NORTONRSX/ISTOCK/GETTY IMAGES PLUS
NORTONRSX/ISTOCK/GETTY IMAGES PLUS
Dental Caries Reimagined
With a growing body of evidence in preventive dental science and increased focus on patient-centered care, oral health professionals should consider new approaches to caries management.
Dental caries has been known to the human race for thousands of years. The disease has been attributed to angry gods, mischievous demons, and other big or small mystical powers. It has been referred to by different names: “tooth worms” for the holes appearing in the teeth for no apparent reason; “dental gangrene” for the inflammation processes associated with its presence; “tooth decay” for the destruction it causes; and “caries,” the word we use to describe the disease now.1–3 Our understanding of caries has changed greatly with van Leeuwenhoek’s observation of microorganisms, which aided Pastor’s discovery of bacteria-driven fermentation, leading to what we know now: dental caries is a multifactorial disease associated with the demineralization of tooth structure due to acids produced by oral bacteria and fueled by fermentable carbohydrate consumption.1
With the shift in understanding of caries’ etiology, treatment modalities have also changed. Palliative treatment using herbs and magic was replaced by the surgical removal of the decayed tissues. With the development of modern dentistry, the extractive phase of caries treatment transitioned into the restorative phase with the goal of preserving the dentition whenever possible.4 Inadvertently, dentistry entered what is known as a “repeat restorative cycle:” a small filling is applied to replace and restore a lesion, leading to a larger filling over time. The large filling is, subsequently, replaced by a crown, often accompanied by endodontic care and then by a fixed or removable prosthetic option.4 The purpose of this review is to help clinicians break out of the repeat restorative cycle and enter the age of noninvasive, preventive dentistry. After all, the final shift toward prevention has been a long time coming. In 1886, G.V. Black, DDS, said “the day is surely coming… when we will be engaged in practicing preventive, rather than reparative dentistry.”1
Demineralization Chemistry in Brief
A human tooth is a complex structure with multiple, functional layers composed of organic and inorganic components. The three main layers—enamel, dentin, and cementum—are initially formed through the biological scaffolding and subjected to a lifelong cycle of losing and gaining mineral content.5 Mature enamel is the first layer of defense against external forces affecting the oral cavity. Enamel is a largely (96%) inorganic hard structure composed of hydroxyapatite crystals [Ca5(PO4)3(OH)] permeated with fluoride, other trace minerals, and supplemented with a small amount of organic matter and water. The enamel apatite crystals are organized into elongated prisms (enamel rods). The highly inorganic content provides strength to the overall structure, yet it appears to be the Achilles heel of the enamel at the same time. Once formed, enamel loses its regenerative capacity and can no longer be repaired from within. Demineralization is “the process of removing mineral ions from hydroxyapatite crystals.”6 It begins with the exposure of the tooth surface to bacteria-produced acids. Uninterrupted acid-enamel interaction leads to the dissolution of mineral ions within the enamel, causing surface destruction and, eventually, cavitation.7 Knowing the mechanisms involved in demineralization, can the process be disrupted with preventive measures or reversed by triggering enamel remineralization, as Black would have hoped?1
Knowing Your Enemy: Assessing and Recording Demineralization
Both clinical and radiographic examinations contribute to the detection of demineralization. However, clinicians mostly rely on clinical examinations for the detection of early lesions, as a substantial amount of mineralized tissue must be lost before the radiolucency is observed on a radiograph. Long gone is the time when an explorer was used to identify demineralized tooth surfaces. As such, other options are used to not only assess the presence and extent of demineralization but also to determine whether the process is active or arrested.
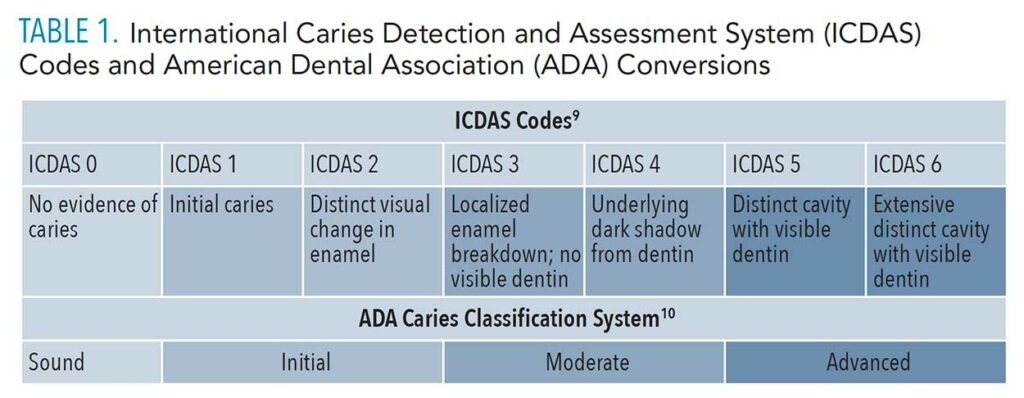
With the absence of a validated approach to detect noncavitated lesions, oral health professionals hovered in a realm of “watch” vs “restore” for some time. The arrival of the International Caries Detection and Assessment System (ICDAS) provided an opportunity to reliably assess and record the “watches.”8 ICDAS is a caries assessment and recording tool incorporated into a concept of caries management referred to as the International Caries Classification and Management System (ICCMS). Using this tool, oral health professionals can track the demineralization and adjust their preventive recommendations based on its active or arrested status. The organization’s website offers quality educational and calibration resources. A summary of the ICDAS codes and their conversion to the American Dental Association (ADA) Caries Classification System are provided in Table 1.9,10
Averting the Battle: Caries Risk Assessment
In addition to assessing and recording the presence of demineralization, oral health professionals can evaluate caries risk and adopt evidence-based measures to modify identified risk factors. This provides a unique opportunity to prevent the loss of enamel mineral content in the first place. Risk assessments have been slowly making their way into healthcare as part of personalized care planning. The role of caries risk assessment in demineralization prevention and management is trifold. The assessment offers guidance regarding which diagnostic procedures are needed, provides personalized caries control and prevention strategies, and aids in care planning. The use of reliable, user-friendly tools is highly encouraged over casual risk assessment methods. The web version of this article includes a list some of the caries risk assessment protocols currently available.
Overview of Existing Remineralization Strategies
Fluoride treatment has long been viewed as the gold standard of prevention and remineralization.11 Studies have established the preventive effect of toothpastes containing a higher concentration of fluoride (1,000 ppm and above). In cases where children’s toothbrushing habits were supervised by adults, the preventive effects of fluoride toothpastes were even more pronounced.12 Caries reduction action was also demonstrated by fluoride mouthrinses and high-concentration gels.13 Although the preventive qualities of fluoride are well-documented in research, its ability to reverse active demineralization is not as widely investigated.14 However, research confirms significant remineralization effect of fluoride toothpastes with higher concentrations of fluoride (5,000 ppm).11 Fluoride varnishes have also been proven to be successful in remineralization in both primary and permanent dentition.14
Clinicians were reminded of the antimicrobial properties of fluoride with the re-emergence of silver diamine fluoride (SDF), an effective remineralization agent that acts within enamel and dentin alike.15,16 However, more research is needed to evaluate the efficacy and side effects of SDF.17 Stannous fluoride’s (SnF2) antimicrobial properties have been widely recognized and confirmed through laboratory data and are commonly employed via commercially available toothpastes.18 Fluoride is the prevailing therapeutic and preventive agent and can be delivered through a variety of preparations. A thorough assessment of the patient’s caries risk level, as well as health behaviors should assist in choosing the appropriate fluoride-based remineralization therapy.
Sealants serve as an effective barrier, protecting the most vulnerable parts of the tooth from cariogenic forces. The preventive qualities of sealants used in child and adolescent populations are strongly supported by evidence.19 Adults can benefit from sealant placement as well. Clinical follow-up is needed in all population groups to assure the integrity of sealant placement.20 While the preventive value of sealant placement is widely recognized, there is also a substantial remineralization effect that is often overlooked. Evidence suggests that early (noncavitated) caries lesions may be arrested when sealed and may also remain arrested over time.21 The key to remineralization success is careful monitoring and immediate repair if needed.
Saliva influences the process of caries development along many trajectories. It is the medium for minerals intimately involved in the remineralization process as well as nutrients for the healthy microbiota.22,23 Furthermore, it buffers acids and contributes to an overall cleansing apparatus for the mouth. Saliva also contains various proteins and peptides with known antibacterial properties.22 Salivary flow and its composition are critical in caries prevention and remineralization processes.4 Salivary characteristics can be negatively affected by a multitude of factors such as medications, hormonal imbalances, and diet. Xerostomia disrupts the prevention and remineralization of caries.
Over-the-counter and prescription saliva stimulants and substitutes should be recommended to combat xerostomia.23 Sugar-free chewing gum can be a good option as it is readily available to the consumer. Prescription saliva stimulants can be discussed with the patient and the patient’s dentist.4 A few alternative treatments and stimulating techniques have been discussed in the literature, including acupuncture, lasers, and mild electrical stimulation.24 Reliable evidence to support any of these techniques is yet to be identified. Longer-duration acupuncture care appears to slightly increase salivary flow in certain populations.24 The identification of salivary deficiencies is critical to supporting any prevention and remineralization efforts.
The idea of using “good” bacteria in the fight against bad ones is not new. Two known groups, lactobacilli and bifidobacteria, were explored in caries-related research.25 L. paracasei and L. rhamnosus strains appear to demonstrate the highest antimicrobial potential. L. salivarius should be mentioned as well, as it can reduce pathogenicity of oral bacteria.26 The effects of intraoral probiotic intake were more pronounced when fluoride supplementation was present.25 Various probiotic regimens have promoted a reduction in caries risk and incidence in children and the reversal of root caries in elderly populations in small-scale studies.25 The majority of research on probiotics focuses on the reduction of cariogenic bacteria rather than the direct effect on caries. However, the probiotic market is not well regulated in the United States,26 and manufacturers often add sweeteners to intraoral probiotic supplements for better palatability.26 While awaiting the outcomes of large in vivo studies, it is important to educate patients on emerging probiotic products and their role in caries prevention.
Although a caries vaccine is not yet accessible, chemicals that affect the ecology of biofilm are commercially available.28 Arginine, an amino acid that influences the ecosystem of dental biofilm, appears to trigger the remineralization of coronal and root surfaces when added to a toothpaste and supported by calcium and fluoride supplementation.11,29 Calcium phosphate technologies may reduce bacterial colonization and support the remineralization of tooth structure.30
Xylitol, a sugar alcohol found in plants, has been widely used as an antimicrobial with some degree of cariostatic effect.31 Unfortunately, the remineralization properties of xylitol-containing products are yet to be well-explored in research.11
Chlorhexidine, the gold standard of oral antiseptics, has many uses in dentistry. Its cariostatic effect is associated with its biocidal properties.32 Chlorhexidine rinses and varnishes should be considered for the prevention of caries when fluoride is not a suitable option.33
Lasers joined the dental toolkit in the 1960s.34 With improved knowledge of laser-tooth surface interactions, it was just a matter of time before lasers were considered as a potential remineralization aide. Although existing research is limited, it appears that the photothermal effect of lasers in the presence of fluoride, calcium, and phosphate ions may assist in the rapid mineralization of compromised enamel surfaces.35 Promising results were seen in both permanent and primary dentitions.35,36 However, the mechanism of laser-assisted mineralization has only been explored in vitro.35–37 More substantial research is needed in order to create clinically viable protocols for laser-aided remineralization.
The Cavity-free World
Since ancient times, caries has remained a heavy burden on human health and well-being. With the rise of preventive dental science and increased focus on patient-centered care, oral health professionals should adopt new preventive and preservation approaches to caries management. Evidence-supported efforts in assessing the risk of caries development, monitoring caries activity, and the use of patient-centered prevention and remineralization strategies can turn the vision of a cavity-free world into a reality.
References
- Ruby JD, Cox CF, Akimoto N, Meada N, Momoi Y. The caries phenomenon: a timeline from witchcraft and superstition to opinions of the 1500s to today’s science. Int J Dent. 2010;2010:1–10.
- Littman H. Cariology: theories past and present. Compendium. 1993;14(6):748–750.
- Caselitz P. Caries—ancient plague of humankind. Dental Anthropology. 1998:203-226.
- Pitts NB, Zero DT. White paper on dental caries prevention and management. FDI World Dental Federation. 2016:3–9.
- Abou Neel EA, Aljabo A, Strange A, et al. Demineralization–remineralization dynamics in teeth and bone. Int J Nanomedicine. 2016;11:4743–4763.
- Moradian-Oldak J. Protein-mediated enamel mineralization. Frontiers in Bioscience. 2012;17:1996.
- Dorozhkin SV. Dissolution mechanism of calcium apatites in acids: a review of literature. World J Methodol. 2012;2:1–17.
- Ismail AI, Sohn W, Tellez M, et al. The International Caries Detection and Assessment System (ICDAS): an integrated system for measuring dental caries. Community Dent Oral Epidemiol. 2007;35:170–178.
- ICDAS Foundation. ICCMS Caries Management. Available at: iccms-web.com. Accessed November 20, 2020.
- Young DA, Nový BB, Zeller GG, et al. The American Dental Association caries classification system for clinical practice: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2015;146:79–86.
- González-Cabezas C, Fernández CE. Recent advances in remineralization therapies for caries lesions. Adv Dent Res. 2018;29:55–59.
- Walsh T, Worthington HV, Glenny AM, Appelbe P, Marinho VC, Shi X. Fluoride toothpastes of different concentrations for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2010;1:CD007868.
- Marinho VC, Higgins JP, Logan S, Sheiham A. Topical fluoride (toothpastes, mouthrinses, gels or varnishes) for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2003;4:CD002782.
- Lenzi TL, Montagner AF, Soares FZM, de Oliveira Rocha R. Are topical fluorides effective for treating incipient carious lesions?: a systematic review and meta-analysis. J Am Dent Assoc. 2016;147:84–91.
- Gao SS, Zhang S, Mei ML, Lo ECM, Chu CH. Caries remineralisation and arresting effect in children by professionally applied fluoride treatment–a systematic review. BMC Oral Health. 2016;16:12.
- Wierichs RJ, Meyer-Lueckel H. Systematic review on noninvasive treatment of root caries lesions. J Dent Res. 2015;94:261–271.
- Rajendra A, Oliveira BH, Ruff RR, et al. Topical silver diamine fluoride for managing dental caries in children and adults. Cochrane Database of Systematic Reviews. 2017;2017:7.
- Fernández CE, Fontana M, Samarian D, Cury JA, Rickard AH, González-Cabezas C. Effect of fluoride-containing toothpastes on enamel demineralization and Streptococcus mutans biofilm architecture. Caries Res. 2016;50:151–158.
- Ahovuo‐Saloranta A, Forss H, Walsh T, Nordblad A, Mäkelä M, Worthington HV. Pit and fissure sealants for preventing dental decay in permanent teeth. Cochrane Database Syst Rev. 2017;7:CD001830.
- Alves LS, Giongo FCM de S, Mua B, et al. A randomized clinical trial on the sealing of occlusal carious lesions: 3–4-year results. Braz Oral Res. 2017;31:e44.
- Fontana M, Platt JA, Eckert GJ, et al. Monitoring of sound and carious surfaces under sealants over 44 months. J Dent Res. 2014;93:1070–1075.
- Dawes C, Pedersen AML, Villa A, et al. The functions of human saliva: A review sponsored by the World Workshop on Oral Medicine VI. Arch Oral Biol. 2015;60:863–874.
- Roblegg E, Coughran A, Sirjani D. Saliva: an all-rounder of our body. Eur J Pharm Biopharm. 2019;142:133–141.
- Furness S, Bryan G, McMillan R, Worthington HV. Interventions for the management of dry mouth: non‐pharmacological interventions. Cochrane Database Syst Rev. 2013;9:CD009603.
- Twetman S, Keller MK. Probiotics for caries prevention and control. Adv Dent Res. 2012;24:98–102.
- Teughels W, Van Essche M, Sliepen I, Quirynen M. Probiotics and oral healthcare. Periodontol 2000. 2008;48:111–147.
- National Center for Complementary and Integrative Health. Probiotics: What You Need To Know. Available at: nccih.nih.gov/health/probiotics/introduction.htm. Accessed November 20, 2020.
- Patel M. Dental caries vaccine: are we there yet? Lett Appl Microbiol. 2020;70:2–12.
- Cummins D. The superior anti-caries efficacy of fluoride toothpaste containing 1.5% arginine. J Clin Dent. 2016;27:27–38.
- Compton R. Opportunities to increase prevention in dentistry. J Dent Hyg. 2015;89(Suppl 1):30–32.
- Riley P, Moore D, Ahmed F, Sharif MO, Worthington HV. Xylitol‐containing products for preventing dental caries in children and adults. Cochrane Database Syst Rev. 2015;3:CD010743.
- Karpiński TM, Szkaradkiewicz AK. Chlorhexidine–pharmaco-biological activity and application. Eur Rev Med Pharmacol Sci. 2015;19:1321–1326.
- Rethman MP, Beltrán-Aguilar ED, Billings RJ, et al. Nonfluoride caries-preventive agents: executive summary of evidence-based clinical recommendations. J Am Dent Assoc. 2011;142:1065–1071.
- Verma SK, Maheshwari S, Singh RK, Chaudhari PK. Laser in dentistry: an innovative tool in modern dental practice. Natl J Maxillofac Surg. 2012;3:124.
- Sun M, Wu N, Chen H. Laser-assisted rapid mineralization of human tooth enamel. Sci Rep. 2017;7:9611.
- Valério RA, Rocha CT, Galo R, Borsatto MC, Saraiva M da CP, Corona SAM. CO2 laser and topical fluoride therapy in the control of caries lesions on demineralized primary enamel. ScientificWorldJournal. 2015;2015:547569.
- Ceballos-Jimenez AY, Rodriguez-Vilchis LE, Contreras-Bulnes R, Alatorre JÁA, Velazquez-Enriquez U, Garcia-Fabila MM. Acid resistance of dental enamel treated with remineralizing agents, Er: YAG laser and combined treatments. Dent Med Probl. 2018;55:255–259.
From Dimensions of Dental Hygiene. December 2020;18(11):16, 18, 21.