 STURTI/ISTOCK/GETTY IMAGES PLUS
STURTI/ISTOCK/GETTY IMAGES PLUS
Motivational Interviewing for Dental Hygienists
The majority of periodontal patients can retain their dentition with appropriate treatment, effective plaque control, and regular maintenance.
This course was published in the May 2017 issue and expires May 2020. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the advantages, clinical uses, and evidence supporting motivational interviewing (MI) in oral health care.
- Identify MI strategies that can be used in clinical practice.
- Explain the key elements and terminology of MI in dental settings.
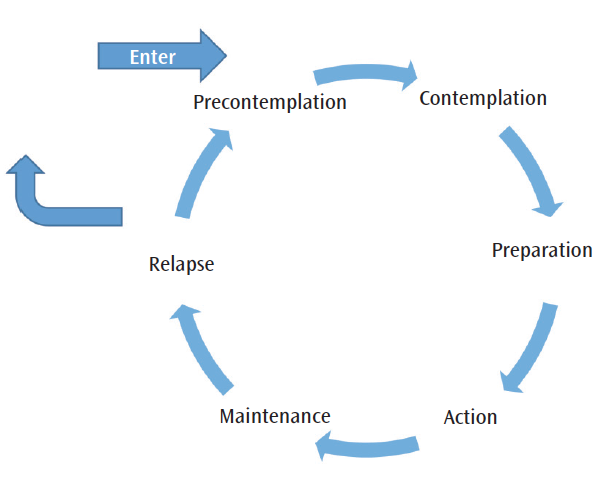
Before discussing behavioral changes, understanding the process a patient goes through when deciding if he or she is ready for change is important.6 Behavioral changes are often difficult and require individual effort to adopt new choices.6 Numerous models and theories explain the process of health behavior changes, such as the Transtheoretical Stages of Change Model (Figure 1), which details the sequential steps in this process.15 By understanding the stages of change, clinicians gain insight into a patient’s readiness to change.6 Supporting a patient’s desire to change by igniting personal motivation is known as intrinsic motivation, and patient-centered counseling has proven to be an effective method for eliciting intrinsic motivation.6,10 Clinicians may be able to achieve this by understanding an individual’s values as they relate to the behavior identified for change.
MI is an evidence-based, patient-centered, collaborative counseling approach that focuses on strengthening a patient’s motivation for a positive change in behavior.10 Research began in 1983 for use in substance abuse and addiction therapy.10,16 Since then, MI has been adapted for use in a variety of health care settings to support positive behavioral changes. This approach helps patients accept responsibility for their health and encourages autonomy in their decision making.10 The goal is to evoke a positive behavioral change from within to improve health.10
This clinical strategy is more of a philosophy than a technique, and is best described as the “spirit of MI.”5,10 Four integrated components foster communication and encompass the spirit of MI: partnership, acceptance, compassion, and evocation (Figure 2).5,10 Partnership encourages communication “with” a person (as a partner) to collaborate in order to reach a goal.5,10 During this partnership, the patient and clinician develop rapport and, when appropriate, the practitioner asks permission to discuss potential behavior changes.10,11 Asking permission lets the clinician know the individual is willing to enter into a discussion.10 Complementary to partnership is acceptance of the patient’s autonomy.10 This requires recognizing a person’s absolute worth and internal motivation to change.10 Compassion involves promoting the patient’s well-being and remaining committed to his or her best interests.10 The evocation component leverages internal motivation to adopt what is already present within the patient.5,10Collectively, these elements describe the mindset of clinicians who truly practice the spirit of MI during patient interactions.10

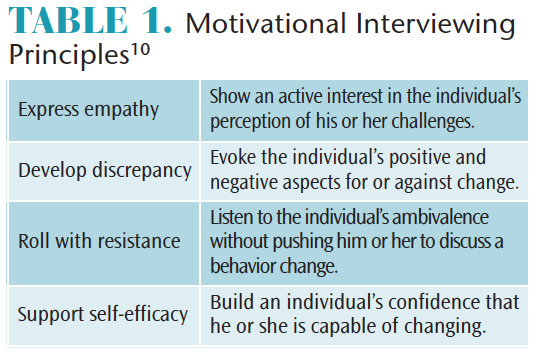
FOUR GUIDING PRINCIPLES
MI has four principles: empathy, discrepancy, rolling with resistance, and supporting self-efficacy (Table 1).5,10 By applying these principles, the clinician allows a patient to maintain autonomy throughout the process of behavior change.10 Clinicians report this approach results in more pleasurable and productive patient interactions.5
Expressing empathy focuses on a clinician’s ability to show interest in understanding the patient’s perception.5 The principle of developing discrepancy distinguishes between the patient’s intrinsic values and behaviors that are inconsistent with his or her change goals.5,17 The third MI principle, rolling with resistance, is also referred to as avoiding conflict.5 Identifying a patient’s resistance and responding with support may minimize ambivalence and offer insight into the individual’s internal challenges.5,17 Supporting self-efficacy involves offering encouragement and praise to build confidence in the individual’s ability to change.5,11
Eight MI strategies can be used to assist patients in achieving behavior changes (Table 2).5,10,18 The first four include open-ended questions, affirmations, reflective listening, and summaries (OARS).14 Open-ended questions cannot be answered with “yes” or “no” statements.5,14 Posing a question that provides an opportunity for the patient to craft a response allows clinicians to better understand the patient’s perception of the issue being discussed. Affirmation is achieved by offering encouragement and acknowledgment of a patient’s strengths; for example, recognizing the patient for a positive stride toward a change goal.5 This builds rapport and fosters confidence in the patient’s ability to change behavior.5 Reflective listening allows clinicians to display an understanding of patient perceptions, ambivalence, and efforts.14 It also helps the patient hear his or her thoughts and feelings in a different format, which may support internal motivation to change.10 Summary is used to close the MI session and ensures the clinician understands the patient’s perspective.5 This helps practitioners connect the information provided by the patient to the individual’s specific behavior change goal.5
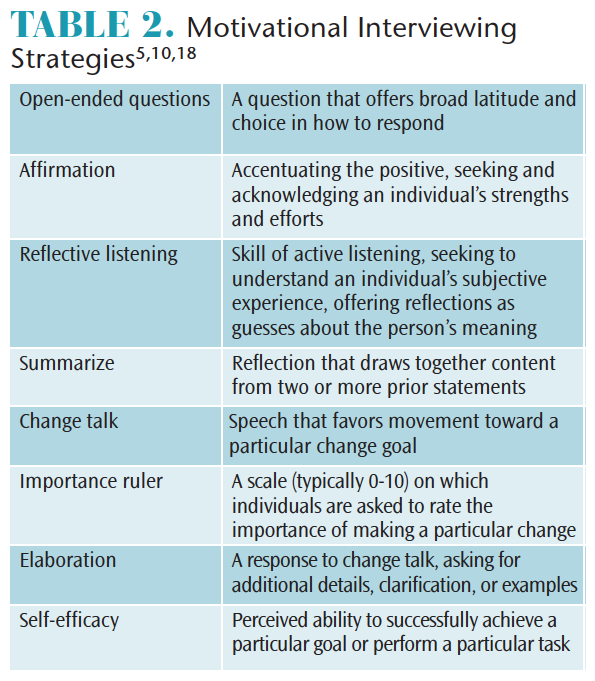 Occasionally, patients see how both sides of a behavior change could positively or negatively impact their lives. Although patient ambivalence is a normal aspect of preparing for behavior change, initiating a “change talk” strategy may help the individual overcome ambivalence based on his or her values and interests.10 Change talk occurs when the individual’s statements identify what behavior needs to change. It is critical for practitioners to recognize when this transition takes place, as it allows clinicians to notify patients they may already be considering a change.10 The key point is that rather than being swayed by clinical instructions, patients are more likely to be persuaded by their own thoughts and words.10
Occasionally, patients see how both sides of a behavior change could positively or negatively impact their lives. Although patient ambivalence is a normal aspect of preparing for behavior change, initiating a “change talk” strategy may help the individual overcome ambivalence based on his or her values and interests.10 Change talk occurs when the individual’s statements identify what behavior needs to change. It is critical for practitioners to recognize when this transition takes place, as it allows clinicians to notify patients they may already be considering a change.10 The key point is that rather than being swayed by clinical instructions, patients are more likely to be persuaded by their own thoughts and words.10
Change talk helps patients evoke their own plans to change. The importance ruler strategy is useful in gauging patients’ perceptions of the importance of behavior changes, and their confidence in being able to change. The importance ruler is determined by posing an evocative question and asking the patient to assess his or her level of importance, as well as confidence in achieving a specific change.10 This helps the patient identify his or her readiness to change and may spur the decision to implement changes.11 Another strategy is asking the patient to elaborate on his or her decision; the clinician then asks, “What else?” to evoke an intrinsic motivation toward positive change.10
BRIEF MOTIVATIONAL INTERVIEWING
A derivative of MI, brief MI is ideal for health care providers who have limited time (eg, 5 minutes to 10 minutes) with patients.11 It focuses on the collaborative spirit of MI by allowing the patient to think about the benefits and challenges of change.11 The key elements of brief MI include assessing motives, enhancing awareness, and supporting change.7 During this counseling, the clinician and patient exchange information about the proposed change. The goal is to reduce the patient’s resistance to change while building rapport and supporting his or her goals.11
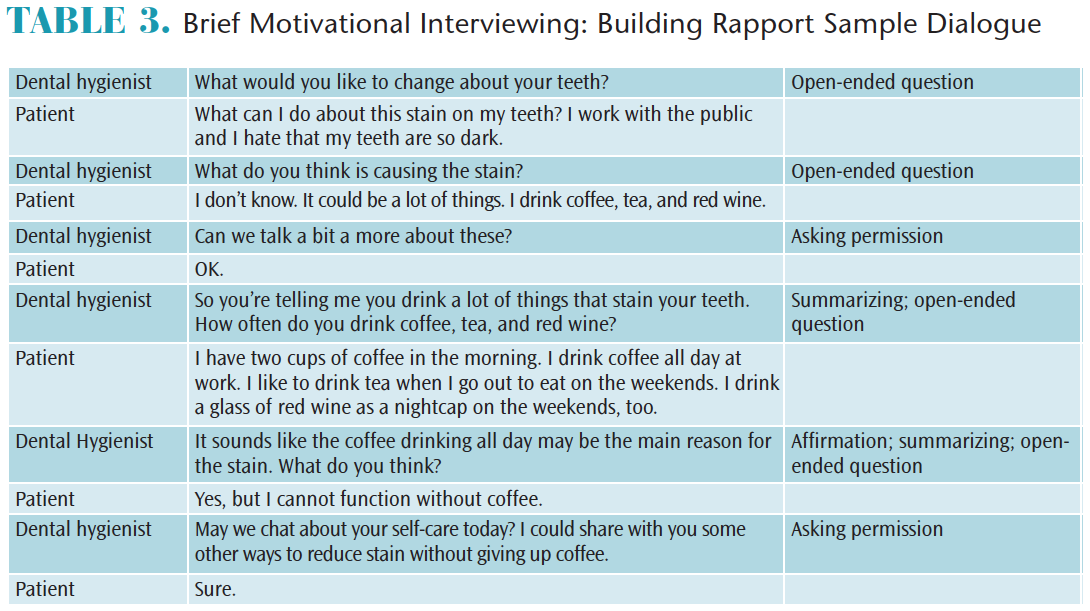
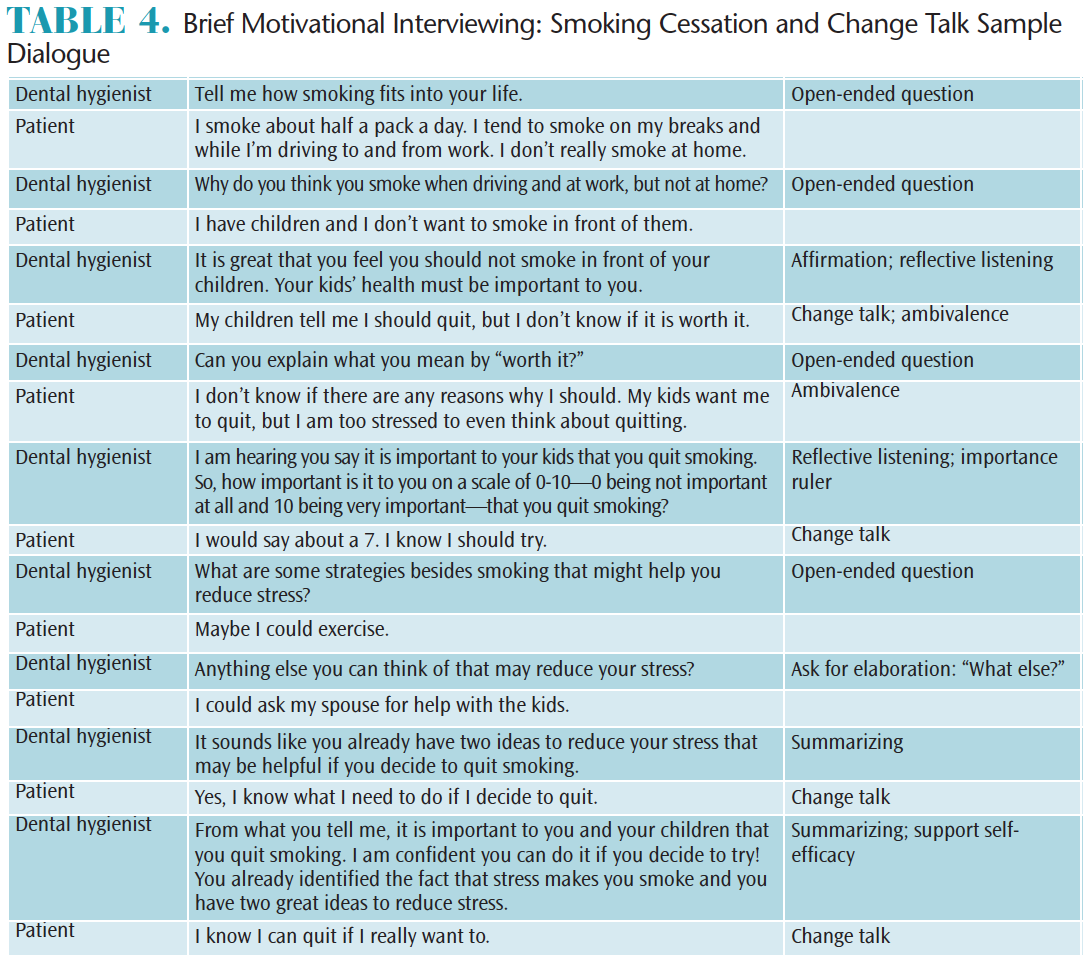
Table 3 demonstrates the development of a clinician-patient partnership via a sample conversation about coffee-stained teeth. Note the dental hygienist does not tell the patient what he or she should do or judge the patient; rather, the clinician focuses on developing rapport. Table 4 is an example of a brief MI smoking-cessation dialogue with a patient who is demonstrating ambivalence to change. Note the dental hygienist uses change talk strategies to evoke the patient’s ideas concerning change.
EDUCATION AND TRAINING
Beyond familiarity with its core principles, clinical training is required to achieve competence in MI.14,16 This includes instruction, coaching, and performance feedback. With the goal of long-term sustainability of behavior changes,14,19 training in brief MI principles and methods enhances the clinician’s knowledge, skills, and confidence in applying this strategy to patient care.20
MI is an evidence-based approach that provides information, education, and support for health-driven behavior changes.5–8,10,11,12,14 Dental hygiene programs are now revising their curricula to incorporate MI instruction.12,14 Training is also available for practicing dental hygienists. Continuing education courses and the Motivational Interviewing Network of Trainers (MINT) are helpful resources for those interested in incorporating MI into practice.21 MINT’s goal is to offer continuing education, skills, resources, communication, publications, and practice opportunities for health care professionals.21
Research suggests that MI training should involve a multimodal approach that includes coaching and feedback that help ensure long-term retention of skills.16,22 Performance feedback during MI training is most effective when it is focused on knowledge and skills that match the learning goal, provided in a timely manner, and connected to practice opportunities to improve performance.23
A fundamental goal of coaching is to gain skill with the support of positive reinforcement; this often involves role-playing to allow clinicians to practice OARS strategies that will elicit change conversations that foster and strengthen individual awareness of motives.14,16,17,19
CONCLUSION
A primary role of the dental hygienist is preventing disease and promoting oral and systemic health. Effective counseling can help patients prevent oral and systemic diseases and enhance health and well-being.1,2 The literature supports the efficacy of MI as an evidence-based, patient-centered, collaborative approach to drive positive changes in behavior and lifestyle.10 In addition, brief MI is practical for implementation in dental settings due to time limitations.11
As increasing emphasis is placed on disease prevention, dental hygienists should strengthen their skills in patient education and counseling.1,2 MI and brief MI strategies can be used to effectively develop a collaborative rapport with patients to support behavior changes that can enhance oral and systemic health.
References
- United States Department of Health and Human Services. Oral health in America: A Report of the Surgeon General, Executive Summary. Available at: nidcr.nih.gov/DataStatistics/SurgeonGeneral/Report/ExecutiveSummary.htm. Accessed February 27, 2017.
- Rhea M, Bettles C. Dental Hygiene at the Crossroads of Change: Environmental Scan 2011–2021. Available at: adha.org/resources-docs/7117_ADHA_Environmental_Scan.pdf. Accessed February 27, 2017.
- Healthy People 2020. Determinants of Health. Available at: healthypeople.gov/2020/about/foundation-health-measures/Determinants-of-Health. Accessed February 27, 2017.
- Healthy People 2020. Topics and Objectives—Oral Health. Available at: healthypeople.gov/2020/topics-objectives/topic/oral-health. Accessed February 27, 2017.
- Catley D, Goggin K, Lynam I. Motivational interviewing and its basic tools. In: Ramseier CA, Suvan JE. Health Behavior Change in the Dental Practice. Ames, Iowa: Wiley-Blackwell; 2010:59–92.
- Gobat N, Bogle V, Lane C. The challenge of behavior change. In: Ramseier CA, Suvan JE. Health Behavior Change in the Dental Practice. Ames, Iowa: Wiley-Blackwell; 2010:13–34.
- Koerber A. Brief interventions in promoting health behavior change. In: Ramseier CA, Suvan JE. Health Behavior Change in the Dental Practice. Ames, Iowa: Wiley-Blackwell; 2010:93–112.
- Lane C. Communication and health behavior change counseling. In: Ramseier CA, Suvan JE. Health Behavior Change in the Dental Practice. Ames, Iowa: Wiley-Blackwell; 2010:35–58.
- Mason P, Butler CC. Health Behavior Change, A Guide for Practitioners. 2nd ed. Edinburgh, Scotland: Elsevier Churchill Livingstone; 2010:221.
- Miller WR, Rollnick S. Motivational Interviewing, Helping People Change. 3rd ed. New York: Guilford Press; 2013:482.
- Rollnick S, Mason P, Butler C. Health Behavior Change, A Guide for Practitioners. Edinburgh, Scotland: Churchill Livingstone; 1999:225.
- Bray KK, Catley D, Voelker MA, Liston R, Williams KB. Motivational interviewing in dental hygiene education: curriculum modification and evaluation. J Dent Educ. 2013;77:1662–1669.
- Brand VS, Bray KK, MacNeill S, Catley D, Williams K. Impact of single-session motivational interviewing on clinical outcomes following periodontal maintenance therapy. Int J Dent Hyg. 2013;11:134–141.
- Croffoot C, Krust Bray K, Black MA, Koerber A. Evaluating the effects of coaching to improve motivational interviewing skills of dental hygiene students. J Dent Hyg. 2010;84:57–64.
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: Toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–395.
- Miller WR, Yahne CE, Moyers TB, Martinez J, Pirritano M. A randomized trial of methods to help clinicians learn motivational interviewing. J Consult Clin Psychol. 2004;72:1050–1062.
- Westra HA, Aviram A. Core skills in motivational interviewing. Psychother (Chic). 2013;50:273–278.
- Schwalbe CS, Oh HY, Zweben A. Sustaining motivational interviewing: a meta-analysis of training studies. Addiction. 2014;109:1287–1294.
- Miller WR, Rollnick S, Butler BC. Motivational Interviewing in Healthcare. New York: Guilford Press; 2008:210.
- Hinz JG. Teaching dental students motivational interviewing techniques: analysis of a third-year class assignment. J Dent Educ. 2010;74:1351–1356.
- Edwards EJ, Stapleton P, Williams K, Ball L. Building skills, knowledge and confidence in eating and exercise behavior change: brief motivational interviewing training for healthcare providers. Patient Educ Couns. 2015;98:674–676.
- About MINT: Motivational Interviewing Network of Trainers. Available at: motivationalinterviewing.org/about_mint. Accessed February 27, 2017.
- Ambrose SA, Bridges MW, DiPietro M, Lovett MC, Norman MK. What kinds of practice and feedback enhance learning? In: How Learning Works: Seven Research-Based Principles for Smart Teaching. San Francisco: John Wiley & Sons Inc; 2010:121–152.
From Dimensions of Dental Hygiene. May 2017;15(5):54-57.



