Maintaining the Beauty and Longevity of Esthetic Restorations
Basic principles of care and maintenance.
This course was published in the June 2009 issue and expires June 2012. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the role of the dental hygienist in maintaining esthetic restorations.
- Discuss self-care recommendations for patients with esthetic restorations.
- Discuss the indications and contraindications for finishing and polishing.
The use of tooth-colored or esthetic restorative materials has increased over the past decade.1 Specifically, the use of direct posterior resin restorations has increased in popularity as a functional and esthetic alternative to amalgam.2 The placement of esthetic restorations is technique sensitive and requires adequate finishing and polishing. Improperly finished and polished restorations can result in excessive biofilm accumulation, gingival irritation, increased surface staining, and poor or suboptimal esthetics of the restored teeth.3
Patients with esthetic restorations have special maintenance needs that should be addressed during routine dental hygiene recare appointments. The dental hygienist can play a significant role in increasing the life span of esthetic restorations, promoting periodontal health, and reducing the incidence of recurrent caries through maintenance procedures such as finishing, polishing, self-care education, and correct dental hygiene instrumentation. Dental hygienists can accomplish these aspects of care in a relatively short amount of time and incorporate them into other comprehensive dental hygiene services during selected appointments.4
Esthetic Materials Review
Tooth-colored restorative dental materials are widely used to meet patients’ esthetic demands. New restorative materials are being introduced at a staggering rate and maintaining awareness of these new materials is key to the dental hygienist’s ability to properly care for and maintain restorations that include those materials. Composite, ceramic, and porcelain materials require special attention during dental hygiene care to ensure the continued esthetic and functional quality of the restorations.
Veneers can be divided into two major categories: indirect and direct. Indirect veneers are custom made and fabricated in a dental laboratory; composed of porcelain, ceramic, or composite; and are bonded into place with a free-flowing composite resin.6 Direct veneers are made in the mouth using composite and can stain more easily than indirect veneers.
Ceramics are composed of compounds containing metal in addition to nonmetal compounds, which yield stable substances that are strong, hard, brittle, and inert conductors of thermal and electric energy.4 Porcelain has a ceramic composition based on silica, aluminum oxide, and potassium oxide. Ceramics are used to fabricate ceramometal crowns and fixed partial dentures, all-ceramic crowns, inlays, onlays and veneers, and ceramic denture teeth.5
Professional Maintenance
Recognizing esthetic restorations can be challenging, especially with the new and improved hybrid and nanofilled materials in use today. Reviewing charting records, radiographs, and records of services is important in determining if restorations are present. If the patient is new to the practice, using magnification, exploration (tactile), air, and radiographs can assist the dental hygienist in determining any existing esthetic restorations.
The restorations should be evaluated for stain, marginal integrity, wear, surface roughness, recurrent caries, biofilm or calculus deposit accumulation, and gingival tissue health surrounding the restoration. The cavosurface margin—the area formed by the cavity wall and the external tooth surface—should be examined to identify areas of overfill (flash), voids (open margins), submarginal anatomy (ditching), or surface roughness. The overall contour of the restoration needs to be assessed the use of heavier pressure, thereby increasing the chance of slipping that can result in ditching or scratching the restoration surface. Thus, curets should be sharpened at the first sign of dullness.
The use of ultrasonic and sonic instruments on restorative materials is a concern due to the mechanical energy produced on the tooth surface. Therefore, contacting any restorative materials with ultrasonic inserts should be avoided. Ultrasonic inserts can scratch restorations, loosen the bond strength in composite restorations, and leave black streaks from the removal of metal from the insert onto the restoration. Ultrasonic instrumentation may be used during care but precision thin inserts on a low power setting with short brush-like strokes apical to any restoration margin should be used.
The use of air-powder polishing using sodium bicarbonate powder or aluminum trihydroxide can pit and scratch esthetic restorations.7-9 As a result, practitioners using air polishing devices for prophylaxis procedures should exercise caution in the area of esthetic restorations and incorporate selective polishing procedures to avoid unnecessary damage. If rubber cup selective polishing is used, avoid using medium or coarse prophy pastes. Aluminum oxide paste, aluminum-coated disks, one step diamond micro-polisher cups/points, paste-free polishing cups, or low abrasive toothpastes may be used instead (Table 3).
Professionally applied fluoride applications are frequently used during dental hygiene recare appointments. However, some esthetic restorative materials may be damaged or altered by the use of acidulated phosphate or stannous fluoride. Acidulated phosphate fluoride can break down the filler particles in composite restorations and etch porcelain; stannous fluoride has staining properties. Thus, the use of a neutral sodium fluoride or fluoride varnish is recommended.
Table 2. Determining the Status of Restorations
Indications for Finishing and Polishing
- Light to moderate stain
- Excess flash, rough margins, or Class I or Class II overhangs
- Surface imperfections
- Premature occlusal contacts
- Minor defects or anatomy recontouring Indications for Repair
- Slight voids in material
- Open cavosurface margin (< 1 mm)
- Slight fracture in marginal ridge or incisal edge Indications for Replacement
- Heavy or intrinsic stain
- Class III overhang (> one-half of embrasure)
- Open cavosurface margin (>1 mm)
- Recurrent caries
- Open contact or broken marginal ridge
FINISHING AND POLISHING COMPOSITES
Finishing involves removing any irregularities around the cavosurface margin, defining anatomic contours, smoothing away surface roughness, and overhang removal. The purpose of polishing is to remove scratches from the surface of a restoration and obtain a smooth, light-reflective luster.10 The provision of all dental hygiene and expanded function procedures should always follow the scope of practice regulations established by each individual state. Some finishing and polishing procedures may not be allowed under certain state dental hygiene practice acts.
A variety of products are available for finishing and polishing that contain aluminum oxide, carbide compounds, diamond abrasives, silicon dioxide, sirconium oxide, and sirconium silicate.10 Some abrasive products are designed for both finishing and polishing. These products can be used with composite and ceramic materials using a friction grip slow speed handpiece. Heat generation during any finishing and polishing procedures must be reduced by using intermittent pressure, water, and air.
Several different techniques are discussed throughout the literature. Rotary attachments should be selected based on the amount of finishing and polishing required. The necessary armamentarium includes: mouth mirror, explorer, articulating paper, isolation materials, air-water syringe, dental floss, friction grip slow speed handpiece, carbide finishing burs, abrasive disks, finishing strips, and finishing and polishing points (Figure 1). A basic sequence should be followed beginning with the proximal surfaces, occlusal surface, cavosurface margin, and facial and lingual surfaces.
Excess material found in the proximal region of the tooth causes excessive biofilm accumulation, which results in gingival inflammation and over time can cause destruction of the periodontium. Overhangs on composite restorations may be removed using a #12 (curved) scalpel blade, a gold knife, or a power-driven anti-rotational handpiece using flat one-sided diamond coated lamineer tips (Figure 2). Using a flat lamineer tip, the excess resin material can be easily filed and shaped without damaging the tooth or restoration.11 Margination procedures restore the anatomical shape of the tooth, reduce biofilm accumulation, and improve patient self-care.
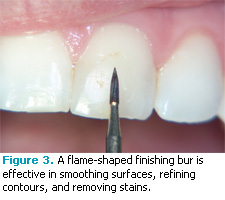
For occlusal surfaces football-shaped or round finishing burs can be used to remove any premature contact points, remove flash, and refine anatomy. The use of abrasive disks and flame-shaped finishing burs is effective to smooth surfaces, refine contours, and remove stain from the buccal/facial and lingual surfaces (Figure 3).
The polishing stage requires the use of finer abrasives in the form of disks, strips, brushes, or rubberized points. Aluminum oxide-coated strips can be used to polish the interproximal areas. To obtain a high gloss and smooth finish, abrasives must be used in sequential order beginning with the coarsest abrasive and finishing with the finest abrasive.
 |
 |
SELF-CARE
Patients are often not aware of their individual responsibility in the maintenance of esthetic restorations. Practitioners must provide individualized instruction based on the needs of the patient. Individualized self-care should include discussion on bacterial biofilm removal methods, dietary assessments, and recare intervals.
Toothbrushing should incorporate the use of a soft bristle brush and gentle sulcular brushing (modified Bass method). Abrasive toothpastes should be avoided. Proximal cleaning devices should be selected based on the size of gingival embrasures and may include floss, nylon-coated soft interdental brushes, soft triangular wooden tips, or toothpicks used in a handle. The use of carbamide peroxide and chlorhexidine- gluconate- and alcohol-containing mouthrinses on composite restorations softens and stains the material, reduces the gloss, and alters the color.12-14 Therefore, the use of alcohol-free mouth rinses should be recommended in most instances. However, the number of existing composite restorations and periodontal conditions should be considered.
Foods and beverages may affect the color stability of composite resin restorative materials. Tobacco products, coffee, tea, blueberries, red wine, and other similar substances can discolor composites. Patients should avoid or reduce the amount of exposure to these triggers. Also, patients should be reminded about the detrimental effects of chewing hard objects such as candy, ice, pens, and pencils.
Successful maintenance of esthetic restorations is a collaborative effort between the patient and practitioner. The dental hygienist is instrumental in maintaining these restorations through evaluation, finishing and polishing procedures, and education. Developing an esthetic restoration maintenance program into practice will not only increase the longevity of these restorations but will increase patient satisfaction and quality of life.
REFERENCES
- Sadawsky SJ. An overview of treatment considerations for esthetic restorations: A review of the literature. J Prosthet Dent. 2006;96:433-442.
- Morgan M. Finishing and polishing of direct posterior resin restorations. Pract Proced Aesthet Dent. 2004;16:211-217.
- Jefferies SR. The art and science of abrasive finishing and polishing in restorative dentistry. Dent Clin North Am. 1998;42:613-627.
- McGuire MK, Miller L. Maintaining esthetic restorations in the periodontal practice. Int J Periodont Rest Dent. 1996;16:231-239.
- Powers JM, Sakaguchi RL. Craig’s Restorative Dental Materials. 12th ed. St. Louis: Mosby Elsevier; 2006.
- Albers HF. Tooth-colored Restoratives: Principles and Techniques. 9th ed. Hamilton, ON: BC Decker; 2002.
- Gutmann MS, Marker VS, Gutmann JL. Restoration surface roughness after air-powder polishing. Am J Dent. 1993;6:99-102.
- Carr MP, Mitchell JC, Seghi RR, Vermilyea SG. The effect of air polishing on contemporary esthetic restorative materials. Gen Den. 2002;50:238-241.
- Johnson WW, Barnes CM, Covey DA, Walker MP, Ross JA. The effects of a commercial aluminum airpolishing powder on dental restorative materials. J Prosthodont. 2004;13:166-72.
- Jefferies SR. Abrasive finishing and polishing in restorative dentistry: A state-of-the art review. Dent Clin N Am. 2007;51:379-397.
- Strassler HE. Clinical applications of the Profin directional reciprocating handpiece. Dental Products Report. 2002;122-126.
- Penugonda B, Settembrini L, Scherer W, Hittelman E. Alcohol-containing mouthwashes: Effect on composite hardness. J Clin Dent.1994;5:60-62.
- Celik C, Yuzugullu B, Erkut S, Yamanel K. Effects of mouth rinses on color stability of resin composites. Eur J Dent. 2008;2: 247-253.
- Gurgan S, Cakir FY. The effect of three different mouthrinses on the surface hardness, gloss and colour change of bleached nano composite resins. Eur J Prosthodont Rest Dent. 2008;16:104-108.
From Dimensions of Dental Hygiene. June 2009; 7(6): 38-41.