JARUN011/ISTOCK/GETTY IMAGES PLUS
JARUN011/ISTOCK/GETTY IMAGES PLUS
Incorporating HIV Testing in the Dental Office
HIV testing in the dental setting can help patients get connected with the care they need to improve their long-term health outcomes.
This course was published in the January 2019 issue and expires January 2022. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the epidemiology of human immunodeficiency virus (HIV) in the United States and common terms used to measure infection.
- Describe the purpose and advantages of early HIV screening in the dental setting.
- Explain how oral health professionals can help improve the health of HIV-infected individuals and reduce HIV transmission.
Once an individual is infected with HIV, the amount of the virus in the blood can be measured and is reported as viral load. This is detected by measuring the amount of viral RNA in the blood and is stated in copies/per milliliter of blood. A higher viral load tends to lower the CD4 count. Therapy aimed at keeping the viral load at a low level allows the CD4 count to rise. Clinicians use antiretroviral therapy (ART) to treat HIV infections. Highly active antiretroviral therapy (HAART) is a term that indicates multiple drugs are being used for treatment. The goal of therapy is to keep the viral load of an HIV-infected person at reduced levels, which, in turn, promotes a rise in CD4 counts.4
Screening for diseases such as oral cancer is routine in dental practice, yet, according to information provided by the Mayo Clinic, there are no studies to prove that oral cancer screening saves lives.5 However, screening for HIV can lead to lifesaving treatment. The goal of HIV screening in the dental setting is to link HIV-infected individuals with proper medical care. If HIV screening shows a reactive result, the patient should be referred to a medical professional for confirmatory testing and diagnosis. In addition, individuals who are aware of their positive HIV status are less likely to engage in risky transmissive behaviors.6 This serves as an important preventive measure. Although HIV screening is not routinely done in dental offices, it can be an important tool—especially in the early stages of infection, when often there are no distinguishable signs or symptoms (Table 1). Linking HIV-positive individuals to medical treatment before symptoms occur is an important step in improving their health and reducing the probability of transmission. The use of ART and/or HAART has been significant in efforts to limit HIV transmission.7,8
![HIV Testing]() INCIDENCE AND PREVALENCE
INCIDENCE AND PREVALENCE
The United States Centers for Disease Control and Prevention (CDC) defines HIV incidence as the estimated number of people within a specific period who are newly infected with HIV, and HIV prevalence as the number of people within a given population who are living with HIV, whether they are diagnosed (independent of the time of diagnosis) or undiagnosed.9 Note that incidence includes only newly infected cases. It does not include cases in which the individual may have been infected prior to the specified period.
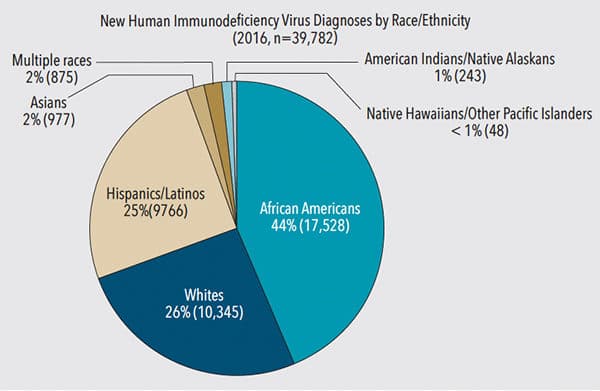
According to the CDC, in 2015 there were 1,122,900 adults and adolescents living with HIV, and in 2016 there were 39,782 newly diagnosed cases (some of which represent individuals who may have been infected long ago).10 These figures represent the US population as a whole, yet a different picture emerges when examining subpopulations. For example, African Americans are diagnosed in 44% of new HIV cases, but only represent 13.3% of the US population; whites comprise 26% of cases, and represent 76.9% of the US population; and Hispanics/Latinos make up 25% of new cases, but only represent 17.8% of the US population.11,12 When viewed in the context of their proportion of the US population, there is a comparatively disproportionate representation of newly diagnosed HIV cases among African Americans and Hispanics/Latinos (Figure 2).11
In order to reduce the incidence of HIV infection, it is important to know how many HIV-infected individuals remain undiagnosed, and identify ways to access and link them to medical treatment. Table 2 shows the percentage in each subgroup that is estimated to be undiagnosed.13
![HIV Testing]() ACCESS TO UNDIAGNOSED INDIVIDUALS
ACCESS TO UNDIAGNOSED INDIVIDUALS
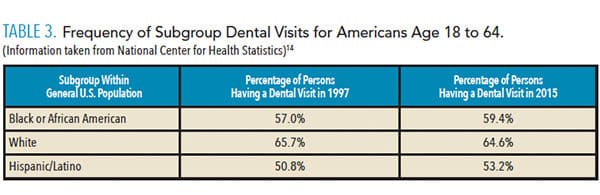
The National Center for Health Statistics documents the percentage of subpopulations that had a dental visit in 2016; these data are summarized in Table 3.14 The data show the percentage of individuals visiting the dentist increased among blacks/African Americans and Hispanics/Latinos between 1997 and 2015. As long as this trend continues to rise, it presents an opportunity for oral health professionals to access disproportionately affected HIV populations. The significance of this access is that it raises the prospect of positively impacting epidemiological estimates of HIV-infected individuals who remain undiagnosed. While the trend of having a dental visit among the white subgroup declined slightly (which may be due to multiple factors), it remains at a higher level than the African American and Hispanic/Latino subgroups. At 64.6%, there is still a good chance of reaching many undiagnosed white HIV-infected patients.
Many studies have been done regarding HIV infection and transmission. Most provide subcategories of HIV-infected individuals on the basis of age, race, gender, and geography; they also consider HIV infections that result from drug injections. Reducing the percentage of undiagnosed HIV-infected cases requires accessing all individuals from all subcategories. Because anyone may experience the need for oral health care, the dental office is a universal access point. Moreover, HIV screening in the dental space can be a safe and confidential starting point for linkage to care.
![HIV testing in the dental office]() SCREENING IN DENTAL PRACTICE
SCREENING IN DENTAL PRACTICE
Traditionally, HIV screening has not been viewed as a component of oral health care. However, a survey by Pollack et al15 showed positive associations between dentists’ willingness to provide HIV screening and patients’ and colleagues’ perceptions of the dental team’s role. This does not mean that HIV screening is a simple fit for the dental office. There are advantages and disadvantages of office practicality that need to be further assessed. That said, reducing the incidence of HIV-infected individuals is a major advantage.
Individuals with an acute stage of HIV infection have been shown to be more likely to transmit the virus than in later stages of infection.16 This makes early detection all the more critical from an epidemiological perspective. Rapid HIV tests yield results that will be termed either reactive or nonreactive. If the dental team finds a reactive response, referral to a medical professional for confirmatory tests can be made the same day.
Screening can be especially important in older adults.17 When performing a typical oral examination on an older adult, the oral health professional should be watchful for lesions that may be related to HIV infection. The dental setting is a good point of access to this population. The percentage of patients age 65 and older who had at least one dental visit in 2016 was 62.7%.14 In the case of HIV infection, early referral to medical care and initiation of ART is essential to prolong the life of older adults.
SURVIVAL AND TRANSMISSION
Advances in HIV drug research, along with better access to ART, are improving survival rates for HIV-infected individuals. This will increase the prevalence of HIV because more patients with HIV will live longer.18 The incidence of HIV is a reflection of recent transmission. This measurement should decrease if more newly infected individuals are linked to medical care through early HIV screening.
Regardless of population subcategory of HIV infection, two factors remain constant: the proportion of people who have a dental visit each year and the fact that ART is effective in extending life and reducing the probability of transmission. There is a significant difference in the chances of survival between an individual presenting for diagnosis who already has AIDS and someone presenting for diagnosis with an asymptomatic, newly diagnosed HIV infection. Early diagnosis leads to early treatment. A study by Samji et al19 indicates that the life expectancy for a 20-year-old HIV-positive patient on ART is nearly equal to that of the general population.
Vertical transmission is the term used for mother-to-child transmission. Early knowledge of HIV status is important for women who are pregnant or planning to become pregnant. According to a study by Siberry,20 it is possible to prevent vertical transmission with antiretroviral medication. The vertical transmission risk in the US can be reduced to 1% or 2% when a combination of antiretroviral drugs is routinely used during an infected woman’s pregnancy.20
CONCLUSION
The epidemiological significance of early HIV screening in the dental setting can be discussed in terms of prevalence and incidence. Infected individuals may be diagnosed or undiagnosed; for the former, treatment with ART or HAART has significantly impacted the length and quality of life. Thus, access to early HIV screening is vital for those who remain undiagnosed. The more time that elapses between infection and treatment, the more likely the infection will progress to a critical stage.
In addition, the probability of transmitting HIV is higher in the early stages of infection. The transmission rate can be reduced through prompt intervention. Early screening for HIV infection links infected individuals with medical care and treatment. The percentage of individuals who visit the dentist at least once per year is high enough to provide dental teams with access to a significant proportion of the subgroups that comprise the majority of new HIV diagnoses. The dental office is a venue with great potential to reach undiagnosed individuals. In this fashion, early screening in the dental setting and referral for confirmatory testing can have a positive impact on the epidemiology of HIV.
HUMAN IMMUNODEFICIENCY VIRUS: CLINICAL PRESENTATION
As part of a national response to the acquired immunodeficiency syndrome (AIDS) epidemic, the White House developed the National HIV/AIDS Strategy.21 These efforts have advanced the care provided to HIV-infected Americans. The introduction of highly active antiretroviral therapy, for example, has lowered the prevalence of oral manifestations of HIV infection by 30%.22 However, oral manifestations do sometimes present, and can be fungal, viral, bacterial, or neoplastic in nature. Common oral manifestations of HIV include the following.
- Erythematous candidiasis often presents on the dorsum of the tongue, but is also seen on the hard palate or soft palate. It is red and flat in appearance.
- Pseudomembranous candidiasis presents on the tongue and oral mucosa. It appears as white plaques and leaves a red or bleeding surface after being wiped off.
- Oral hairy leukoplakia is seen on the lateral borders of the tongue, and has a white corrugated appearance that cannot be wiped off.
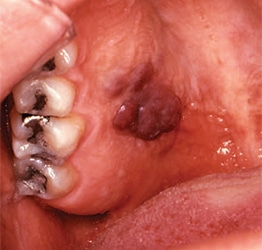
- Kaposi’s sarcoma appears as a macular or nodular lesion. It may or may not be ulcerated. These lesions can be red or even purple, and older lesions are darker (Figure 1).
REFERENCES
- United States Centers for Disease Control and Prevention. The Importance of HIV Testing. Available at: cdc.gov/healthcommunication/toolstemplates/entertainmented/tips/HivTesting.html. Accessed December 4, 2018.
- Bour S, Geleziunas R, Wainberg MA. The human immunodeficiency virus type 1 (HIV-1) receptor and its central role in promotion of HIV-1 infection. Microbiol Rev. 1995;59:63–93.
- U.S. Department of Veterans Affairs. CD4 Count (or T-cell count). Available at: hiv.va.gov/patient/diagnosis/labs-CD4-count.asp. Accessed December 4, 2018.
- Bello KJ, Mesner O, O’Bryan TA, et al. Factors associated with 10 years of continuous viral load suppression on HAART. BMC Infec Dis. 2016;16:351.
- Mayo Clinic. Oral Cancer Screening. Available at: mayoclinic.org/tests-procedures/oral-cancer-screening/about/pac-20394802. Accessed December 4, 2018.
- NAM aidsmap. Short-term risk reduction. Available at: aidsmap.com/Behaviour-change-after-testing/page/1746537/. Accessed December 4, 2018.
- U.S. Department of Health and Human Services. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents Living with HIV. Available at: https://aidsinfo.nih.gov/guidelines/html/1/adult-and-adolescent-arv/9/treatment-goals. Accessed December 4, 2018.
- National HIV Curriculum. Initial Evaluation. Available at: www.hiv.uw.edu/go/basic-primary-care/staging-initial-evaluation-monitoring/core-concept/all#page-title. Accessed December 4, 2018.
- United States. Centers for Disease Control and Prevention. Terms, Definitions, and Calculations Used in CDC HIV Surveillance Publications. Available at: cdc.gov/hiv/statistics /surveillance/terms.html. Accessed December 4, 2018.
- United States Centers for Disease Control and Prevention. HIV in the United States: At A Glance. Available at: cdc.gov/hiv/statistics/overview/ataglance.html. Accessed December 4, 2018.
- United States Centers for Disease Control and Prevention. Basic Statistics. Available at: cdc.gov/hiv/basics/statistics.html. Accessed December 4, 2018.
- United States Census Bureau. Quick Facts United States. Available at: census.gov/quickfacts/fact/table/US/PST045216. Accessed December 4, 2018.
- United States Centers for Disease Control and Prevention. Monitoring Selected National HIV Prevention and Care Objectives by Using HIV Surveillance Data-United States and six dependent areas, 2015. HIV Surveillance Supplemental Report. Available at: cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-supplemental-report-vol-22-2.pdf. Accessed December 4, 2018.
- United States Department of Health and Human Services. Health, United States, 2016; With Chartbook on Logn-Term Trends in Health. Available at: cdc.gov/nchs/data/hus/hus16.pdf. Accessed December 4, 2018.
- Pollack HA, Pereyra M, Parish CL, et al. Dentists’ willingness to provide expanded HIV screening in oral health care settings: Results from a nationally representative survey. Am J Public Health. 2014;104:872–880.
- Cornett JK, Kirn TJ. Laboratory diagnosis of HIV in adults: a review of current methods. Clin Infect Dis. 2013;57:712–718.
- Davis DH, Smith R, Brown A, Rice B, Yin Z, Delpech V. Early diagnosis and treatment of HIV infection: magnitude of benefit on short-term mortality is greatest in older adults. Age Ageing. 2013;42:520–526.
- Fettig J, Swaminathan M, Murrill CS, Kaplan JE. Global epidemiology of HIV. Infect Dis Clin North Am. 2014;28:323–337.
- Samji H, Cescon A, Hogg RS, et al. Closing the gap: increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PLoS One. 2013;8:12.
- Siberry GK. Preventing and managing HIV infection in infants, children, and adolescents in the United States. Pediatr Rev. 2014;35:268–286.
- What is the National HIV/Aids Strategy? Available at: hiv.gov/federal-response/national-hiv-aids-strategy/overview. Accessed December 4, 2018.
- Leao JC, Ribeiro CM, Carvalho AA, Frezzini C, Porter S. Oral complications of HIV disease. Clinics (Sao Paulo). 2009;64:459–470.
From Dimensions of Dental Hygiene. January 2019;17(1):40–43.