and relevance. J Dent Hyg. 2008;82(Suppl 3):10-15.
13. Sweeting LA, Davis K, Cobb CM. Periodontal Treatment Protocol (PTP) for the general dental practice. J Dent Hyg. 2008;82(Suppl 3):16-26.
From Dimensions of Dental Hygiene. June 2009; 7(6): 18-20.

