Prevent Cement-Associated Peri-Implantitis
Stacy A. Matsuda, RDH, BS, MS, discusses this serious threat to implant viability and what can be done to prevent it.
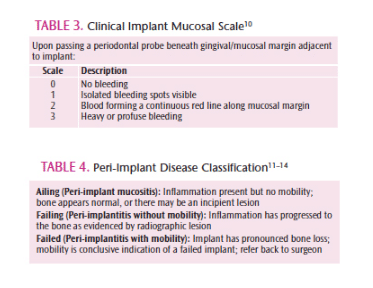
Cement-associated peri-implantitis is a growing concern about which dental professionals must be knowledgeable (Figure 1 to Figure 3). Fully integrated implants ready for prosthetic restoration can be setup to fail due to crown cementation displacing excess cement into the peri-implant space.1,2 This error often escapes detection even when post-restorative radiographs have been examined, as only the direct mesial and distal surfaces of the implant threads and abutment are visible. Because most implant cements on the market today are radiolucent, detecting cement left behind is difficult.3
To help clinicians prevent cement-associated peri-implantitis, instrumentation expert Stacy A. Matsuda, RDH, BS, MS, shares her expertise in this informative interview with Dimensions of Dental Hygiene.
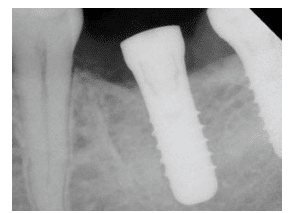 FIGURE 1. This osseointegrated implant is ready for the restorative phase. The patient signs a form acknowledging the need to return to the surgeon for postrestorative follow-up to confirm prosthetic integrity and receive professional maintenance.
FIGURE 1. This osseointegrated implant is ready for the restorative phase. The patient signs a form acknowledging the need to return to the surgeon for postrestorative follow-up to confirm prosthetic integrity and receive professional maintenance.
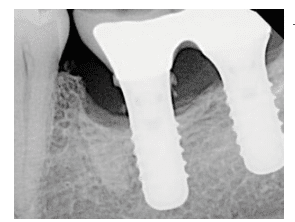 FIGURE 2. Six years later, after failing to follow-up with the surgical office to have the restored implant examined, the patient returned. In this case, the excess cement retained is readily apparent on the radiograph; often, the reverse is true.
FIGURE 2. Six years later, after failing to follow-up with the surgical office to have the restored implant examined, the patient returned. In this case, the excess cement retained is readily apparent on the radiograph; often, the reverse is true.
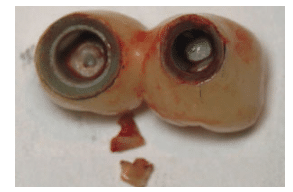 FIGURE 3. These prosthetics were removed from the implant, along with sizeable pieces of retained cement, which was a permanent acrylic resin. The patient required surgical repair to access and remove cement, as well as bone grafting to fill the defect. FIGURE 1 TO FIGURE 3 COURTESY OF DAVID FRENCH, DDS, CALGARY, ALBERTA, CANADA
FIGURE 3. These prosthetics were removed from the implant, along with sizeable pieces of retained cement, which was a permanent acrylic resin. The patient required surgical repair to access and remove cement, as well as bone grafting to fill the defect. FIGURE 1 TO FIGURE 3 COURTESY OF DAVID FRENCH, DDS, CALGARY, ALBERTA, CANADA
How does the problem of cement-associated peri-implantitis occur?
The mere presence of residual cement creates the issue. Its rough, outer surface forms profuse niches for biofilm to attach to and mature undisturbed—often to the point of calculus formation.4 Prosthetic cements used for implants are generally resin-based, creating a permanent bond. Unlike traditional cements, they cannot be removed with any degree of certainty via nonsurgical scaling and root planing. Excess cement will continue to pose a problem until it can be effectively removed, which is generally accomplished through the creation of access via a surgical flap.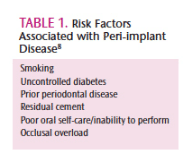
A confounding factor is that cement-associated peri-implantitis can occur well after case completion and assumed stability. Research has shown there may be a delay of up to 9 years before clinical signs of implant failure become evident.5
What can be done to prevent cement-associated peri-implantitis?
The implementation of preemptive strategies for the restorative dentist is essential. Precise machining of the crown-abutment interface leaves no margin for error in cementation, meaning the amount of cement used must be tightly controlled.6 For implant prosthetics that are cement- rather than screw-retained, the type of cement used should be documented. The use of zinc-based cements that are radiopaque and bacteriostatic is recommended for cement-retained implant prosthetics.3 Additionally, positioning abutment margins at or above the gingival margin while tightly controlling the volume and flow of cement used can prevent or reduce the prevalence of this problem.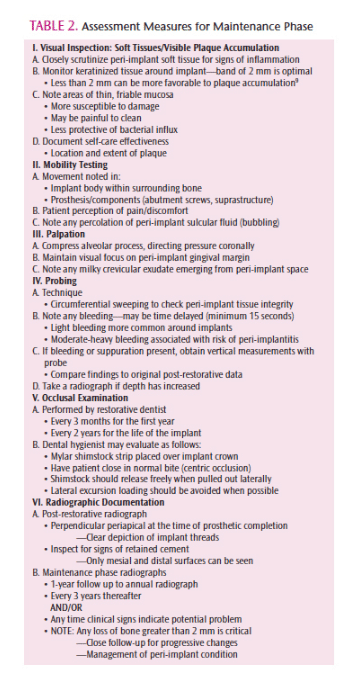
If an implant analogue of solid or final custom abutment is available, it can be used to express excess cement by positioning the crown onto the model prior to cementation in the mouth. Additionally, a small vent hole can be placed on a PFM-style crown at the cingulum, which has been shown to reduce the volume of cement expressed subgingivally.7
What Is The Role of The Dental Hygienist in Implant Maintenance Therapy?
Early intervention is essential for any implant showing signs of inflammation. Develop a practice protocol for implant maintenance that incorporates risk (Table 1) and methodical assessment (Table 2).8,9 Scales for the classification of mucosal findings are shown in Table 3.10 Use a safe and effective armamentarium for implant maintenance that permits maximum value in professional instrumentation. All-metal titanium instruments provide the strength and rigidity needed to remove calculus that is embedded in cement. However, most cements cannot be removed nonsurgically. Instruments and ultrasonic inserts/tips designed for safe use on implants can be utilized for light calculus removal. Titanium micro-mini-bladed Gracey curets provide access into very tight areas, and should be part of the implant maintenance armamentarium. Should an implant exhibit visual signs of inflammation, a brief follow-up tissue check is mandated.
Peri-implant inflammation (Table 4) can advance from mucositis to the irreversible bony destruction of peri-implantitis without warning.11–14 Although comparable to periodontitis in terms of irreversible bone loss, peri-implantitis is marked by a greater severity of tissue destruction at a faster rate of progression than periodontitis. Peri-implant disease progression can be rapid and fatal to the implant—once there is detectable mobility, the implant has failed and must be removed. Dental hygienists must be vigilant to the subtlest signs that something is wrong, and then respond appropriately.
Peri-implant diseases cannot be reliably controlled with the same measures used in the treatment of periodontal inflammation, due to anatomical differences in the attachment apparatus.15 An ailing implant that has not favorably responded to maintenance debridement within 2 weeks should be referred back to the surgeon for immediate attention. Considering the investment made and implications of progressive decline, it is better to err on the side of caution. If at any time retained cement is suspected, refer the case back to the surgeon for surgical debridement.
Perhaps one of the most significant roles dental hygienists can play is that of quarterback for the maintenance phase of implant therapy. As part of the implant team, dental hygienists should have a working relationship with the specialty offices handling the surgical phase of implant placement. A critical juncture occurs in the first few months of function following restorative completion—one typically underestimated by the patient. The surgeon must see his or her patient for a follow-up examination prior to transitioning to the maintenance phase. A radiograph is taken to confirm prosthetic fit, peri-implant tissue is inspected, and occlusal function is evaluated. This follow-up is key to achieving a successful outcome.
![]() REFERENCES
REFERENCES
- Linkevicius T, Puisys A, Vindasiute E, Linkeviciene L, Apse P. Does residual cement around implant-supported restorations cause peri-implant disease? A retrospective case analysis. Clin Oral Implants Res. 2013;24:1179–1184.
- Gapski R, Neugeboren N, Pomeranz AZ, Reissner MW. Endosseous implant failure influenced by crown cementation: a clinical case report. Int J Oral Maxillofac Implants. 2008;23:943–946.
- Wadhwani C, Rapoport D, La Rosa S, Hess T, Kretschmar S. Radiographic detection and characteristic patterns of residual excess cement associated with cement-retained implant restorations: a clinical report. J Prosthet Dent. 2012;107:151–157.
- Lee A, Wang HL. Biofilm related to dental implants. Implant Dent. 2010;19:387–393.
- Wilson TG. The positive relationship between excess cement and peri-implant disease: a prospective clinical endoscopic study. J Periodontol. 2009;80:1388–1392.
- Korsch M, Walther W. Peri-implantitis associated with type of cement: a retrospective analysis of different types of cement and their clinical correlation to the peri-implant tissue. Clin Implant Dent Relat Res. 2014 Sep 2. Epub ahead of print.
- Patel D, Invest JCF, Tredwin CJ, Setchell DJ, Moles DR. An analysis of the effect of a vent hole on excess cement expressed at the crown–abutment margin for cement-retained implant crowns. J Prosthodont. 2009;18:54–59.
- Karbach J, Callaway A, Kwon YD, d’Hoedt B, Al-Nawas B. Comparison of five parameters as risk factors for peri-mucositis. Int J Oral Maxillofac Implants. 2009;24:491–496.
- Schrott AR, Jiminez M, Hwang JW, Fiorellini J, Weber HP. Five-year evaluation of the influence of keratinized mucosa on peri-implant soft-tissue health and stability around implants supporting full-arch mandibular fixed prostheses. Clin Oral Implants Res. 2009;20:1170–1177.
- Mombelli A, van Oosten MA, Schurch E Jr, Land NP. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immun. 1987;2:145–151.
- Meffert, RM. Maintenance and treatment of the ailing and failing implant. J Indiana Dent Assoc. 1994;73:22–24.
- Lindhe J, Meyle J. Peri-implant diseases: Consensus report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008;35(Suppl 8): 282–285.
- Sanz M, Chapple IL. Clinical research on peri-implant diseases: Consensus report of Working Group 4. J Clin Periodontol. 2012;39(Suppl 12):202–206.
- Tomasi C, Derks J. Clinical research of peri-implant diseases—quality of reporting, case definitions and methods to study incidence, prevalence and risk factors of peri-implant diseases. J Clin Periodontol. 2012;39(Suppl 12): 207–223.
- Belibasakis GN. Microbiological and immuno-pathological aspects of peri-implant diseases. Arch Oral Biol. 2014;59:66–72.
From Dimensions of Dental Hygiene. November 2014;12(11):34,36–37.