Small Incision = Big Benefits
Patients, periodontists, and dental hygienists all gain the advantages of minimally invasive periodontal surgery.
Minimally invasive periodontal surgery (MIS) is a surgical approach for the treatment of periodontal diseases that was introduced in 1995.1-5 The guiding principle of minimally invasive surgery is to make the incisions as small as possible and to confine the periodontal surgical procedure to the site of the periodontal defect.
MIS offers many advantages for the patient over osseous surgery or traditional regenerative periodontal surgery. Most of these advantages are based on the fact that the incisions are smaller. Smaller incisions result in less post-operative pain, more rapid healing, little post-operative change in tissue contour, minimal post-operative sensitivity, and a more rapid return to routine activities.6 Patients often have multiple sites of MIS performed in a single surgical session with little or no post operative pain. The necessity for post-operative narcotics is rare, with most patients taking only over-the-counter medication. Patients can return to most normal activities the day following surgery. Moderately firm food can be chewed in the surgical area within 1 to 2 days, and routine chewing of hard foods is possible within 1 to 2 weeks. Cold sensitivity, which frequently occurs following most other periodontal surgical procedures, is rare with MIS. The application of desensitizing medication is not usually necessary.
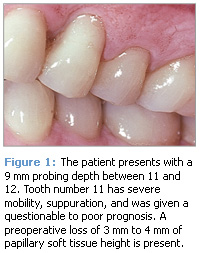
One of the most rewarding advantages of MIS for the patient and the periodontist is the lack of negative post-operative esthetic concerns. Recession and root exposure (long teeth) are routine following osseous surgical procedures and are frequent following traditional regenerative surgery. Recession results in unfavorable post-operative esthetics that may cause many patients to avoid periodontal surgery. MIS routinely results in minimal recession. Wilson, Nunn, and I reported recession of 0.05 mm in 160 sites while Cortellini and Tonetti reported 0.1 mm of recession in 13 sites.5,7 These levels of recession are more favorable than those reported with other periodontal regenerative surgical procedures. With MIS, post-operative esthetic concerns are rare. See Figures 1-3 for a visual case study of a patient receiving MIS.
 |
 |
 |
ADVANTAGES OF MIS FOR THE DENTAL HYGIENIST
Dental hygienists are first and foremost concerned about their patients’ periodontal health. The results of nonsurgical treatment performed by a dental hygienist are often excellent with only one or two sites continuing to have deep probing depths. While it may be possible to maintain deeper pockets with frequent periodontal maintenance, a large body of research indicates that the strongest predictor of future periodontal breakdown is the presence of a probing depth of 5 mm or greater.8 The American Academy of Periodontology addressed this in its Guidelines for the Management of Patients with Periodontal Disease,9 which was published with permission in the October 2006 issue of Dimensions of Dental Hygiene.
Despite the desire and need for shallow and easily maintained sites, dental hygienists may be reluctant to recommend referral of patients for surgical treatment because traditional periodontal surgery routinely extends beyond the isolated remaining defects with the adjacent healthy teeth often included in the surgery. This inclusion of healthy teeth within the surgical area may result in recession and sensitivity of teeth that the hygienist has worked hard to bring to a state of periodontal health. With MIS, the surgery is only performed at the sites that have not responded to nonsurgical treatment; negative post-operative esthetic and sensitivity sequelae are rare.
Another advantage of MIS for the dental hygienist is improved patient acceptance of needed periodontal treatment. Patients may be more open to having surgery if they know the incisions will be small and the discomfort minimal. Many patients are afraid of periodontal surgery because of stories they have heard about severe post-operative pain, extended inability to chew, and long-term esthetic problems. Many of these stories come from an era long past when gingivectomy was the routine periodontal surgical procedure. All periodontal surgery has progressed since that time and most of these stories are not relevant to any modern periodontal surgical techniques. However, the tales of horror persist and they often influence patients’ acceptance of needed periodontal therapy.
When discussing referral for MIS with patients, the dental hygienist can point out that MIS is similar to what is referred to as “bandaid” surgery on other parts of the body. Thirty years ago, the removal of a gall bladder required an incision 12 to 14 inches long, a week or more in the hospital, bed rest for 2 to 6 weeks, and 8 to 10 weeks of recuperation before returning to routine activities. In contrast, when gall bladder removal is accomplished using medical minimally invasive surgery, one or two incisions are made of approximately 1 inch or less, the procedure may be performed on an outpatient basis, and the patient usually returns to most normal activities within a week. MIS for periodontal procedures has similar advantages like decreased post-surgical discomfort and a rapid return to normal activities. Patient acceptance of referral for MIS is usually excellent when the advantages of MIS over other types of periodontal surgery are explained.
MIS represents a significant change in the way surgical periodontal procedures are performed. While other types of small incision surgeries have been used in the past, none have led to the favorable results reported for the MIS technique. The MIS approach meshes well with improved results from nonsurgical procedures achieved by many dental hygienists and allows for isolated site-specific regenerative periodontal surgery for those areas that don’t fully respond to nonsurgical treatment. MIS can help improve long-term patient management for the dental hygienist and result in long-term improvement in patients’ health and function.
REFERENCES
- Harrel SK, Rees TD. Granulation tissue removal in routine and minimally invasive surgical procedures. Compend Contin Educ Dent. 1995; 16:960-967.
- Harrel SK. A minimally invasive surgical approach for periodontal bone grafting. Int J Periodontics Restorative Dent. 1998;18:161-169.
- Harrel SK. A minimally invasive surgical approach for periodontal regeneration: surgical technique and observations. J Periodontol. 1999;70:1547-1557.
- Harrel SK, Wright JM. Treatment of periodontal destruction associated with a cemental tear using minimally invasive surgery. J Periodontol. 2000;71:1761-1766.
- Harrel SK, Wilson TG, Nunn ME. Prospective assessment of the use of enamel matrix proteins with minimally invasive surgery. J Periodontol. 2005;76:380-384.
- Cortellini C, Tonetti M. Minimally invasive surgical technique and enamel matrix derivative in intra-bony pockets. I: clinical outcomes and morbidity. J Clin Periodontol. 2007;34:1082-1088.
- Cortellini P, Tonetti MS. A minimally invasive surgical technique with an enamel matrix derivative in the regenerative treatment of intrabony defects: a novel approach to limit morbidity. J Clin Periodontol. 2007;34:87-93.
- Garrett S. Periodontal regeneration around natural teeth. Ann Periodontol. 1996;1:621-666.
- Krebs KA, Clem DS 3rd, American Academy of Periodontology. Guidelines for the management of patients with periodontal diseases. J Periodontol. 2006;77:1607-1611.
From Dimensions of Dental Hygiene. April 2008; 6(4): 22, 24.