 DECADE3D / ISTOCK / THINKSTOCK
DECADE3D / ISTOCK / THINKSTOCK
Caring For Patients With Hearing Impairment
Clinicians need to be prepared to provide effective oral health services to this patient population.
This course was published in the July 2016 issue and expires July 31, 2019. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- List the types of hearing loss.
- Identify the causes of hearing loss.
- Discuss the types of hearing assistance.
- Describe the methods available to properly communicate and treat patients with hearing impairment.
Hearing loss is defined as the partial or complete loss of hearing in one or both ears.5 When hearing becomes impaired to the degree that the practical value of audio communication is lost, an individual is considered deaf. Defective but still functional hearing (with or without a hearing aid) defines an individual with a hearing impairment.6,7 The World Health Organization (WHO) estimates that 360 million people around the globe have some form of hearing loss—32 million of whom are children.8 Hearing loss is the third most common global health problem. While only 5% of people age 18 to 45 have hearing deficiencies,3 nearly one out of every three people older than 60 have some form of hearing loss.5
Hearing impairment is a common disability among children.9 In the United States, four out of every 1,000 infants are born deaf. More than 70,000 American children receive hearing services under the Individuals with Disabilities Education Act.10 Hearing deficits in childhood are associated with difficulties in developing communication skills, particularly speech. Social and emotional development, as well as the ability to learn are impaired,5,7 which can lead to decreased academic performance.3,7 As the degree of hearing loss increases, emotional, social, and psychological issues become more pronounced.2,9 The extent of such problems depends on the age of hearing-impairment onset, success of training in alternative communication methods, and the family’s and child’s acceptance of the disability.
TYPES OF HEARING LOSS
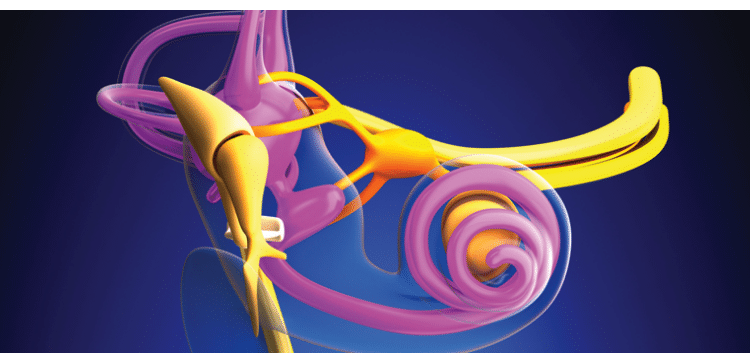
Anatomic causes of hearing are typically associated with aberrations in the outer, middle, or inner ear, or a combination (Figure 1).6 There are four types of hearing loss: conductive, sensorineural, mixed, and central.6 Conductive hearing loss occurs when sound is not effectively conducted through the outer and middle ears to the inner ear.6 It is characterized by a decrease in sound volume and the inability to hear faint sounds. Typically caused by earwax, foreign body, or retained tissue fluid in the ear canal, conductive hearing loss may be related to allergies, ear infections, or poorly functioning Eustachian tubes. This type of hearing loss can generally be corrected with medication or surgery.3
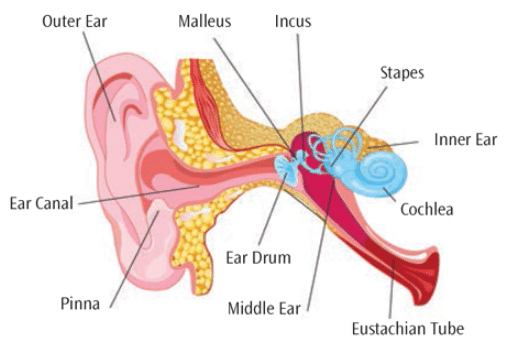
Sensorineural hearing loss results from damage to the sensory hair cells in the inner ear or nerves that supply the inner ear.6 Patients with this type experience loss of volume and trouble discriminating between speech sounds. This hearing loss is permanent.3 Globally, the leading cause of sensorineural hearing loss is chronic ear infections;8 however, in the US, the most common etiology is presbycusis, or the gradual and progressive loss of hearing due to the aging process or noise damage.2,11 Other causes include disease or genetic syndromes, tumors, infectious diseases (eg, Rubella, meningitis), birth defects, or head trauma.3 Multiple medications can adversely affect the auditory system, including: aminoglycoside antimicrobials, chemotherapies, loop diuretics, aspirin,11 and anti-malarial agents.8 Systemic disease has also been linked to this type of hearing loss—namely hypertension, hyperlidemia, and diabetes mellitus (especially when diabetes is uncontrolled or in conjunction with smoking).11
Mixed hearing loss is a combination of conductive and sensorineural hearing loss.6 Central hearing loss occurs when there is damage to the central nervous system that adversely affects nervous pathways to the brain.6 These include the effects of tumors, genetics, systemic diseases, or idiopathic factors. This type involves problems with identifying the location of sounds, discriminating between different sounds, inability to recognize auditory patterns, competing signals, or changes in tones and volumes. Because this type of hearing loss involves nerve damage, the condition is permanent.3
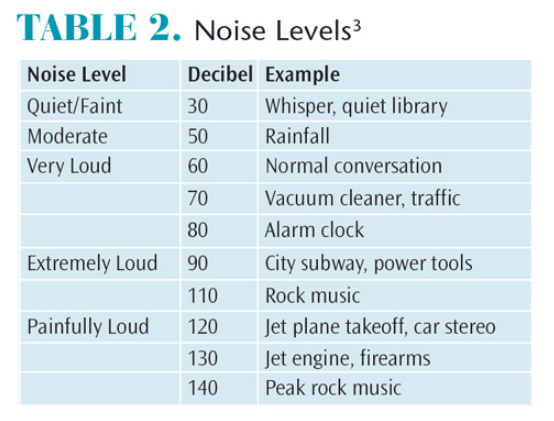
The severity of hearing loss is described by the lowest volume, measured in decibels (dB), that can be heard.3 Severity of hearing loss is grouped into degrees: mild, moderate, severe, and profound.7 A patient’s degree of hearing loss will influence the quality and quantity of his or her hearing ability and preferred method of communication (Table 1).1 Hearing loss can further be described as bilateral or unilateral, and progressive (worsens over time vs sudden, perhaps resulting from head trauma or an extremely loud noise or atmospheric overpressure).3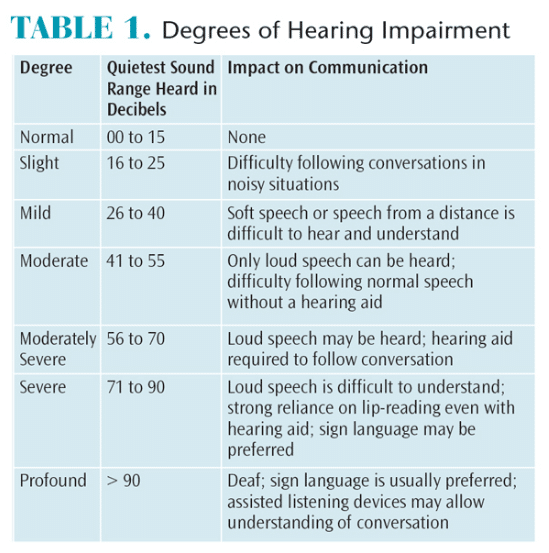
NOISE LEVELS
Noise levels greater than 80 dB are considered detrimental to the auditory system.3 Both the length of time exposed to loud noises and the amplitude of noises contribute to hearing loss.3 The WHO estimates that 1.1 billion people are at risk of developing sensorineural hearing loss due to unsafe listening practices.8 Common sounds such as city traffic become hazardous to hearing after 8 hours; exposure to loud stereos, personal music players, rock concerts, or night clubs can be damaging after only 15 minutes (Table 2).11 Hearing protection from loud or chronic noise exposures is recommended to prevent hearing loss.11
Occasionally, hearing loss is accompanied by tinnitus, or ringing in the ears. This may be related to an undiagnosed systemic illness, such as Meniere disease, but is often caused by sudden damage to the auditory system, which may contribute to permanent hearing loss.11 Fifty percent of all sensorineural hearing loss is preventable via a combination of vaccinations against relevant infectious diseases, effective treatment for acute and chronic ear infections, and healthy hearing habits.8
HEARING ASSISTANCE
Several devices can help patients with mild to severe sensorineural hearing loss improve their hearing by magnifying or clarifying sounds or by enhancing sound conduction through the ear.12 Hearing aids are small electronic devices that amplify and shape sound waves before they enter the external ear.6 A hearing aid receives sounds, converts the sound waves to electrical signals, and sends them to a device that can amplify or otherwise modify sound signals destined for the ear.12 Although technological advances have resulted in smaller sized hearing aids and better sound qualities,11 only one in five patients who would benefit from a hearing aid has one. There are several styles of hearing aids, such as behind-the-ear, in-the-ear, and in-the-canal options.12
A cochlear implant is a complex electronic device that provides hearing for patients who are deaf. The implant consists of an outer piece that sits behind the ear and a surgically placed piece under the skin. The implant directly stimulates the auditory nerve, bypassing a faulty inner ear.13
An implantable device that combines a sound processor behind the ear and an osseointegrated implant is also available for individuals with profound hearing loss. This technology allows the transfer of sound waves through the bone directly to both the cochlea and the middle ear. This device is especially useful to treat hearing loss in patients whose deafness has been caused by malformation of the middle ear, chronic infections, or systemic diseases.14
For patients with unilateral deafness, an intraoral hearing system that uses the teeth and nearby bone to conduct sound to the inner ear may be an option.11,15 It consists of a removable intraoral microphone and a microphone worn behind the ear. In order for proper placement of the intraoral piece, the abutment teeth must be free of caries, periodontitis, and endodontic lesions.11 Some patients reported oral mucosa sores; however, these lesions resolved promptly after adjusting the fit of the appliance and when meticulous oral hygiene was enacted.15
ORAL MANIFESTATIONS
Several studies assess specific oral characteristics of deaf children and adolescents, finding they have an increased prevalence of caries and gingival inflammation, are more prone to develop periodontitis earlier in life, and tend to have poor oral hygiene and be mouth breathers (typically with xerostomia).5,10,16,17 Worldwide, dental caries is the most widespread disease in children younger than 18, and children with disabilities are at an even higher risk. Indeed, preventive and restorative dental treatments are the greatest unattended health needs in children with disabilities.
Poor oral health and pronounced gingival inflammation are common among adults with hearing impairments, thus raising their risk for caries and periodontitis. Adults with hearing impairment frequently report they do not understand how to prevent caries and periodontitis because of problems communicating with their oral health professionals.10 Auditory challenged adults also describe feelings of dental fear and anxiety.11
Slight to moderate hearing loss may go undiagnosed, especially in older adults. Oral health professionals should be aware of behaviors that may indicate a patient is having difficulty hearing, such as lack of attention and failure to respond to questions, strained facial expressions and staring when listening, turning head to one side, giving unexpected answers to questions or doing one thing when asked to do another, unusual speech quality or volume, frequent requests for the speaker to repeat what was said, and an inability to repeat information previously conveyed, such as oral hygiene instructions.6 Clinicians should be careful not to confuse a patient’s struggle to hear and communicate appropriately as disrespect, lack of interest, or impaired cognitive function.11
COMMUNICATION IS KEY
Oral health professionals must make concerted efforts to effectively communicate with patients with hearing loss in order to understand their oral needs and improve self-care, in addition to ensuring patients can make informed decisions regarding treatment.4,11 Patients with auditory impairments are legally entitled to the same information and treatment as hearing patients,9 and communication efforts should be tailored to each patient’s preferences.4
Successful communication is needed for medical history reviews, obtaining informed consent, explaining oral findings and treatment options, and patient education. Good communication builds trust and tends to ease patient anxiety. This can lead to better patient experiences and fewer misunderstandings, complaints, and potential legal issues.1,4
Body language and facial expressions transfer at least 60% of the total messaging that accompanies vocal tone and words when communicating with patients who have auditory impairments.1 For patients with slight to moderately severe hearing loss, several steps can be taken to improve communication and enhance outcomes. Appointment scheduling and confirmation may be best conducted in-writing via postal mail, electronic mail, or text messaging.3 Clinicians should plan adequate appointment time for these patients because extra time is often needed for effective communication. Moving to a place in the practice that is relatively isolated from typical office noise is best.1 Furthermore, background music should be turned off and windows closed to minimize outside noise. If the patient has unilateral hearing loss, speak to the side of the patient with the better hearing capabilities. Facing the patient at the same horizontal level may help. Clinicians may also lean slightly forward in the operating chair to nonverbally signal interest and attention. Maintaining eye contact and making encouraging gestures (eg, “thumbs up”) will indicate active listening. Clinicians should avoid communicating with patients while wearing surgical masks.1
A lower vocal pitch is often easier for patients with hearing impairment to comprehend; however, loud volume is not necessarily helpful.1 Speaking clearly but not overly slow, while avoiding exaggerated lip movements or enunciation is preferred. Clinicians should also seek to avoid negative body language or facial expressions.1
Oral self-care should be demonstrated in a patient’s own mouth while he or she observes in a hand mirror. Disclosing solution may serve as a motivator to improve oral habits. Visual aids are helpful when explaining different disease processes. Written brochures on proper brushing and flossing instructions can be useful for adults.3 During patient education, try to avoid using jargon or overly technical terminology and ask the patient to repeat what was said. This will help evaluate the patient’s hearing and comprehension. If a patient asks to have some information repeated, try saying it in a different way.1
Hearing aids also amplify other sounds in the treatment area. Thus, assure the area remains quiet, free of background music or television. Try to avoid unnecessary shifting of instruments, and turn off the saliva ejector when it’s not in use. Because the hearing aid magnifies sounds from the ultrasonic scaler and handpiece, ask the patient to turn aids down or off during equipment use.3
Patients with severe or profound hearing loss nearly always prefer a particular method of communication. Office staff should confirm the patient’s preferred method and work as a team to treat the patient based on his or her preferences, in compliance with the Americans with Disabilities Act.4,6 If a patient requests an American Sign Language (ASL) interpreter, the dental office is legally required to provide one. Interpreters are able to help office staff fully understand a patient’s concerns and symptoms, secure informed consent, and help ensure effective treatment, especially for more invasive procedures.4 If using an ASL interpreter, always look directly at the patient when speaking—not at the interpreter.1
Despite looking directly at the patient and working to enunciate clearly, lip reading can be problematic in part because only 30% of sounds in the English language can be inferred by observing the lips. Different dialects and facial expressions can further complicate effective comprehension.3 In short, lip reading is not reliable for a lengthy conversation or conveying new or complex information, nor is it legally acceptable for obtaining informed consent.6
Writing is often an effective method of communication; however, clinicians need to plan for longer appointments to permit such time-consuming attempts at communication.3 Advances in technology allow written communication to occur using differing means (eg, handwriting, typing, or text messaging). Language should be kept simple so the conversation can move easily.3 Writing with paper and pen is best performed with a clipboard. Remember to spell correctly and write legibly.6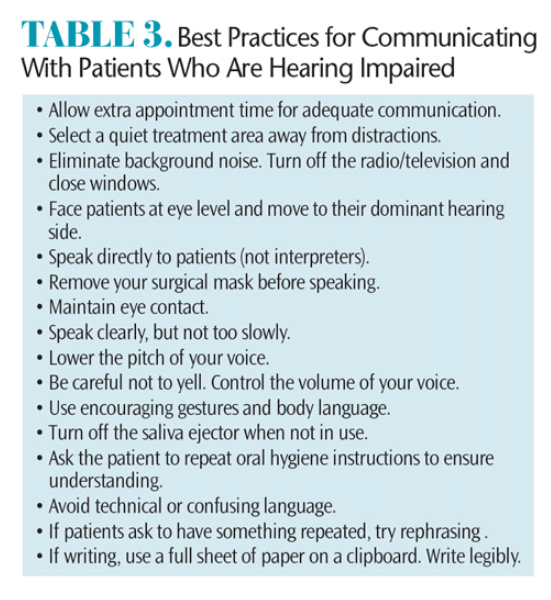
Computers in dental operatories also allow clinicians to type with patients. To maintain the chain of asepsis, barrier the keyboard so it can be easily disinfected. Open a typing program and alternate turns with the keyboard. This is ideal when keyboards are wireless and can be passed between users. Cell phones allow clinician and patient to communicate via instant messaging. Children and adolescents with hearing loss respond well to text messaging, especially if they are not proficient with ASL. Table 3 lists additional suggestions for improving communication with patients who are hearing impaired.
Parents/caregivers should be involved in oral hygiene instructions for children with hearing impairment.1,18 Research indicates that providing dual parent-child brushing education helps significantly reduce plaque indices at a deaf child’s recare appointment.18 The clinician will need to remain flexible with teaching methods when communicating with children/adolescents with auditory impairments. After several appointments, both the patient and practitioner typically develop good rapport.10 While written instructions are useful for adults, brochures and pamphlets are ineffective for children and adolescents. Video clips for oral hygiene instructions, especially when played repeatedly, can be effective at reducing plaque scores and gingivitis in deaf teenagers.17,18
CONCLUSION
When patients cannot hear clearly, clinical management must be modified to meet their needs. Clinicians should be compassionate and understanding when working with patients who are hearing impaired and allow additional treatment time for effective communication and patient education.9 Simple modifications to communication styles will allow hearing impaired patients to feel at ease during treatment and leave the office fully comprehending their oral status.19
References
- Dougall A, Fiske J. Access to special care dentistry, part 2: Communication. Br Dent J. 2008;205:11–21.
- Ciorba A, Bianchini C, Pelucchi S, Pastore A. The impact of hearing loss on the quality of life in elderly adults. Clin Interven Aging. 2012;7:159–163.
- Darby ML, Walsh MW. Persons with neurologic and sensory disabilities. Dental Hygiene Theory and Practice. 2nd ed. St. Louis: Saunders; 2003:794–815.
- Sfikas PM. Serving the hearing impaired. J Am Dent Assoc. 2001;132:681–683.
- University of Washington School of Dentistry. Oral Health Fact Sheet for Dental Professionals. Available at: dental.washington.edu/oral-medicine/special-needs/Patients-with-special-needs. Accessed June 9, 2016.
- Wilkins EM. The patient with a sensory disability. Clinical Practice of the Dental Hygienist. 9th ed. Philadelphia: Lippincott Wilkins & Williams; 2005:948–959.
- Stevens G, Flaxman S, Brunskill E, Mascarehnas M, Mathers CD, Finucane M. Global and regional hearing impairment prevalence: an analysis of 42 studies in 29 countries. Eur J Pub Health. 2011;23:146–152.
- World Health Organization. Deafness and Hearing Loss. Available at: who.int/topics/deafness.en. Accessed June 9, 2016.
- Shetty V, Kumar J, Hedge A. Breaking the sound barrier: oral health education for children with hearing impairment. Special Care Dent. 2014;34:131–137.
- Bimstein E, Jerrell RG, Weaver JP, Dailey L. Oral characteristics of children with visual and auditory impairments. Ped Dent. 2014;36:336–341.
- Waldron SK. Auditory sensory impairments and the impact on oral healthcare: a review of the literature. Canadian Journal of Dental Hygiene. 2011;45(3):180–184.
- National Institute of Deafness and Other Communication Disorders. Hearing Aids. Available at: nidcd.nih.gov/health/hearing-aids. Accessed June 9, 2016.
- National Institute of Deafness and Other Communication Disorders. Cochlear Implants. Available at: nidcd.nih.gov/health/cochlear-implants. Accessed June 9, 2016.
- Johns Hopkins Medicine. Baha—the implantable hearing device. Available at: hopkinsmedicine.org/ hearing/hearing-aids/baha.html. Accessed June 9, 2016.
- Gurgel RK, Shelton C. The SoundBite hearing system: Patient-assessed safety and benefit study. The Laryngoscope. 2013;123(11):2807–2812.
- Jain M, Mathur A, Kumar S, Dagle, RH, Duraiswamy P, Kulbarn S. Dentition status and treatment needs among children with impaired hearing attending a special school for the deaf and mute in Udaipur, India. J Oral Sci. 2008;50:161–165.
- Sandeep V, Vinay C, Madhuri V, Veerabhadra Rao V, Uloopi KS, Chandra Sekar R. Impact of visual instruction on oral hygiene status of children with hearing impairment. Journal of Indian Society of Pedodontics and Preventative Dentistry. 2014;32(1):39–43.
- Pareek S, Nagaraj A, Yousuf A, Ganta S, Mansi A, Singh K. Effectiveness of supervised oral health maintenance in hearing impaired and mute children—a parallel randomized controlled trial. Journal of International Society of Preventative and Community Dentistry. 2015;5(3):176–182.
- San Bernardino-Alsmark S, de Nova Garcia J, Martinez MRM, Lopez NEG. How to improve communication with deaf children in the dental clinic. Med Oral Patol Oral Cir Bucal. 2007;12:E578–581.
From Dimensions of Dental Hygiene. July 2016;14(07):44–47.