The presence of furcation involvement or furcation invasion has long been recognized as a risk factor for tooth loss. As a general rule, the presence of furcation involvement lowers the long-term prognosis of a tooth by one category, eg, from good to fair. The periodontal literature also shows that patients who comply with periodontal maintenance treatment recommendations lose fewer teeth than patients who do not receive regular periodontal maintenance therapy.1,2 During periodontal maintenance treatment, dental hygienists must debride the furcation as completely as possible.
Despite having a compromised prognosis, molars with furcation involvement can be successfully maintained with fairly conservative treatment and regular maintenance. This is demonstrated by a long-term study of maxillary molars with furcation involvement in 100 periodontal patients who were followed for 24 years. Of the involved teeth, 88% were still functioning at the end of the study.3
WHAT IS FURCATION INVOLVEMENT?
A furcation involvement exists when bone loss has extended into the bifurcation or tri-furcation of a multi-rooted tooth. The presence of furcation involvement in a molar poses multiple treatment challenges for the clinician and also for the patient who is trying to attain good plaque control. The first step to successful treatment of a furcation is to identify its presence and the extent and specific anatomy of the furca.

Mandibular molars are two rooted (bifurcated) with furcations on the buccal and lingual surfaces. Maxillary molars are typically three rooted (trifurcated) with furcations on the buccal, mesial, and distal surfaces. The article “Furcation Anatomy” by Constance R. Sharuga, RDH, PhD, that appeared in the March 2010 issue of Dimensions pro vided an excellent review of furcation anatomy and the importance of thinking about tooth anatomy in three-dimensions. Even teeth with normal root trunks can have furcations starting at 3 mm to 4 mm below the cementoenamel junction. A clinician holding a probe parallel to the long axis of a tooth and focused on accurately probing only for pocket depth will often fail to identify the presence of a furcation involvement. Knowing where to look and using multiple tools are important for furcation detection and grading, especially for the proximal furcations.
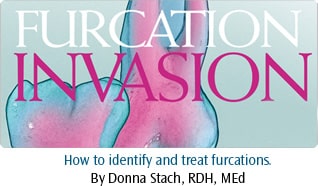
Furcation involvement is more common and severe in first molars than in second molars.5 The general trend is to move from normal and mild involvement in the third decade of life to moderate and severe furcation involvement in the fifth, sixth, and sev enth decades.5 These findings are based on tooth/root anatomy and progression of bone loss. A classic study by Ross and Thompson that looked at patients in a periodontal practice provides more insight into the prevalence of furcation invasions and also into the methods most likely to identify their presence.6 Clinical examination showed furcation involvement in 90% of the maxillary molars and in 35% of the mandibular molars. Clearly, there are more furcation involvements in maxillary teeth, which means there are many proximal furcations. These furcations are more difficult to find and treat. Both clinical and radiographic exams should be used to identify the presence of furcation invasions. In this study, when only a clinical examination was used, 22% of maxillary furcations were missed, most likely those on the proximal surfaces. As seen in radiographs, proximal furcations appear as small triangular shadows pointing to the furcation on either the mesial or distal surfaces. These are called “furcation arrows” (Figure 1). The presence of the furcation arrow indicates the presence of a Class II or Class III proximal furcation involvement but this should be confirmed clinically. However, the absence of a furcation arrow does not necessarily mean the absence of a furcation.7

Maxillary molar mesial furcations are typically located one-third of the distance from the lingual surface and two-thirds of the distance from the buccal surface. This location, combined with the larger lingual embrasure space, makes mesial furcations both easier to locate and treat. Distal molar furcations are located halfway across the distal surface and can be accessed from either the buccal or lingual aspect. Knowing the most likely location of a furcation allows a clinician to tilt the periodontal probe inward along a molar surface to find the furcation opening or, in the case of fused roots, the groove of the furcation. This technique is especially useful in identifying furcations on the distal surface of the last maxillary molar. On a second or third molar, the roots are often fused so that the furcation is a long vertical groove in the root surface rather than a frank opening between the roots (Figure 2A). With the probe adapted to the distal of the tooth, a gentle sliding motion from buccal to lingual and back will identify a dip in the surface that is the furcation (Figure 2B). A similar technique can be used for other proximal furcations but may be more difficult if they are close to the adjacent tooth.
A furcation is a difficult treatment chal lenge and successful treatment is possible only by fully understanding the furcation’s contours. The Nabers 1N and 2N probes are traditional instruments for measuring the horizontal depth of a furcation and can also be used to explore the shape of the space (Figure 3). For a groove created by fused roots, a curved explorer or a straight periodontal probe may be used. These will often be the best choice for a furcation in a deep pocket where the large curve of a Nabers probe can be difficult to manipulate. Often the treatment instrument (either a curved curet or ultrasonic tip) used with a light exploratory horizontal or vertical stroke instead of a treatment stroke works well. A slim style ultrasonic tip used with the power off can be used like an explorer (Figure 2C) and should be used often dur ing pauses in treatment to feel the way along the tooth contours. More acute tactile sensitivity to assess the inner surfaces of the roots and the floor or ceiling of the furcation can be achieved with an explorer. Direct the toe of the explorer apically, precisely adapt the terminal por tion of a long, slightly curved explorer like the 3A or an extended shank ODU 11/12 and activate overlapping vertical, oblique, and horizontal strokes with light to mod erate pressure.
INSTRUMENTATION TECHNIQUE
A 1987 study by Leon and Vogel8 showed that in a Class I furcation treatment with either a curet or an ultrasonic scaler was equally successful. But in Class II or Class III furcations treatment with an ultrasonic tip was more successful. In 1997, Otero-Cagide and Long published two articles that showed mini-bladed curets were more effective for scaling furcations than a thin ultrasonic tip.9,10
Many furcations have tight openings with little room for adapting a curet with a standard, larger cutting edge and making a working stroke, so a mini-bladed or micro mini-bladed curet or a thin ultrasonic tip that works by vibrating in place would be the instruments of choice.
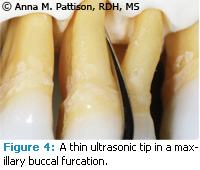
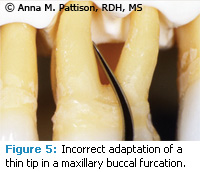
The turbulence and acoustic micro streaming created by the ultrasonic vibration in a small space results in a flushing of debris and biofilm that also plays a critical role in treatment. An ultrasonic tip is not an irrigator to be used for a quick rinse before moving on to the next surface. Contact of the ultrasonic tip to the tooth surface is important for best treatment. Ideally, the terminal few millimeters of the tip and not the point should make contact (Figure 4). Since the point is the most powerful part of the ultrasonic tip, contacting the inner surfaces of the furcation with the point can result in etch ing, root damage, or even pulpal expo sure with repeated grooving over time (Figure 5). While it is important to keep the point from contacting the inner aspects of the roots, it is not always possible to achieve this in a tight or complex furcation. In a large furcation where the insides of the roots are accessible, there are numerous concavities in the inner surfaces of the roots, and clinicians need to feel their way along the surface. The goal of instrumentation is always to have over lapping strokes and to contact all areas of the tooth. Nowhere is this more difficult than in furcations and complete success is not achievable in many cases. However, striving for this goal of complete instrumentation and carefully visualizing the shape of the furcation will give the best possible result and these teeth can be suc cessfully maintained over many years.
Vertical strokes with a standard curet blade or an ultrasonic tip with the working end adapted perpendicular to the long axis of the tooth will pass over the furcation area without any contact in the problematic groove or concavity formed on the distal of a maxillary second molar (Figure 2). Essentially, the furcation is not being accessed or treated. This is one reason it is important to know that a furcation is present on the tooth. Because the shape of an ultrasonic tip is more likely to adapt to the furcation groove, it is a good instrument choice. On the distal of the last maxillary molar, the straight tip may be the instrument of choice in a groove. Adaptation is only possible if the terminal portion of the ultrasonic insert is held parallel to the long axis of the tooth and then carefully adapted to follow the usual inward tapering surface of the root (Figure 2C).
The best ultrasonic tip to use in treating a furcation is usually a curved or contra angled slim style insert. The rule of thumb in treating a furcation is to first understand the extent and features of the furcation and then to instrument it with careful overlap ping strokes. The root flutings of an early stage furcation are often a broad, accessible surface, and the back or convex side of the contra-angled ultrasonic insert adapts well to the concave surface (Figure 6). It is relatively easy to adapt, but keep the point off of the root and use methodical overlapping strokes.
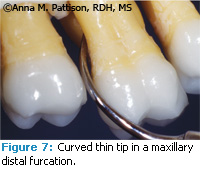
In a Class II furcation where there is access between the roots but not much bone loss, there is often a tight space ending in a cul-de-sac. An ultrasonic insert will fit into the space but it may not be possible to have much or any up-and down movement. In this case, move the tip in and out of the furcation. The inside of the curve or the concave surface of the ultrasonic insert will be the one that seems to adapt best but this will likely put the terminal point of the insert on the root surface and frequent or repetitive working strokes on the same path can result in damage by creating a groove in the root surface (Figure 7). Root damage is less likely if the outer curve or convex surface of the insert is adapted to the root (Figure 8). The inner root surfaces should be assessed frequently with an awareness of the potential for gouging or creating grooves over time.
DON’T FORGET THE FLUORIDE.
Furcations are often plaque retentive root surfaces seen in older patients. When a furcation is found, evaluate the need for in-office fluoride varnish and/or prescription at-home fluoride gel applied with an interdental brush. It would be unfortunate to stop the progression of periodontitis in a furcation only to lose the tooth to root caries.

Special furcation inserts with ball tips are designed to be more protective of the inner root surfaces and should be used on low power. They are beneficial for biofilm removal but there is limited research about their efficacy in calculus removal. Tunneling is an intentional procedure that opens or reshapes the entrance to the furcation to improve access for treatment and long-term maintenance of the tooth. It can be done with a bur by a dentist or periodontist or over a longer period of time with a curet or ultrasonic tip during repeated debridements. Instrumentation in this situation will also be influenced by the position of The soft tissue over the furcation opening. If the gingiva cover ing the furcation open ing is very tight and is forcing the ultrasonic point into the tooth or always in the same path of insertion, then the tip should not be active during the insertion and should only be reactivated after the tip is in place to begin treatment.
Molars with more furcation involve ment, more working room, and more root surface needing treatment pose additional additional challenges. The internal anatomy of the roots can be complex with a number of concave surfaces. Access to these areas may be com promised, especially in the maxillary molars, by adjacent teeth or by pocketing and soft tissue covering the entrance. The use of carefully overlapping strokes may not be possible (Figure 7). Instrument thoughtfully, interrupt the power frequently so the tip can be used to evaluate treatment, try approaching from multiple directions, and notice if the shape of the tooth and the access or path of insertion is always guiding the instrument into the same spots. Keep in mind that treatment of a furcation is challenging and that good treatment is imperfect. The long-term prognosis of the tooth is improved by careful treatment and frequent maintenance.
CONCLUSION
Furcation involvement in both maxillary and mandibular molars presents a significant technical challenge for successful treatment. Much of the research about the location, frequency, and characteristics of furcations was conducted in the 1980s. However, the information is just as pertinent today as it was then. It is only by anticipating and looking for furcations, determining their shapes and contours, and treating them as meticulously as possible—usually with an ultrasonic scaler—that the many patients with furcation-involved teeth will receive the best quality treatment.
REFERENCES
- Pihlstrom BL, Oliphant TH, McHugh RB. Molar and nonmolar teeth compacted over 6 ½ years following two methods of periodontal therapy. J Periodontol. 1984;55:499.
- McFall WT. Tooth loss in 100 treated patients with periodontal disease. A long-term study. J Periodontol. 1982;53:539.
- Ross IF, Thompson RH Jr. A long term study of root retention in the treatment of maxillary molars with furcation involvement. J Periodontol. 1978;49:238.
- Sharuga CR. Furcation anatomy. Dimensions of Dental Hygiene. 2010;9(3):36-38.
- Tal H, Lemmer J. Furcal defects in dry mandibles. Part II: Severity of furcal defects. J Periodontol. 1982;53:364-367.
- Ross IF, Thompson RH Jr. Furcation Involvement in maxillary and mandibular molars. J Periodontol. 1980;51:450.
- Hardekopf JD, Dunlap RM, Ahl DR, Pelleu GE Jr. The “furcation arrow,” a reliable radiographic image? J Periodontol. 1987;58:258.
- Leon LE, Vogel RI. A comparison of the effectiveness of hand scaling and ultrasonic debridement in furcations as evaluated by differential dark-field microscopy. J Periodontol. 1987;58:86-94.
- Otero-Cagide FJ, Long BA. Comparative in vitro effectiveness of closed root debridement with fine instruments on specific areas of mandibular first molar furcations. I. Root trunk and furcation entrance. J Periodontol. 1997;68:1093.
- Otero-Cagide FJ, Long BA. Comparative in vitro effectiveness of closed root debridement with fine instruments on specific areas of mandibular first molar furcations. II. Furcation area. J Periodontol. 1997;68:1098-1101.
From Dimensions of Dental Hygiene. January 2011; 9(1): 42, 44, 46-48.

