
Maintaining Implant Health
Patients with aggressive periodontitis are at increased risk of implant complications, but an effective peri-implant tissue maintenance protocol can help improve
outcomes.
This course was published in the August 2012 issue and expires August 2015. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the risks of placing implant-supported restorations in patients with aggressive periodontitis.
- Detail the research conducted on implant success and failure in patients with aggressive periodontitis.
- Identify the restorative options for patients with aggressive periodontitis.
- Explain the proper implant maintenance protocol for patients at increased risk of implant complications.
In the past, patients with aggressive periodontitis—a form of periodontal disease that affects otherwise healthy individuals and leads to rapid attachment loss and bone destruction—were not considered good candidates for implant-supported restorations. With advancements in treatment and research, implant therapy is widely used today, and it can be implemented successfully in a wide range of patients, including those with aggressive periodontitis.
Aggressive periodontitis is more common among younger people than older adults, and it is not typically related to other systemic health problems. Although disease progression is rapid, patients with aggressive periodontitis often present with low levels of gingival inflammation and little calculus or plaque on tooth surfaces. Outcomes can be dire, as patients with aggressive periodontitis frequently experience severe attachment loss of affected teeth. When these teeth are replaced, the treatment of choice is often implant-supported restorations. Using this technique, missing teeth can be replaced without involving the remaining dentition. Moreover, implant-supported restorations can provide occlusal support, thus reducing occlusal forces on the remaining dentition.
Placing implant-supported restorations in patients with aggressive periodontitis is not without risk, however, as these individuals are at increased risk of peri-implantitis. While recognized experts have described peri-implantitis as a local nuisance event and not a disease process as recently as 2009,1,2 a growing body of evidence indicates that peri-implantitis is a disease entity and patients with aggressive periodontitis at the time of implant placement are more prone to exhibiting these lesions.3-9


WHAT THE RESEARCH SAYS
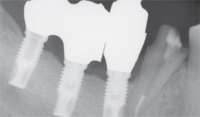
The evidence shows that patients with advanced and chronic periodontitis are at greater risk of implant complications. In 1991, Rosenberg et al10 evaluated the microflora associated with osseointegrated implants. Failed implants were retrieved from both partially dentate and fully edentulous patients. Implant failure was attributed to infection in the cases that exhibited bleeding, suppuration, high scores on plaque and gingival indices, and granulomatous tissue upon surgical removal. In the cases that did not exhibit these symptoms, the failures were considered traumatic. Distinct differences were found in the microbiota from the two types of failures. The bacteria found in the infectious failures contained more spirochetes and motile rods. Figure 1 and Figure 2 illustrate typical clinical presentations of the two types of failures. Figure 1A shows swelling and inflammation of the peri-implant soft tissues and Figure 1B demonstrates that once removed, the implant is covered with granulomatous tissue. Figure 2A and Figure 2B illustrate traumatic failure where intraoral tissues appear relatively healthy and implants removed appear “clean.”


In 2003, Karoussis et al8 reported on longterm implant prognosis in patients with and without a history of chronic periodontitis. They found that the survival rate for patients with a history of chronic periodontitis was 90.5%, and for those without a history of chronic periodontitis, the rate was 96.5%. Additionally, more biological problems, such as bleeding on probing and peri-implant bone loss, were demonstrated among patients with a history of chronic periodontitis. More recently, Roos JansOEker et al3-5 performed a retrospective study of 218 patients with 1,057 implants 9 years to 14 years post restoration.

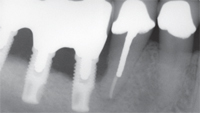
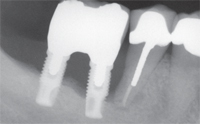
They found a significant relationship between implant loss and periodontal bone loss in the remaining teeth at the time of implant placement. Early implant failures were attributed to causes other than peri-implantitis, and later failures (after delivery of definitive prostheses) were attributed to peri-implantitis. Figure 3A to Figure 3E provide an example of the progressive bone loss surrounding implants in a patient with

RESTORATIVE OPTIONS
When implant therapy was in its infancy, clinicians were most often concerned with mechanical issues, such as screw loosening, mechanical breakage of restorations, or breakage of implant components after implant surgery.11,12 Many leaders in the field thought that implant-supported restorations were immune to the bacterial attacks in the oral environment because there were no calcified tissues to decay or periodontium to infect.1,2 While this theory may apply to people who have lost teeth due to trauma or caries, this is clearly not the case for patients with tooth loss caused by periodontal diseases. Effective implant maintenance is crucial to positive implant therapy outcomes among patients with periodontal diseases, especially aggressive periodontitis.
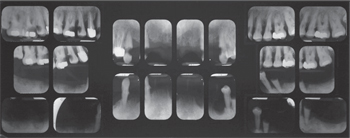
The prognosis for most or all of the teeth in patients with generalized aggressive periodontitis and advanced attachment loss is often poor. When treatment planning for these individuals, most clinicians will proceed with periodontal infection control, including scaling and root planing, followed by bacterial culture and systemic antibiotic therapy in conjunction with the intraoral use of chlorhexidine, sodium hypochlorite, and iodine. After this initial stage of treatment, a re-evaluation of periodontal infection and a reassessment of the prognosis are conducted. At this point, the dentition is often deemed nonmaintainable due to poor function and poor esthetics.13 Hence, two restorative options are available: removable prosthesis (occasionally with some type of implant-supported overdenture) or implant-supported fixed restoration. Either option provides oral hygiene challenges for both patients and dental hygienists. The contours of the replaced teeth, as well as the analogs used to improve esthetics of lost hard and soft tissues, hinder oral hygiene access and maintenance (Figure 4 through Figure 7).


MAINTENANCE PROTOCOL
Once these restorations are placed, the patient must undergo a strict oral hygiene regimen at home and maintain a rigid 3-month interval maintenance program. Any signs of increased probing depth, bleeding on probing, and peri-implant mucositis must be actively investigated. A radiograph should be taken to evaluate any peri-implant bone loss. When bleeding on probing and mucositis are detected, effective self-care must be re-enforced. Submucosal mechanical plaque control and submucosal application of local antiseptic agents, such as iodine, sodium hypochlorite, and chlorhexidine, or local delivery antibiotics, should be initiated, and a re-evaluation should be carried out after 1 week to 2 weeks.14 If these steps fail to control mucosal inflammation, bacterial sampling and systemic antibiotic therapy may be indicated when putative periodontal pathogens and/or enteric rods are detected, especially if peri-implant bone loss is evident. Surgical mucosal contouring and submucosal debridement may also be considered to manage persistent peri-implant mucositis.



A consensus on best practices for the treatment of peri-implant bone loss has not yet been reached, but common sense dictates that a conservative approach should be implemented initially, followed by resective therapy if the first approaches fail. Resective procedures to eliminate soft tissue pockets can be disfiguring.
Conservative approaches range from irrigation with saline to the use of lasers. Some of these treatments are supported by animal studies, while others are reported in case series or anecdotally.15–19 If no treatment is performed, the peri-implant bone loss will proceed, eventually causing loss of the implant (Figure 3A through Figure 3E).

CONCLUSION
Dental restoration of patients suffering from aggressive periodontitis can be predictably completed with implant-supported or implant-assisted prostheses. There is a higher incidence, however, of peri-implant diseases and less favorable long-term survival rate among this population when compared to patients without a history of aggressive periodontitis. In view of current information, any patient with aggressive periodontitis (or severe forms of chronic periodontitis) who is subsequently restored with dental implants should be considered at high risk of peri-implant diseases compared to patients who have lost teeth due to caries or trauma. A rigid 3-month maintenance protocol should be implemented when signs mucositis are detected.
This information originally appeared in the Journal of the California Dental Association and is reprinted with permission.
REFERENCES
- Zarb GA. On manufactured dental conditions. Int J Prosthodont. 2009;22:117.
- Albrektsson T, Brunski J, Wennerberg A. “A requiem for the periodontal ligament” revisited. Int J Prosthodont. 2009;22:120–122.
- Roos-Jansåker AM, Lindahl C, Renvert H, Renvert S. Nine- to fourteen-year follow-up of implant treatment. Part I: implant loss and associations to various factors. J Clin Periodontol. 2006;33:283–289.
- Roos-Jansåker AM, Lindahl C, Renvert H, Renvert S. Nine- to fourteen-year follow-up of implant treatment. Part II: presence of peri-implant lesions. J Clin Periodontol.2006;33:290–295.
- Roos-Jansåker AM, Lindahl C, Renvert H, Renvert S. Nine- to fourteen-year follow-up of implant treatment. Part III: factors associated with peri-implant lesions. J Clin Periodontol. 2006;33:296–301.
- Renvert S, Roos-Jansåker AM, Lindahl C, Renvert H, Rutger Persson G. Infection at titanium implants with or without a clinical diagnosis of inflammation. Clin Oral Implants Res. 2007;18:509–516.
- Karoussis IK, Müller S, Salvi GE, Heitz-Mayfield LJ, Brägger U, Lang NP. Association between periodontal and peri-implant conditions: a 10-year prospective study. Clin Oral Implants Res. 2004;15:1–7.
- Karoussis IK, Salvi GE, Heitz-Mayfield LJ, Brägger U, Hämmerle CH, Lang NP. Long-term implant prognosis in patients with and without a history of chronic periodontitis: a 10-year prospective cohort study of the ITI Dental Implant System. Clin Oral Implants Res. 2003;14:329–339.
- De Boever AL, Quirynen M, Coucke W, Theuniers G, De Boever JA. Clinical and radiographic study of implant treatment outcome in periodontally susceptible andnonsusceptible patients: a prospective longterm study. Clin Oral Implants Res. 2009;20:1341–1350.
- Rosenberg ES, Torosian JP, Slots J. Microbial differences in 2 clinically distinct types of failures of osseointegrated implants. Clin Oral Implants Res. 1991;2:135–144.
- McGlumphy EA, Mendel DA, Holloway JA.Implant screw mechanics. Dent Clin North Am. 1998;42:71–89.
- Gealh WC, Mazzo V, Barbi F, Camarini ET. Osseointegrated implant fracture: causes and treatment. J Oral Implantol. 2011;37:499–503.
- Wu AY, Chee W. Implant-supported reconstruction in a patient with generalized aggressive periodontitis. J Periodontol. 2007;78:777–782.
- Emrani J, Chee W, Slots J. Bacterial colonization of oral implants from nondental sources. Clin Implant Dent Relat Res. 2009;11:106–112.
- Roos-Jansåker AM, Renvert S, Egelberg J. Treatment of peri-implant infections: a literature review. J Clin Periodontol. 2003;30:467–485.
- Renvert S, Roos-Jansåker AM, Claffey N.Non-surgical treatment of peri-implant mucositis and peri-implantitis: a literature review. J Clin Periodontol. 2008;35(Suppl):305–315.
- Albouy J-P, Abrahamsson I, Persson LG, Berglundh T. Spontaneous progression of ligatured induced peri-implantitis at implants with different surface characteristics. Anexperimental study in dogs II: histological observations. Clin Oral Implants Res.2009;20:366–371.
- Albouy J-P, Abrahamsson I, Persson LG Berglundh T. Spontaneous progression of peri-implantitis at different types of implants. An experimental study in dogs. I: clinical and radiographic observations. Clin Oral Implants Res. 2008;19:997–1002.
- Albouy J-P, Abrahamsson I, Persson LG, Berglundh T. Implant surface characteristics influence the outcome of treatment of peri-implantitis: an experimental study in dogs. J Clin Periodontol. 2011;38:58–64.
From Dimensions of Dental Hygiene. August 2012; 10(8): 24-27.



