Dental Waterline Safety
Tips to ensure the water quality in your practice.
The quality of dental unit water is critical to effective infection control. Clinicians and patients are exposed to water from these lines, as well as aerosols produced by dental instruments. Microorganisms colonize in biofilms within dental units and contaminate dental treatment waters.1-5 To minimize this potential source of contamination, clinicians must implement appropriate strategies for cleaning and maintenance. Waterlines should be aseptically maintained with the same detail as the other environmental surfaces in the operatory.
Etiology of Biofilm Growth
Biofilms are well-organized aggregates of microorganisms in which cells adhere to each other on a surface. They are composed of bacteria, algae, protozoa, nematodes, and fungi. Biofilms form on most surfaces in contact with water, and they thrive on plastic tubing and dental unit waterlines (DUWLs).6 Frequently embedded within a protective matrix of extracellular polymeric substance called slime, biofilms tightly adhere to the surface in which they are attached, making biofilm infection difficult to destroy.7,8
Water from community systems delivered to the dental unit contains substantially lower numbers of microorganisms than the water that comes out of the dental unit because DUWLs encourage biofilm growth. There are three basic factors involved in this phenomenon: surface area, surface chemistry, and flow rates.10,11 The small plastic tubing used in dental operatories plays a prominent role. Biofilm is tightly bound to the lining of the DUWL tubing and the high surface-area-to-volume ratio increases the area accessible for the development of biofilms.10 Most plastic dental tubing has an inside diameter of 1∕16 inch to 1∕8 inch and is made of polyurethane. This form of plastic provides a hydrophobic, carbon source that promotes and sustains bacterial proliferation.
Another cause of biofilm proliferation is the laminar flow issue, where water moves in parallel layers, with no movement between the layers.12,13 As a result, even when water is flowing, stagnant conditions within the tubing still exist—allowing biofilms to easily form. Intermittent use of water between patients and often no use on weekends and evenings also contribute to stagnant conditions, which favor microbial colonization. The microbial build-up rate is rapid because organisms suspended in the water have a shorter distance to fall before contacting the tubing surface.11 These active biofilms now become the primary reservoir for continued contamination. Pieces of biofilm detach and seed biofilm growth elsewhere in the waterline. As water flows through the piping adjacent to the biofilms, microorganisms spread. This creates the possibility that microorganisms from the biofilm can be flushed into the mouth—putting patients at risk.12 Aerosols and spatter from contaminated waterlines may also contain pieces of biofilm and planktonic microorganisms. Their endotoxins can be inhaled into the lungs of both patients and clinicians.12 The microbes found in DUWLs are usually benign, and people with healthy immune systems are not susceptible to infection from contaminated water.
However, Pseduomonas, Mycobacterium, and Legionella have been isolated in DUWLs, and these respiratory-opportunistic pathogens can cause serious disease in the immunocompromised.7 As dental practices treat more medically complex patients with weakened immune systems, more people will be susceptible to disease through ingesting and inhaling contaminated water. Endotoxins released from Gram-negative water microorganisms can also be found in DUWLs and can cause localized inflammation and fever.15,16 These endotoxins are also associated with a greater incidence of occupational asthma among dental personnel,17 although more research is still needed to validate this link.
Waterline Management
For routine dental treatment, the United States Centers for Disease Control and Prevention (CDC) recommend that DUWLs contain less than 500 colony forming units per milliliter (CFU/mL) of heterotrophic bacteria.18 The manufacturer of the dental unit should be consulted to determine the best approach to DUWL management, which consists of three parts: biofilm eradication, control of free-floating planktonic microorganisms, and periodic water quality monitoring. Flushing of DUWLs was first recommended by the American Dental Association (ADA) in its 1995 “Statement on Dental Unit Waterlines,” and, while still recommended, flushing does not remove biofilm.18 Studies reveal that even after flushing for 4 minutes, the level of CFUs still exceed ADA recommendations for water quality, and biofilms continue to exist.19,20 According to the CDC, DUWLs should be flushed for a minimum of 20 seconds to 30 seconds between patients to discharge oral fluids that may have bypassed antiretraction valves.17 Most contemporary units are equipped with an antiretraction valve designed to reduce suck-back of contaminated oral fluids; however, flushing is still necessary. While flushing can reduce the number of microbes in the water, the effect is temporary. Additionally, all waterlines and handpieces should be flushed for at least 2 minutes at the beginning of the day to reduce the bacterial load from stagnant water conditions that have occurred overnight.13
Treatment Strategies
Several options are available to improve the microbial quality of water used in practice: filters, independent reservoirs, chemical treatments, slow release cartridge devices, sterile water delivery systems, and antimicrobial agents incorporated into tubing.10-14 These options can be divided into two categories: those that treat water entering the dental unit, and independent water systems. There is no universally accepted protocol for DUWL decontamination.
For practices that use community water supplies, the use of microbial filters may be a smart approach. These water treatment devices are placed on each waterline and are designed to remove free-floating microorganisms. The microbial filter is placed in the waterline to trap microorganisms before they can enter a handpiece or air/water syringe, but filters have a limited effect on biofilm and endotoxins.18 Filters also require upkeep, continued expense, and they do not include a container method for sterile water delivery.14
For practices that seek a more centralized approach, water purifiers and centralized systems are available. These are placed at the junction box connected to the municipal water system. Used for decontaminating DUWLs at the point of entry, nanofiltration, deionization, heat, and ultraviolet germicidal irradiation are used to kill and/or remove organisms from the source water.10 These devices may be plumbed directly into the unit or they may use holding tanks placed in a centralized location. This approach improves the source water and can be used in multiple operatories, but it has no residual effect on biofilms within the dental unit. Hence, waterlines must also be treated with a chemical agent to ensure removal of biofilms. Water purifiers, however, may inhibit and delay biofilm formation and increase the effectiveness of other decontamination methods.14 Some systems are designed to also introduce chemicals.
Self-contained water systems used in conjunction with chemicals are effective in improving the quality of DUWL water. Typically available as standard equipment on contemporary dental units, an independent reservoir isolates the dental unit from community water, which allows for chemical treatment of 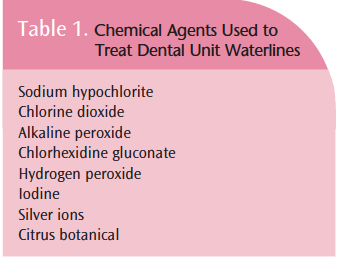 the water. Older units can be easily and inexpensively retrofitted with a bottle system. Unless the biofilm in the lines is controlled and treated, changing the water source from municipal to distilled or sterile in the independent reservoir will not ensure that water standards of less than 500 CFU/mL will be met.
the water. Older units can be easily and inexpensively retrofitted with a bottle system. Unless the biofilm in the lines is controlled and treated, changing the water source from municipal to distilled or sterile in the independent reservoir will not ensure that water standards of less than 500 CFU/mL will be met.
Many agents are available to prevent, inactivate, and remove biofilms, as well as reduce endotoxins. The technique and frequency of adding these products vary depending on manufacturer instructions. Table 1 provides a list of chemicals used for waterline cleaning. Chemical treatments may be periodically added to the waterline or continuously released. The chemicals come in tablets, cartridges, powders, drops, and liquids.19-24 Careful compliance with recommended protocols is critical to prevent harmful effects, as well as to ensure optimal water quality. Because they slowly release antimicrobial agents, automated cartridge systems are less dependent on compliance than other products, but they may require specially conditioned water to achieve the best results. The first step of DUWL treatment is to implement a “shocking” process to eliminate biofilm.
Shocking treatments (intermittent use of high concentration chemicals) are designed to remove the biofilm masses that have built up in the DUWL.9-11 These germicides are typically placed in the water bottle, flushed into the water lines, and held in the line for an extended period before being flushed out.8-11 Shocking treatments should be performed on a weekly or monthly basis. Daily maintenance with low dose chemical treatments is also needed to maintain low levels of microbes in the lines. These agents are added to the water bottle with each filling.
To ensure chemical compatibility, it may be prudent to select the same type of product for both daily use and intermittent shock treatments. Concerns with the use of chemical products include the following: risk of exposure to patients and clinicians; interference between adhesions of resins to enamel and dentin; damage to the dental unit; and microbial resistance to the chemicals over time.23-26
Reservoir bottles are easily contaminated and aseptic techniques must be maintained while filling bottles to minimize contact with skin microorganisms. Reservoir bottles should be cleaned and disinfected according to manufacturer directions. Ensuring that several bottles are available throughout the day is judicious. The incorporation of antimicrobial materials into dental tubing and water bottles is an emerging technology in biofilm control. Some dental unit manufacturers impregnate tubing with silver ions or iodine. Silver ions interfere with the metabolism of microorganisms and, to some extent, may minimize biofilm development.
The periodic addition of an antimicrobial agent, such as tin ion, to recharge the active ingredient is needed. Hard water, however, may deposit minerals on the tubing—blocking its effectiveness.22 Other agents, such as N-halamine, are being researched with promising results. One study showed that the grafting of N-halamine onto the inner surface of polyurethane tubing resulted in the prevention of bacterial adhesion for up to 4 weeks.27 The study also found that the introduction of diluted chlorine bleach regenerated N-halamine’s effects.
Sterile water delivery systems can effectively prevent the formation of biofilms, but this method is costly and inconvenient for routine dental treatment. Oral surgical procedures, such as biopsies; implant surgery; periodontal surgery; and those requiring mucoperiosteal flaps, suturing, and bone removal, all require sterile water.18 Sterile water is necessary to prevent pathogens in the water from entering the vascular system—increasing the opportunity for localized infection.13 Designed to completely bypass the dental unit, autoclaveable and single-use tubing is available to deliver sterile water. For occasional use, sterile bottled water can be delivered with a handheld, bulb-type syringe.
System Monitoring
Regardless of what system is used, the efficacy of the DUWL disinfection system should be periodically monitored. Monitoring is critical to assess how well the product is functioning and to determine whether procedures are being performed properly. The correct interval for monitoring is determined by the manufacturer of the dental unit or asepsis product. Practitioners can test DUWLs with in-office test kits or through outside testing services. While in-office test kits are convenient, some studies report they may underestimate the number of CFUs present in the water.28-30 In-office testing kits may be better used as screening tools. These kits typically require three separate samples from the same dental unit. Aseptic techniques must be implemented when obtaining the samples in order to prevent contamination. If test results reveal high CFU counts, a review of protocols should be conducted to ensure compliance.
Additionally, shock treatment is warranted to improve overall water quality. If a problem still exists, another agent or product might be considered. As with other forms of office testing, a log of test dates and results should be kept.
Boil-Water Advisories
During a boil-water advisory, water from municipal water supplies cannot be used for patient treatment.31 These advisories are typically associated with bacterial contamination, and they have been become more common due to the rise in floods that cause contamination of water supplies and power outages that interfere with purification systems. When advisories are in effect, dental practitioners should use alcoholbased hand rubs for hand disinfection. If hands are visibly soiled, clinicians should use bottled water with soap. The CDC recommends patients rinse with bottled water or distilled water as long as the boil-water advisory is in effect.31 Units equipped with an independent water reservoir that bypasses the municipal water system are not affected. However, if the bottled water was disseminated through a DUWL previously connected to the affected water supply, flushing and disinfection of the lines are imperative before use. Once the advisory is cancelled, all DUWLs should be flushed for 5 minutes, and followed by disinfection.31
In Summary
Waterline maintenance is an essential component of any infection control program. Dental hygienists play a critical role in ensuring that the water delivered during patient care is safe. Biofilm removal, daily control of microorganisms, regular chemical disinfection, and water quality maintenance and monitoring are all key pieces of the DUWL safety puzzle.
References
- Atlas RM, Williams JF, Huntington MK. Legionella contamination of dental-unit waters. Appl Environ Microbiol. 1995;61:1208-1213.
- Pankhurst CL, Philpott-Howard JN. The microbiological quality of water in dental chair units. J Hosp Infect. 1993;23:167-174.
- Costerton JW, Stewart PS, Greenberg EP. Bacterial biofilms: a common cause of persistent infections. Science. 1999;284:1318-1322.
- Williams HN, Baer ML, Kelley JI. Contribution of biofilm bacteria to the contamination of the dental unit water supply. J Am Dent Assoc. 1995;126:1255-1260.
- Depaola LG, Mangan D, Mills SE, et al. A review of the science regarding dental unit waterlines. J Am Dent Assoc. 2002;133:1199-1206.
- Szymanska J, Sitkowska J, Dutkiewicz J. Microbial contamination of dental unit waterlines. Ann Agric Environ Med. 2008;15:173-179.
- Coleman DC, O’Donnell MJ, Boyle M, Russell R Microbial biofilm control within the dental clinic: reducing multiple risks. Journal of Infection Prevention. 2010;11:192-198.
- Szymanska J. Biofilm and dental unit waterlines. Ann Agric Environ Med. 2003;10:151-157.
- Walker JT, Marsh PD. Microbial biofilm formation in DUWLs and their control using disinfectants. J Dent. 2007;35:721-730.
- Mollarni JA, Harte JA. Cottone’s Practical Infection Control in Dentistry. 3rd ed. Baltimore, Md: Walters Kluwer/Lippincott, Williams and Wilkins; 2010.
- Mills SE. The dental unit water line controversy-defusing the myths, defining the solution. J Am Dent Assoc. 2000;131:1427-1441.
- Coleman DC, O’Donnell MJ, Shore AC, Russell RJ. Biofilm problems in dental unit water systems and its practical control. J Appl Microbiol. 2009;106:1424-1437.
- American Dental Association Council of Scientific Affairs. ADA Statement on Dental Unit Waterlines 2004. Available at: www.ada.org/1856.aspx. Accessed October 4, 2011.
- American Dental Association Council of Scientific Affairs. Dental Unit Water Quality. Available at: www.ada.org/sections/professionalResources/pdfs/cleaning_waterlines.pdf. Accessed September 29, 2011.
- Singh TS, Mabe OD. Occupational exposure to endotoxin from contaminated dental unit waterlines. SADJ. 2009;64:8, 10-14.
- Szymanska J. Exposure to bacterial endotoxins during conservative dental treatment. Ann Agric Environ Med. 2005:12; 153-155.
- Pankhurst CL, Coulter W, Philpott-Howard JN, Surman-Lee S,Warburton F, Challacombe S. Evaluation of the potential risk ofoccupational asthma in dentists exposed to contaminated dental unitwaterlines. Prim Dent Care. 2005;12:53-59.
- Kohn WG, Collins AS, Cleveland JL, Harte JA, Eklund KJ, MalvitzDM; CDC. Guidelines for infection control in dental health-caresettings—2003. MMWR Recomm Rep. 2003;52:1-61.
- Organization for Safety, Asepsis, and Prevention (OSAP). Dental unit waterlines. Available at www.osap.org/?page=Issues_DUWL. Accessed October 10, 2011.
- Cobb CM, Martel CR, McKnight SA, Pasley-Mowry C, ferguson BL: Howdoes time-dependent dental unit waterline flushing affect planktonicbacteria levels? J Dent educ. 2002; 66, 549-555.
- Walker JT, Bradshaw DJ, Fulford MR, Marsh PD. Microbiologicalevaluation of a range of disinfectant products to control mixed-speciesbiofilm contamination in a laboratory model of a dental unit watersystem; Appl Environ Microbiol, 2003; 69: 3327-3332.
- Schel AJ, Marsh PD, Bradshaw DJ, Finney M, Fulford MR, Frandsen E,Ostergaard E, Ten Cate, JM, Moorer WR, Mavridou A, Kamma JJ, MandilaraG,et al. . Comparison of the Efficacies of Disinfectants To ControlMicrobial Contamination in Dental Unit Water Systems in General DentalPractices across the European Union. Appl. Environ. Microbiol. 2006; 72: 1380-1387.
- Mills SE. Dental waterlines: a decade in review. Inside dentistry2(3), 2006. Available at http://www.dentalaegis.com/id/2006/04/dentalwaterlines; a decade in review. Accessed Oct 10, 2011.
- Knight JS, Davis SB, McRoberts JG. The effect of a dental unitwaterline treatment regimen on the shear bond strength of resin-basedcomposite. JADA. 2001; 13:615-619.
- Ritter AV, Leonard RH, Ghaname E. The influence of dental unit waterline cleaners on composite-to-dentin bond strengths. J Am Dent Assoc. 2007; 138: 985-991.
- von Fraunhofer JA, DePaola LG, Kelley JI, Meiller TF. Effect of a dental unit waterline additive on resin bond strengths. Gen Dent. 2004; 52:502-504.
- Luo J, Porteous N, Rechargeable biofilm-controlling tubing materials for use in dental unit water lines. ACS Appl Mater Interfaces. 2011; 24; 3:2895-2903.
- Walker J. Decontamination in dentistry – the times they are a changing. British Journal of Infection Control, 2010; 11: 188-191.
- Bartoloni JA, Porteous NB, Zarzabal LA. Measuring the validity of two in-office water test kits. J Am Dent Assoc. 2006;137: 363-371.
- Morris BF, Vandewalle KS, Hensley DM, Bartoloni JA. Comparison of in-office dental unit waterline test kits. Mil Med. 2010;175:901-906.
- CDC. Infection Control in the Dental Settings. Boil-water advisories and the dental office. Available at: www.cdc.gov/oralhealth/infectioncontrol/factsheets/boilwater.htm. Accessed October 1, 2011.From Dimensions of Dental Hygiene. January 2012; 10(1): 36, 38, 40-41.
| Visit the American Dental Association’s website at www.ada.org/sections/professionalResources/pdfs/cleaning_waterlines.pdffor a list of products used to decontaminate dental unit waterlines, in addition to waterline testing products and service providers. |

