
Improving Health and Saving Lives
Statewide tobacco use quitlines are a valuable resource in the fight to eliminate tobacco use.
This is the first of two articles on smoking cessation. Part II will discuss nicotine addiction and the key elements of a more intensive, in-office cessation program that dental hygienists can implement.
.gif)
Smoking and periodontal disease are linked, with 50% of adult periodontitis cases in the United States attributed to cigarette smoking.4,5 Oral snuff and chewing tobacco use are associated with gingival recession.6 Tobacco use also significantly predicts failure of periodontal therapy and dental implants, impairs oral wound healing, and increases the risk of dental caries and a wide range of oral soft tissue changes.7-14Approximately 450,000 people in the United States die each year from tobacco-related diseases.1 Tobacco use accounts for more annual deaths than those caused by AIDS, alcohol, car accidents, homicides, drug overdose, and suicides combined.1 Tobacco use increases risk of heart disease, cancer, lung disease, and other illnesses and is associated with oral and pharyngeal cancer, accounting for more than 75% of deaths caused by these malignancies in the United States.2,3
Dental hygienists have the opportunity and responsibility to improve health and save lives by asking clients if they use tobacco, advising those who use to quit, and assisting those who wish to quit either by referring them to statewide tobacco quitlines or to other tobacco cessation programs including those provided directly in the dental operatory. Numerous studies show that individuals, even those who plan to continue using tobacco, prefer that health professionals advise them to quit.15 Most tobacco users want to quit and desire support and encouragement to do so, especially from those they highly respect and trust. When clinicians intervene in smoking cessation, the number of people who quit smoking doubles.16
The 5 A’s Approach
Clinical Practice Guidelines for Treating Tobacco Use and Dependence are provided by the Public Health Service. They outline the following 5 A’s Approach that dental hygienists can use to help their clients conquer their tobacco use:16
- Ask all clients if they use tobacco.
- Advise those who do to quit.
- Assess the client’s readiness to quit in the next month.
- Assist clients with quitting.
- Arrange follow-up to check on their progress.
If you do not have the resources to provide in-office, intensive cessation assistance or if you want to augment assistance already provided, a new cessation tool is available—tobacco use quitlines. These are telephone-based cessation counseling programs that provide tobacco product users with support in quitting.17 The Office on Smoking and Health, Centers for Disease Control and Prevention (CDC), and the American Legacy Foundations describe tobacco use quitlines as an “integral part of tobacco use cessation services,”18 and they are effective in helping individuals quit.19-21 Quitline services are usually offered toll-free to the general public and are available in two-thirds of the states in the United States.18 You do not have to live in a particular state to access the toll-free quitline. Thus, for those clients who are ready to quit their tobacco use, dental hygienists can feel confident advising them that additional help is a phone call away and providing them with a tobacco quitline number.
Quitline Growth
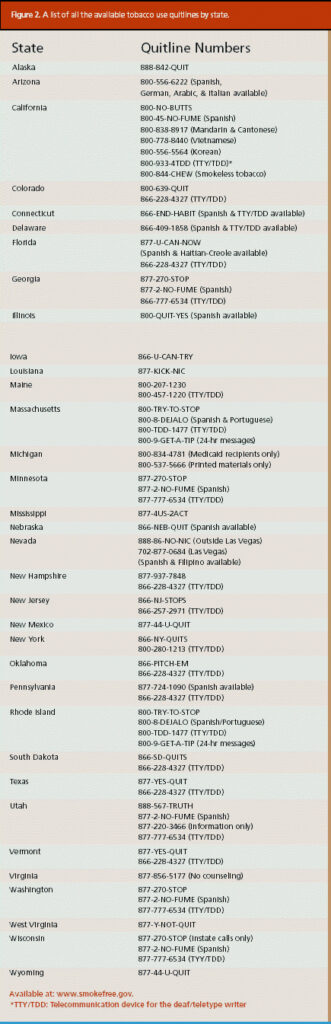
Quitlines are available to most Americans with access to telephones. Figure 1 shows the 34 states that currently offer statewide tobacco use quitlines. In 1992, only the state of California offered a quitline. Figure 2 provides a list of all the available quitlines by state.
Quitlines are becoming more widespread because they offer easy access at no cost to the client, they address ethnic and geographic disparities, and, most importantly, they work. Randomized trials of the California quitline showed that telephone counseling doubled quit rates compared with the use of self-help materials alone.19-21
In addition, one study found that many tobacco users prefer quitlines over face-to-face programs because telephone counseling is more convenient.23 Quitlines also provide anonymity since the counselor and client never meet in person.
Key factors that increase quitline effectiveness include: the use of trained counselors,24 proactive quitlines where staff initiate contact and follow-up,16,17 and the use in combination with client self-help materials and/or Food and Drug Administration (FDA) approved pharmaceuticals.16,17 Effective tobacco cessation treatment includes counseling plus nicotine replacement therapy and/or Bupropion Sustained Release (Zyban), which is the first non-nicotine medication effective for smoking cessation and approved by the FDA for that use.25 Its mechanism of action is presumed to be mediated by its capacity to block neural re-uptake of dopamine and/or norepinephrine. Available by prescription only, it is contraindicated in clients with a seizure disorder, a current or prior diagnosis of bulimia or anorexia nervosa, use of a monoamine oxidase inhibitor within the previous 14 days, or in clients on another medication that contains Bupropion. The quitline staff are trained counselors and provide tobacco users with all the necessary information.
To date among statewide quitlines, 100% offer mailed materials; 90% provide reactive counseling (ie, they respond to callers); 87% provide additional proactive counseling (ie, they call on quit dates and at other times to check how the client is progressing with the quitting process); 43% help obtain nicotine replacement or Zyban to assist with quitting; 42% provide web-based chat rooms; 32% provide taped messages; and 25% dispense nicotine replacement or Zyban.22
Some quitlines offer guidance for particular populations. For example, 90% of quitlines provide special services for pregnant smokers and 63% do for spit tobacco users (ie, those who use oral snuff, chewing tobacco, or some other form of nonsmoked tobacco). In addition to English, most quitlines offer services in Spanish, and some offer them in Korean, Vietnamese, Mandarin, and Cantonese.22
The US Department of Health and Human Services’ Healthy People 2010 states that by the year 2010 “at least 75% of the population of primary care and oral health care providers will routinely advise cessation and provide assistance and follow-up to all of their tobacco using patients.”26 Tobacco use quitlines are valuable resources available to dental hygienists and other health care professionals to augment cessation assistance provided in the health care setting. By referring clients to tobacco use quitlines, the dental hygienist can help improve oral health and save a life in less than 3 minutes.
References
- Smoking-attributable mortality and years of potential life lost—United States, 1984. MMWR Morb Mortal Wkly Rep. 1997;46:444-451.
- Schroeder SA. Conflicting dispatches from the tobacco wars. N Engl J Med. 2002;347:1106-1109.
- Reducing the Health Consequences of Smoking: 25 Years of Progress—a Report of the Surgeon General. Rockville, Md: US Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health;1989. DHHS publication 89-8411.
- Tomar SL, Asma S. Smoking-attributable periodontitis in theUnited States: findings from NHANES III—National Health and Nutrition Examination Survey. J Periodontol. 2000;71:743-751.
- Gelsky SC. Cigarette smoking and periodontitis: methodology to assess the strength of evidence in support of a causal association. Community Dental Oral Epidemiology. 1999;27(1):16-24.
- Robertson PB, Walsh M, Greene J, et al. Periodontal effects associated with the use of smokeless tobacco. J Periodontol. 1990;61:438-443.
- Research, Science and Therapy Committee of theAmericanAcademyof Periodontology. Position paper: tobacco use and the periodontal patient. J Periodontol.1999;70:1419-1427.
- Tomar SL. Dentistry’s role in tobacco control. J Am Dent Assoc. 2001;132(Suppl):30S-35S.
- Ernster VL, Grady DG, Greene JC, et al. Smokeless tobacco use and health effects among baseball players. JAMA. 1990;264:218-224.
- Tomar SL, Winn DM, Swango PA,GiovinoGA, Kleinman DV. Oral mucosal smokeless tobacco lesions among adolescents in theUnited States. J Dent Res.1997;76(6):1277-1286.
- Little SJ, Stevens VJ, LaChance PA, et al. Smokeless tobacco habits and oral mucosal lesions in dental patients. J Public Health Dent. 1992;52(5):269-276.
- Mecklenburg RE, Greenspan D, Kleinman DV, et al. Tobacco effects in the mouth.Washington,DC: US Department of Health and Human Services, Public Health Service; 1992. DHHS publication 92-3330.
- Jones JK, Triplett RG. The relationship of cigarette smoking to impaired intraoral wound healing: a review of evidence and implications for patient care. J Oral Maxiollofac Surg. 1992;50:237-239.
- Preber H, Bergstrom J. Effect of smoking on periodontal healing following surgical therapy. J Clin Periodontol. 1990;17:324-328.
- Campbell HS, Sletten M, Petty T. Patient perceptions of tobacco cessation services in dental offices. J Am Dent Assoc. 1999;130:219-226.
- Fiore MC, Bailey WC, Cohen SJ, et al. Treating Tobacco Use and Dependence: Clinical Practical Guideline.Rockville,Md:USDepartment of Health and Human Services, Public Health Service; June 2000.
- Hopkins DP, Briss PA, Ricard CJ, et al. Reviews of evidence regarding interventions to reduce tobacco use and exposure to environmental tobacco smoke. Am J Prev Med. 2001;20(Suppl):16-66.
- Zhu SH, Stretch V, Balabanis M, Rosbrook B, Sadler G, Pierce JP. Telephone counseling for smoking cessation: effects of single-session and multiple-session interventions. J Consult Clin Psychol. 1996;64(1):202-211.
- Zhu SH,AndersonCM, Johnson CE, Tedeschi G, Roeseler A. A centralized telephone service for tobacco cessation: the California experience. Tob Control.2000;9(Suppl 2):ii48-ii55.
- Zhu S-H, Anderson CM, Tedeschi GJ, et al. Evidence of real-world effectiveness of a telephone quitline for smokers. N Engl J Med. 2002;347:1087-1093.
- Anderson CM. Making a difference: tobacco quitlines. Paper presented at: Dental Hygienists’ Tobacco Cessation Leadership Meeting;September 4-5, 2003;San Francisco.
- McAfee T, Sofian N, Wilson J, Hindmarsh M. The role of tobacco intervention in population-based health care: a case study. Am J Prev Med. 1998;14(Suppl):46-52.
- Best practices for a comprehensive tobacco control program. Presented at: Annual Meeting of the Centers for Disease Control and Prevention;Atlanta: 1999.
- Gansky SA, Ellison JA, Kavanagh C, Hilton JF, Walsh MM. Oral screening and brief spit tobacco cessation counseling: a review and findings. J Dent Education. 2002;66(9):1088-1098.
- Healthy People 2010 Information Access Project. Office of Disease Prevention and Health Promotion, US Department of Health and Human Services. Available at: www.healthypeople.gov. AccessedMarch 20, 2003.
From Dimensions of Dental Hygiene. November / December 2003;1(7):20-22, 24.

