BECON/ISTOCK/GETTY IMAGES PLUS
BECON/ISTOCK/GETTY IMAGES PLUS
Esthetic Options for Tooth Movement
Clear aligners and lingually positioned appliances present esthetic alternatives to orthodontic treatment with traditional braces.
This course was published in the February 2019 issue and expires February 2022. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- List various approaches to orthodontic therapy, reasons why patients may prefer one modality to another, and how gender and age may influence preference.
- Identify the pros and cons of clear aligner and lingual appliance therapies.
- Discuss theories for tooth movement and forces that affect outcomes during orthodontic treatment.
Compared with traditional braces, clear aligners are perceived as more attractive.2 Most women age 40 and younger prefer lingual vs buccal appliances, and women ages 20 to 30 prefer aligner therapy.3,4 Children and teens also rate the acceptability of clear aligners higher than conventional appliances.5 Adults may favor aligners due to ease of adaptation, greater comfort, and less analgesic consumption.4,6 Alternatives to metal braces are usually more expensive, yet adults desiring esthetic options are often willing to assume these costs.7 As with traditional buccally positioned systems, lingual appliances have brackets with a slot for a wire that is ligated into the bracket (Figure 2).
ALIGNER THERAPY
Today, ongoing advances allow more complex malocclusions to be treated with aligners than was previously possible. Aligner therapy consists of a series of removable, clear polyurethane trays. Each aligner in the sequence moves the teeth in small increments until the predetermined setup is achieved.8 Because the aligners are removable, the forces are interrupted; therefore, the prescription is typically to wear each set for 20 hours to 22 hours per day for 1 week to 2 weeks. They are only removed while eating or for oral hygiene procedures.9 Although research has not established the ideal wear time, a study comparing 1-week and 2-week-activations found that 2-week wearers were more likely to complete treatment with the desired result.10 Weekly changes have recently been advocated; this stems from improved aligner materials and refined treatment mechanics that purportedly allow more efficient tooth movement. At present, evidence supporting weekly aligner change is lacking.
There are also many aligner “do it yourself” approaches, where the patient submits “selfie” impressions. No studies document the effectiveness of these approaches, which omit an orthodontic expert who can refine and redirect treatment for optimal outcomes and diagnostic radiographs. They are not endorsed by the American Association of Orthodontists.

TOOTH MOVEMENT
Whether using traditional, lingual, or clear aligner systems, the major player in tooth movement is the periodontal ligament (PDL) that surrounds and attaches each tooth root to the alveolar bone.11 Approximately 0.5 mm in width, the PDL contains collagenous fibers, fibroblasts, osteoblasts, osteoclasts and tissue fluids. The collagen acts as the tooth’s support system during function and is continually remodeled by fibroblasts. The osteoclasts are responsible for carving away bone to create space into which the tooth moves, while osteoblasts build new bone in the space vacated by the tooth.11

Two theories for the initiation of tooth movement are piezoelectricity (biological electricity generated by bending crystals within the bone) and pressure-tension within the PDL.12 Biological electricity is produced as membrane potentials in the alveolar bone are disrupted. This change alters the bone metabolism which, in turn, impacts tooth movement. The focus of the pressure-tension theory is chemical mediators rather than electrical signals.13 As force is applied to a tooth, the PDL is compressed on the side where the tooth is pushed. This alters blood flow, which signals the formation of chemical messengers to recruit osteoclasts and osteoblasts for bone remodeling.11 In both theories, the bone adjacent to the PDL is remodeled in a subtractive or additive way, depending on the direction of applied force.
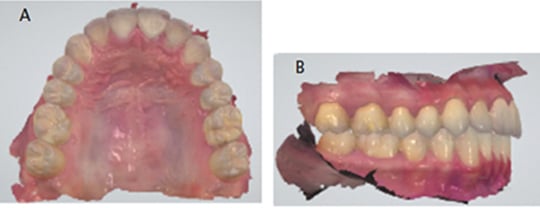
Aligner therapy utilizes computer aided design/computer aided manufacturing (CAD/CAM) technology for the digital setup and manipulation of malocclusions. Teeth are digitally scanned and a three-dimensional digital file is submitted (Figure 3). Alternately, vinyl polysiloxane impressions can be submitted for digitizing by the aligner company. A technician digitally aligns the teeth and sets up the occlusion. The treating dentist views the proposed setup and supplies changes as needed to create a final setup. Once approved, physical models of each treatment stage are created, upon which the aligners are fabricated (Figure 4). Tooth movement proceeds by up to 0.25 mm per aligner/stage, although this may vary by manufacturer. The number of aligners is based on the severity of the individual malocclusion.9
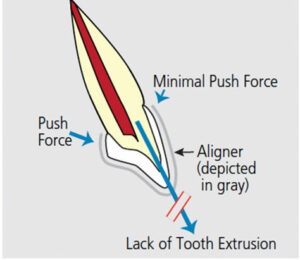
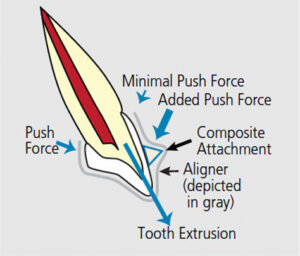
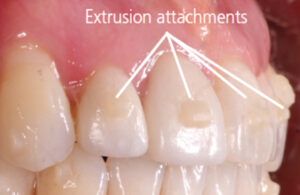
Aligners produce tooth movement by pushing, rather than pulling, on teeth. Compared with lingual or buccal braces that produce push-and-pull forces, this places aligners at a distinct disadvantage. The natural anatomy of teeth can make certain types of orthodontic movement with aligners difficult. Tooth extrusion is one example. The lack of sufficient undercuts at the gingival margins of a tooth makes pushing it into a more extruded position nearly impossible. To address this, an undercut can be created by bonding composite to the tooth. Using the created undercut, a tooth can be pressed or squeezed into the aligner in an extrusive direction (Figure 5 to Figure 7).
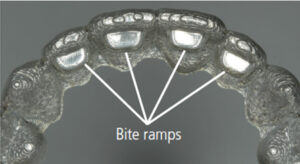
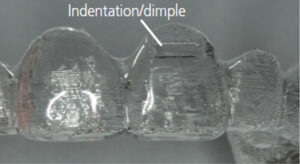
Modern aligners include a host of optional features that may improve efficacy. Built-in bite ramps can be placed on the outside surface of the aligner to create an anterior vertical stop to prevent excessive bite force on molars (Figure 8). Aligner indentations/dimples help with root position (Figure 9, page 35), and cutouts for interarch elastics can also aid treatment. Auxiliary appliances, such as elastics or Class II or III bite correctors, as used with traditional braces, may be combined with aligner therapy. Prior to commencing treatment, clinicians should have a full understanding of the application of each system. It is imperative that treatment is monitored regularly by a dentist or specialist to make adjustments and avoid adverse outcomes.
Interproximal reduction (ie, reducing tooth width with finishing strips) is frequently used with aligner therapy to reduce crowding. If necessary, this step should be outlined in the treatment plan.
ADVANTAGES OF ALIGNER THERAPY
Periodontal health. Studies have found that compared to fixed appliances, removable appliances are associated with less biofilm accumulation and significantly improved overall periodontal health in terms of probing depth, bleeding on probing, and plaque index, both in the short term (3 months) and long term (12 months).14,15 Patients wearing clear aligners also exhibit better oral hygiene compliance than individuals treated with traditional fixed brackets.15
Increased comfort. Although clear aligner therapy is not pain free, there is generally less discomfort than with fixed appliances, especially in the initial stages of treatment.16 Additionally, this approach reportedly minimizes negative impacts on quality of life.6
Shorter and fewer appointments. A study comparing similar malocclusions treated with traditional braces or clear aligners found that braces required a median of 13.6 minutes for routine appointments, compared with 9.9 minutes for aligners. On average, braces required an additional 2.6 appointments (requiring 86.2 more minutes of chairtime), and overall treatment took 2.4 months longer.17

DISADVANTAGES
Compared with traditional orthodontic treatment, the lab costs associated with aligners are typically higher. Compliance can be an issue with some patients. Beyond this, a common occurrence with aligners is the development of a posterior open bite.9 With 0.75 mm of plastic per arch between the teeth, occlusion has an intrusive effect on the posterior teeth. Subsequently, the clinician must rely on the teeth to settle on their own, or use interarch elastics to close the open bite. Reportedly, placing anterior bite ramps on the maxillary aligners can lessen the intrusive force, resulting in even occlusion with the anterior teeth—yet there is no literature evidence to support this claim. Despite improvements, aligners are not yet indicated for all types of tooth movement and malocclusions.
ALIGNER-APPROPRIATE CASES
Whether clear aligners and conventional braces produce equally effective outcomes is unclear. Extraction treatment is not often indicated with aligner therapy, and this also applies to correction of Class II and III malocclusions. As technology advances, however, more types of malocclusions may be treated with aligners.
A systematic review found that aligning teeth works well in cases of mild to moderate crowding.18 Intrusion is equivalent with aligners and traditional braces,19 but extrusion is the most difficult movement to produce using aligners.18 With proper staging of tooth movement and appropriately designed attachments, both rotations and bodily movements can be accomplished,18,20 but there is debate regarding these types of movement. Controlled and uncontrolled tipping have been found to be fairly successful.19,21 Furthermore, aligners can be effective for Class I extraction cases;22 in more complex situations, however, treatment time may be longer compared to fixed appliance therapy.22 Aligners do not procline lower incisors (normally an unwanted outcome) more than fixed appliances, as was once thought.23 Regarding Class II and III malocclusion corrections, early studies indicated poor outcomes with aligners;21 however, strong evidence is lacking. Case considerations and knowledge of comparative research findings are key when selecting the appropriate treatment approach.
LINGUAL APPLIANCE PROS AND CONS
In the United States, Kurz introduced a lingual appliance with the objective of esthetics.24 At that time, clinical protocols for lingual braces were not fully developed, and the complexity of bonding and inaccuracy in finishing discouraged their use. Lingual orthodontic treatment soon fell out of favor due to the introduction of ceramic brackets, which were more esthetic than metal and easier to use than lingual appliances. Current technology offered in several new systems, however, addresses many of the clinical difficulties of lingual appliances.
This treatment modality is available in customized and noncustomized formats. The fully customized system uses CAD/CAM technology to manufacture lingual brackets formatted to the anatomy of each tooth, along with robotically bent archwires programmed to align the teeth precisely. For noncustomized appliances, prefabricated brackets with adjustable composite bracket pads are used. Typically, use of an indirect bonding technique improves accuracy of bracket placement.
The major advantage of lingual braces is esthetics, as they are largely undetectable during social interaction. Another advantage is a reduction in visible surface damage resulting from bonding, debonding, decalcification, and adhesive removal. Compared with lingual appliances, white spot lesions occur or progress 4.8 times faster with traditional braces.25 In addition, unsightly hypertrophic facial gingival tissue is minimal, and any tissue edema that develops on the lingual would not be visible.
Another benefit of lingual appliances is an improved view of the patient’s teeth and soft tissues during therapy. Practitioners can make slight corrections as treatment progresses, and avoid surprises that sometimes occur after the removal of labial braces. Both clinicians and patients can view facial contours and lip position during treatment to adjust outcomes before debonding.
Lingual braces are more difficult for practitioners to position and adjust than labial appliances. The environment is more constricted, and both tongue and saliva present challenges. Additionally, there are biomechanical differences because the reduction in interbracket distance between lingual brackets increases the stiffness of the wire. This results in lingual braces exerting higher forces than traditional braces.26 Patients also experience a significant adaptation phase with lingual appliances that may include masticatory difficulties, tongue irritation, and speech disturbances during the first 2 weeks to 4 weeks. Compared with noncustomized systems, customized brackets present significantly fewer tongue space restrictions, changes in articulation, and difficulties in mastication due to their lower profile.27
A further consideration is that lingual appliances place 15% more stress on teeth and strain on the PDL than labial braces.28 Consequently, the labial approach may be preferable for a periodontally compromised patient. A recent systematic review and meta-analysis comparing lingual and labial appliances included 11 clinical trials involving 407 patients. Lingual appliances were associated with increased oral discomfort, speech impediment, and eating difficulty. However, the authors concluded there is insufficient evidence to declare either system superior regarding treatment outcomes.29
CONCLUSION
In conclusion, there are multiple considerations when determining the optimal therapeutic approach to moving teeth and correcting malocclusion. In some cases, esthetic options—although more costly—can produce desired outcomes. For other patients, more traditional approaches are indicated. Ultimately, the value of the oral health professional’s knowledge and clinical expertise cannot be overemphasized in this advancing era of technology-based orthodontic treatment.
REFERENCES
- Shalish M, Cooper-Kazaz R, Ivgi I, et al. Adult patients’ adjustability to orthodontic appliances. Part I: a comparison between labial, lingual, and Invisalign. Eur J Orthod. 2012;34:724–730.
- Ziuchkovski JP, Fields HW, Johnston WM, Lindsey DT. Assessment of perceived orthodontic appliance attractiveness. Am J Orthod Dentofacial Orthop. 2008;133:S68—S78.
- Hohoff A, Fillion D, Stamm T, Goder G, Sauerland C, Ehmer U. Oral comfort, function and hygiene in patients with lingual brackets: a prospective longitudinal study. J Orofac Orthop. 2003;64:359–371.
- Nedwed V, Miethke RR. Motivation, acceptance and problems of Invisalign patients. J Orofac Orthop. 2005;66:162–173.
- Walton DK, Fields HW, Johnston WM, Rosenstiel SF, Firestone AR, Christensen JC. Orthodontic appliance preferences of children and adolescents. Am J Orthod Dentofacial Orthop. 2010;138:698.e1–e12.
- Miller KB, McGorray SP, Womack R, et al. A comparison of treatment impacts between Invisal=lign aligner and fixed appliance therapy during the first week of treatment. Am J Orthod Dentofacial Orthop. 2007;131:302.e1–e9.
- Rosvall MD, Fields HW, Ziuchkovski J, Rosential SF, Johnston WM. Attractiveness, acceptability, and value of orthodontic appliances. Am J Orthod Dentofacial Orthop. 2009;135:276.e1–e12.
- Boyd R, Vlaskalic V. Three-dimensional diagnosis and orthodontic treatment of complex malocclusions with the Invisalign appliance. Sem in Orthod. 2001;7:274–293.
- Boyd R, Miller R, Vlaskalic V. The Invisalign system in adult orthodontics: mild crowding and space closure cases. J Clin Orthod. 2000;34:203–212.
- Bollen AM, Huang G, King G, Hujoel P, Ma T. Activation time and material stiffness of sequential removable orthodontic appliances. Part 1: ability to complete treatment. Am J Orthod Dentofacial Orthop. 2003;124:496–501.
- Proffit WR. The biological basis of orthodontic. In: Proffit WR, Fields HW, eds. Contemporary Orthodontics. 5th ed. St Louis: Mosby; 2012:278–311.
- Thilander B. Tissue reactions in orthodontics. In: Graber LW, Vanarsdall R, Vig KWL, eds. Orthodontics: Current Principles and Techniques. 5th ed. St. Louis, Elsevier, 2011:247–286.
- Krishnan V, Davidovitch Z. On a path to unfolding the biologic mechanisms of orthodontic tooth movement. J Dent Res. 2009; 88:587–608.
- Levrini L, Mangano A, Montanari P, Margherini S, Caprioglio A, Abbate GM. Periodontal health status in patients treated with the Invisalign system and fixed orthodontic appliances: A 3 months clinical and microbiological evaluation. Eur J Dent. 2015;9:404–410.
- Abbate GM, Caria MP, Montanari P, et al. Periodontal health in teenagers treated with removable aligners and fixed orthodontic appliances. J Orofac Orthop. 2015;76:240–250.
- Fujiyama K, Honjo T, Suzuki M, Matsuoka S, Deguchi T. Analysis of pain level in cases treated with Invisalign aligner: comparison with fixed edgewise appliance therapy. Prog Orthod. 2014;15:64.e1—e7.
- Harrison L. Study Shows Invisalign More Profitable Than Braces. Available at https:/ / www.medscape.com/ viewarticle/ 761051. Accessed November 30, 2018.
- Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Efficacy of clear aligners in controlling orthodontic tooth movement: a systematic review. Angle Orthod. 2015;85:881–889.
- Kravitz ND, Kusnoto B, BeGole E, Obrez A, Agran B. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am J Orthod Dentofacial Orthop. 2009;35:27–35.
- Simon M, Keilig L, Schwarze J, Jung BA, Bourauel C. Treatment outcome and efficacy of an aligner technique — regarding incisor torque, premolar derotation and molar distalization. BMC Oral Health. 2014;14:68.e1–e7.
- Djeu G, Shelton C, Maganzini A. Outcome assessment of Invisalign and traditional orthodontic treatment compared with the American Board of Orthodontics objective grading system. Am J Orthod Dentofacial Orthop. 2005;128:292–298.
- Li W, Wang S, Zhang Y. The effectiveness of the Invisalign appliance in extraction cases using the ABO model grading system: a multicenter randomized controlled trial. Int J Clin Exp Med. 2015;8:8276–82.
- Hennessy J, Garvey T, Al-Awadhi EA. A randomized clinical trial comparing mandibular incisor proclination produced by fixed labial appliances and clear aligners. Angle Orthod. 2016;86:706–712.
- Ling PH. Lingual orthodontics: history, misconceptions, and clarification. J Can Dent Assoc. 2005;71:99–102.
- van der Veen M, Attin R, Schwestka-Polly R, Wiechmann D. Caries outcomes after orthodontic treatment with fixed appliances: do lingual brackets make a difference? Eur J Oral Sci. 2010;118:298–303.
- McMullin A, Waring DT, Malik OH. Invisible orthodontics part 2: lingual appliance treatment. Dent Update. 2013;40:391–394,401–402.
- Hohoff A, Stamm T, Ehmer U. Comparison of the effect on oral discomfort of two positioning techniques with lingual brackets. Angle Orthod. 2004;74:226–233.
- Liang W, Rong Q, Lin J, Xu B. Torque control of the maxillary incisors in lingual and labial orthodontics: a 3-dimensional finite element analysis. Am J Orthod Dentofacial Orthop. 2009;135:316–322.
- Papageorgiou SN, Gölz L, Jäger A, Eliades T, Bourauel C. Lingual vs. labial fixed orthodontic appliances: systematic review and meta‐analysis of treatment effects. Eur J Oral Sci. 2016;124:105–118.
From Dimensions of Dental Hygiene. February 2019;17(2):32–35.