Laser Therapy Basics
How lasers work and what they are used for in the dental operatory.
This course was published in the January 2011 issue and expires January 2014. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
1. Describe the
basic principles of how lasers work.
2. Discuss how
dental hygienists can use laser therapy.
3. Describe how the
different types of lasers are used in the dental
setting.
Technological advances continue to impact the practice of dentistry. The use of lasers is an important facet of patient treatment. However, dental practitioners must understand the basic principles, the evidence-based research on their use, laser safety practices, and varying state laws to successfully integrate their use into practice.
LASER BASICS
Laser is an acronym for “light amplification by stimulated emission of radiation.” Based on a quantum mechanical effect, lasers concentrate high photon energies into an intense narrow beam of monochromatic, electromagnetic radiation.1 Energy beam photons are collimated into a focused nondivergent beam of light that is absorbed by tissues, producing a photothermal, photomechanical, or photochemical reaction.2 Energy beams interact with the targeted tissue and effect tissue change by being reflected, absorbed, scattered, or transmitted.3 Beam splitters or mirrors are used to capture the particular portion of the laser beam needed to perform a procedure. The monochromatic nature and high degree of collimation distinguishes laser light from ordinary light (which reflects in many directions) and each laser wave is identical in size. The nondivergent nature of the laser beam affords opportunity for greater focus, precision, and accuracy during treatment procedures, minimizing the potential risk of adjacent tissue damage. Lasers used in dentistry typically range in wavelengths from 457 nanometers (nm) to 10,600nm.3 Wavelengths describe units in which the amplified light is measured: the horizontal distance from one wave to the next wave, in either nanometers or meters, depending on the amount of light production. Wavelengths and the absorbed energy reaction depend on the amount of heat emitted, and whether the waveform beam is continuous or pulsating. Different wavelengths are absorbed at varying rates by the target tissue and influence patient comfort, treatment efficacy, and clinicians’ ease of use. Because specific wavelengths affect tissues differently, more than one type of laser is needed for the different types of procedures. For example, hard tissue lasers have energy beams that penetrate hydroxyapatite as the waves are absorbed by calcium phosphate. In contrast, the energy produced with soft tissue lasers penetrates tissue while sealing blood vessels and nerve endings as the energy is absorbed by melanin and hemoglobin.
TYPES OF LASERS IN DENTISTRY
Diode, CO2 (carbon dioxide), Nd:YAG (neodymium-doped yttrium aluminum garnet), argon, ErCr:YSGG (erbium chromiumyttrium- scandium-gallium-garnet), and Er:YAG (erbium yttium-aluminum-garnet) are the most commonly used lasers in dentistry. Since each dental laser’s abilities are different, the dental practice’s goals and patient needs should be considered when determining which dental laser is right for the designated treatment (see Table 1).
The American Dental Association (ADA) recommends clinicians access the Food and Drug Administration (FDA) website at: www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMN/pmn.cfm for specific and current information about FDA-cleared indications for laser use in dentistry.4 All dental professionals who intend to use the laser need to review their states’ rules and regulations for certification requirements and safety regulations prior to use.
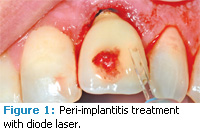
DIODE
The energy source of a diode laser is a semiconductor embedded in a crystal. The diode laser, often referred to as “the soft tissue laser,” is designed to reduce the amount of bacteria in a diseased pocket, as well as remove inflammatory products.5,6 Research has provided mixed results and further patient-based studies are needed to validate such claims.4,9 Diode wavelengths are absorbed by pigmented structures, such as hemoglobin and melanin, and work well in soft tissues. The light energy is transferred to heat, resulting in an instantaneous tissue reaction of warming, coagulation, and cell vaporization. This instantaneous reaction is termed ablation and results in minimal tissue bleeding. With the diode laser, soft tissue procedures can often be performed with slight discomfort requiring only minimal anesthesia.

Nd:YAG
The Nd:YAG is the first laser approved by the FDA for gingival sulcular debridement. Energy waves are absorbed in hemoglobin, blood components, and melanin. The Nd:YAG may be effective in the reduction of bacteria in diseased pockets and it creates excellent hemostasis, similar to the diode laser. The laser-assisted new attachment procedure (LANAP) uses the laser for removing and reducing gram-negative bacteria in the periodontal pocket, and also is purported to regenerate the attachment apparatus of the teeth: periodontal ligament, cementum, and alveolar bone. The ADA Council on Scientific Affairs suggests these results are promising, but more studies are needed to determine its safety and efficacy.4
Since both the diode and Nd:YAG lasers are attracted to pigment and hemoglobin, the beam tends to avoid interacting with root surfaces, which ensures no resultant root damage occurs during treatment. However, both the diode and the Nd:YAG lasers are contraindicated for calculus removal due to the amount of heat build-up that results when a dark deposit is located in the pocket.
CO2 LASER
Only used on soft tissue, the CO2 (carbon dioxide) laser is considered the most effective laser to control bleeding. It uses high wavelengths and is effective in cutting into tissues quickly and deeply. Oral surgeons and periodontists often favor this laser due to its proficiencies with tissues, especially for use with biopsy, frenectomy, and gingivectomy procedures.7 While controversial, some practitioners use the CO2 laser in surgical tissue procedures because of the strong hemostasis and bacterial reduction effects it produces. When the laser hits the tissues, a layer of carbon called char is left behind, which serves as a surgical dressing maintaining sterility and possibly improving healing of the surgical site.4,5 One disadvantage of the CO2 laser is that the wavelength is easily absorbed in hydroxyapatite and water so if the beam is not carefully placed, hard and soft tissues can be easily damaged.1
ERBIUM
Erbium-based lasers are used for hard tissue treatments. The energy with this laser is absorbed in hard tissues and water at a very low depth. They are used to perform cavity preparations and their use may reduce the need for anesthesia during treatment. Available in two forms: Er:YAG and ErCr:YSGG, the erbium laser may replace the dental drill in certain applications. Due to its shallow penetration, it has a decreased risk of internal pulpal damage from high temperatures when compared to other lasers.7 Because of high wavelengths, it easily cuts into hard structures and also has the ability to anesthetize a tooth, blocking sensory innervations, when the beam is held on the tooth for a few seconds at low wavelengths. For dental hygienists, the erbium laser can be used in sealant preparation because it can disinfect the tooth prior to sealant placement.
The ErCr:YSGG laser has the ability to work on hard tissues as well as soft tissues. The ErCr:YSGG laser is most noteworthy for sulcular debridement, decay removal, and treatment of oral lesions through ablation. And because it is less invasive than a scalpel when used for soft tissue surgeries, the need for anesthesia and sutures as well as post-operative sequelae are often reduced or eliminated.
Both erbium lasers have been successfully used for calculus removal, hemostasis, and pocket depth reduction.1 They may show potential for use in root debridement, and treatment may result in increased gains in clinical attachment levels over scaling and root planing alone.4 Caution must be used with erbium lasers because the beam is not completely selective and can remove root surface accretions and may place micro-irregularities in cementum.
ARGON
The low-powered argon laser is best suited for curing composite resins. A quicker curing time and improved bonding are reported advantages. The 514 nm argon laser is effective for soft tissue procedures because the wavelength is highly absorbed by pigmented tissue. It works well for labial and oral lesions with large vascular components. It provides excellent hemostasis and is considered a versatile laser since it can be used not only for curing but whitening, coagulation, and transillumination.
LASERS IN DENTAL HYGIENE
Prior to use, dental hygienists need to contact their state boards to determine if their states’ scope of practice allows for the use of lasers by dental hygienists. Dental hygienists typically use lasers for the following functions: sulcular debridement, reduction of subgingival bacterial loads, inflammation control, and hemostasis of bleeding.8 The goal is to promote healing and reduce pocket depth without reducing the height of the gingival crest via recession and tissue shrinkage.
The American Academy of Periodontology (AAP) released its “Statement on the Efficacy of Lasers in the Non-surgical Treatment of Inflammatory Periodontal Disease” in 2010.9 The statement asserts that the dental literature currently shows little to no benefit to the use of mechanical, chemical, or laser curettage in comparison to scaling and root planing alone. The AAP also states that the evidence is inconsistent in the ability of lasers to reduce subgingival microbial loads more than scaling and root planing alone. AAP does find the research on the use of erbium lasers in effective root debridement to be the most promising. Studies conducted in vitro have shown that the Er:YAG laser does remove calculus and negate endotoxin.10-13 However, the use of the Er:YAG laser in debridement may cause root surface damage because clinicians cannot see what they are lasing. Additional in vivo research is necessary to fully understand the role of lasers in the nonsurgical treatment of periodontitis.
SAFETY
Lasers can cause serious ocular injuries if used without appropriate eye safety devices. Laser damage to the eye causes biochemical and morphological changes, which lead to degeneration and loss of eye function.2 Damage may cause cataracts, headaches, exaggerated watering of the eyes, and swirling eye distortions known as floaters.14 Retinal damage from lasers may result in permanent eye problems in the form of diminished night vision, decreased ability to see color, and even blindness. The lack of pain receptors in the retina can result in practitioners being unaware of damage until it is very serious.
Protective eyewear must be selected based on the laser wavelength in use. Specific eyewear protection is needed for each laser wavelength and multi-wavelength lasers require the switching of safety lens during procedures.15 Opacity of the laser protective material known as optical density (OD) and the wavelength number for which it can be used must be permanently imprinted on laser safety goggles. Typically laser safety eyewear must have an OD of at least 4 for the particular laser emission.15 For clinicians with loupes, laser protective inserts or filters can be used. Protective eyewear for both the operator and patient should be in place before the laser is activated. A common mistake is lifting the eyewear during a procedure in an attempt to see tissues better; this can result in serious eye injury.
Laser therapy has the potential to provide a variety of treatments in oral health care. More evidence-based research is necessary to determine the status of laser use in the nonsurgical treatment of periodontal diseases.
ACKNOWLEDGMENT
The authors would like to thank Albert Konikoff, DDS, of Virginia Beach, Va, for the use of his clinical photos in this article.
REFERENCES
- Coluzzi DJ. Lasers for use in dental hygiene. Access. 2009;23(1):10-13.
- Knappe V, Frank F, Rohde E. Principles of lasers and biophotonic effects. Photomed Laser Surg. 2004;22:411-417.
- Cobb C. Lasers in periodontics: a review of the literature. J Periodontol. 2006;77:545-564.
- ADA Positions and Statements. Statement on Lasers in Dentistry. Available at: www.ada.org/1860.aspx. Accessed December 28, 2010.
- Neill ME, Mellonig JT. Clinical efficacy of the Nd:YAG laser for combination periodontitis therapy. Pract Periodontics Aesthet Dent. 1997; 9(6 Suppl):1-5.
- Schwarz F, Sculean A, Berakdar M, Georg T, Reich E, Becker J. Clinical evaluation of an Er:YAG laser combined with scaling and root planing for non-surgical periodontal treatment. A controlled, prospective clinical study. J Clin Periodontol. 2003;30:26-34.
- Yung F. The use of an Er:YAG laser in perio – dontal surgery: clinical cases with long term follow-up. J Laser Dent. 2009;17:13-20.
- Cozean C, Arcoria CJ, Pelagalli J, Powell GL. Dentistry for the 21st century? Erbium:YAG laser for teeth. J Am Dent Assoc. 1997;128;1080-1087.
- AAP Statement on the Efficacy of Lasers in the Non-surgical Treatment of Inflammatory Periodontal Diseases. Available at: www.perio.org/resources-products/pdf/laser-use_consensusstatement.pdf. Accessed December 31, 2010.
- Schwarz F, Aoki A, Becker J, Sculean A. Laser application in non-surgical periodontal therapy: A systematic review. J Clin Periodontol. 2008;35(Suppl 8):29-44.
- Schwarz A, Aoki A, Sculean A, Becker J. The impact of laser application on periodontal and peri-implant wound healing. Periodontol 2000. 2009;51:79-108.
- Ting CC, Fukuda M, Watanabe T, Aoki T, Sanaoka A, Noguchi T. Effects of Er,Cr:YSGG laser irradiation on the root surface: morphologic analysis and efficiency of calculus removal. J Periodontol. 2007;78:2156-2164.
- Folwaczny M, Aggstaller H, Mehl A, Hickel R. Removal of bacterial endotoxin from root surface with Er:YAG laser. Am J Dent. 2003;16:3-5.
- Bahn SL. Dental lasers: safe or sorry? Comp Cont Educ Dent. 1994;15:812-816.
- Piccione PJ. Dental laser safety. Dent Clin North Am. 2004;48:795-807.
From Dimensions of Dental Hygiene. January 2011; 9(1): 50, 52-53.






