
Cancer Care
Here are proven strategies to treat patients with head and neck cancer before, during, and after cancer therapy.
This course was published in the September 2010 issue and expires September 2013. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Understand the guiding principles of motivational interviewing.
- Discuss how the principles of motivational interviewing impact oral health education.
- Identify the five stages of change and how each stage relates to behavior change.
- Critically assess how motivational interviewing and traditional oral health education approaches differ.
Patients with cancer are being diagnosed earlier and living longer than ever before mostly due to early detection. Current prevention, diagnosis, treatment, and recovery depend on the efforts of a multidisciplinary team of health care professionals. The team may include the patient’s surgeon, oncologist, physician, nutritionist, dentist, and dental hygienist.
Malignancies of the head and neck comprise about 10.35% of all cancers, with the highest incidence of 16.1% occurring among black men.1 The average 5-year survival rate for head and neck cancers is 62.2%, with white women having the highest survival rate and black men the lowest.1
Squamous cell carcinoma, which originates in the cells that make up the lining of the nose, throat, and mouth, is the most common form of head and neck cancer.2 Salivary gland tumors, lymphomas, and sarcomas are more rare.2 Table 1 lists some of the different types of head and neck cancers. Patients2 may also undergo treatment to the head and neck area for other types of cancers, such as tumors of the salivary and parotid glands as well as lymphomas.
Head and neck radiation and surgery are the standard treatment options for these types of cancers.2,3 Chemotherapy is used to reduce the risk of the cancer spreading, to increase the efficacy of radiation on the malignant cells, and if the cancer has already metastasized.3 These treatments can have profound effects on patients’ oral health, thus, the dental hygienist is an important component of the health care team for these patients.
The Treatment
Head and neck radiation therapy is used to destroy abnormal cancer cells. Although effective in the fight against cancer, the therapy can also injure normal, healthy cells at the same time. Table 2 lists the adverse oral side effects associated with radiation therapy of the head and neck.4 Chemotherapy uses drugs to kill rapidly dividing cancer cells at different points in the cell cycle. The drugs can be used as a single agent or in combination. Side effects can be severe and frequently involve the oral cavity.5 Table 3 lists the oral complications associated with chemotherapy.5
ORAL SIDE EFFECTS
Although many oral conditions are associated with the treatment of head and neck cancer, oral mucositis is one of the most common and can be the most serious. Oral mucositis is an inflammation of the mucous membranes within the oral cavity. Typically, it appears as red, burn-like or ulcer-like sores and affects oral tissues such as the gingiva, tongue, hard and soft palate, floor of the mouth, and tissues inside the lips and cheeks. Oral mucositis also includes infections of the mucous membranes.6 It occurs in almost all patients undergoing stem cell transplantation, radiation therapy to the head and neck, and chemotherapy.7 Chemotherapy-related mucositis is extremely painful and it increases the patient’s risk of systemic infections by odontopathic, periodontopathic, and transient oral microorganisms.8 Symptoms can become so severe that cancer treatment may be discontinued until the oral cavity has healed. Significantly more patients with mucositis (59%) require unplanned delays/breaks in cancer therapy than those without mucositis (16%).9
TABLE 1. SOME TYPES OF HEAD AND NECK CANCERS.
- Cancers of the oral cavity
- Lips, floor of the mouth, buccal mucosa, tongue, hard and soft palate, gingiva
- Oropharynx
- Tonsils, base of the tongue, pharyngeal wall
- Nasopharynx
- Uppermost part of the pharynx
- Larynx
- Voice box
Mouth soreness and erythema generally start within 2 weeks of beginning chemotherapy treatment. More severe damage to the oral mucosa often develops within 2 more weeks.10 Inadequate nutrition is also associated with mucositis due to the patient’s inability to eat. However, the severity of mucositis caused by radiation therapy is generally dependent on the patient’s level of oral hygiene.11
Xerostomia in patients undergoing head and neck radiation is caused by damage to the salivary glands. Saliva has many properties and functions, particularly to buffer acids and to supply minerals to replace calcium and phosphate ions dissolved from the tooth during demineralization.4 Saliva is also key in the dissemination of fluoride.4 A decrease in saliva production and flow increases patients’ risk of caries.
Osteoradionecrosis is a serious risk for those undergoing radiation therapy to the head and neck region. The therapy compromises blood vessels causing necrosis of the bone, which decreases the body’s ability to heal. Areas affected by osteoradionecrosis are extremely susceptible to infection, especially if traumatized.
Neurotoxicity is a side effect of chemotherapy. Neurotoxicity is the ability of a drug or other agent to destroy or damage nervous tissue.12 Within the oral cavity, select classes of chemotherapy, including the plant alkaloids, vincristine, etoposide, and vinblastine, can cause direct neurotoxicity.8 Symptoms can mimic pulpal pain with deep throbbing discomfort that usually affects the mandible and is felt bilaterally.
Chemotherapeutic agents may secondarily reduce platelet formation (thrombocytopenia), which is a common cause of intraoral hemorrhage.8 Hemorrhage can occur anywhere in the mouth either spontaneously or due to trauma or existing disease.8
Oral Care Management Prior to Cancer Treatment
Patients should see a dental professional 2 weeks to 4 weeks before beginning head/neck radiation or chemo therapy. This provides enough time for the mouth to heal after any dental work is completed.6 The examination also provides a basis for future comparison of oral health changes, and assists in the monitoring and treatment of oral complications.8 After the initial oral assessment, the dental practitioner must consult with the managing oncologist to determine the patient’s ability to undergo the anticipated dental treatment.8 Also, it is important to discuss the need for antibiotic prophylaxis before any dental procedures are performed on patients who have a central venous catheter.13
Completing necessary dental work is essential in preventing the patient from requiring invasive procedures during cancer treatment. The goal of the oral care plan is to find and treat oral disease that may produce complications during cancer treatment.6 Oral complications in patients undergoing cancer treatment may be reduced by taking aggressive preventive measures before treatment begins. The oral cavity should be in the best possible condition so it can withstand treatment.1
TABLE 2. ADVERSE ORAL EFFECTS CAUSED BY RADIATION THERAPY.4
- Oral mucositis
- XerostomiA
- Radiation caries
- Dysgeusia (distortion of the sense of taste)
- Infection: bacterial, viral (herpessimplex), and fungal (Candida albicans)
- Trismus (lockjaw)
- Osteoradionecrosis (death of nonvital bone where the radiation therapy is directed)
Pretreatment oral care should include the identification and treatment of low grade and acute oral infections including: caries, broken teeth, retained root tips, endodontic disease, and mucosal lesions. All sources of oral trauma and irritation, such as ill-fitting dentures, orthodontic bands, and other appliances, should be eliminated.13 Due to the increased fragility of oral mucosa, only well-fitting dentures should be worn during radiation treatment and during meals. The prevention of pressure sores beneath partials and full dentures is particularly important.14
The dental hygienist has an important role in providing clinical treatment, as well as in providing information and education. Treatment should include radiographs, periodontal scaling and root planing (if necessary), polishing, and fluoride applications prior to the start of cancer treatment.5 Also, the dental hygienist should emphasize the importance of maintaining oral health throughout the continuum of treatment.5
Patients receiving radiation therapy are at a significant risk of xerostomia, demineralization, and radiation caries. Patients must begin a home regimen of fluoride therapy before beginning cancer treatment. During the initial appointment, impressions should be taken to fabricate custom fluoride trays. Instructions should be provided for the use of the at-home fluoride. Instructions for “basic oral care” should also be provided. Before treatment begins, a recall schedule should be determined. This should be based on the individual’s overall oral health prior to treatment. Ongoing oral health care during treatment will depend on specific needs of the patient (the radiation dose, locations, and the duration of treatment) and the complications that may occur.6 Patients who use tobacco products should be encouraged to refrain from use because they contribute to delayed healing and slow recovery.6
ORAL CARE MANAGEMENT DURING CANCER TREATMENT
The managing oncologist must be consulted before any dental clinical procedures are implemented during chemotherapy.4 Blood work, ordered by the managing oncologist, should be obtained 24 hours before oral surgery or other invasive procedures (such as periodontal scaling/root planing).4 During chemotherapy, the patient is more susceptible to infection due to a reduction in the number of white blood cells.6 Neutrophils are essential for the phagocytosis of bacteria and for the stimulation of the immune system.8 A low neutrophil count is a common adverse drug effect of cancer chemotherapy.8 Treatment should be postponed if the platelet count is less than 50,000/mm and/or if the neutrophil count is less than 1,000/mm.4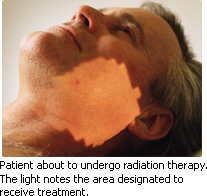
Good oral hygiene is paramount to preventing oral mucositis.9 The Multinational Association of Supportive Care in Cancer (MASCC) and National Comprehensive Cancer Network (NCCN) guidelines recommend “basic oral care” as a standard practice to prevent infections and potentially help alleviate mucosal symptoms.15,16 During treatment, patients should be instructed to remove biofilm daily by gently brushing teeth, gingiva, and tongue with an extra soft toothbrush and fluoride toothpaste after every meal and at bedtime. Teeth should be flossed gently but thoroughly each day.4 Mouthrinsing should be performed every 2 hours to 3 hours while awake, with a baking soda, salt, and water solution (½ teaspoon of baking soda and salt dissolved in 1 cup lukewarm water) followed by a plain water rinse. Products containing alcohol, astringents, oils, and antiseptics should be avoided.8 To prevent irritation, hot, spicy, and hard foods should also be avoided.
TABLE 3. ADVERSE ORAL EFFECTS CAUSED BY CHEMOTHERAPY.5
- Oral mucositis
- Xerostomia
- Infections: bacterial, viral, or fungal
- Increased bleeding and hemorrhage: spontaneous or induced
- Neurotoxicity (damage to nervous tissue)
For patients who develop mucositis, treatment is based on cleaning the mouth and relieving the pain. Topical oral agents are the first step in pain management. Topical agents are often combined with a coating agent, such as kaolin with pectin (Kaopectate), magnesium hydroxide, and/or aluminum hydroxide (Milk of Magnesia, Mylanta, etc), in a compounded product referred to as “miracle mix.” These barrier rinses must be compounded by a registered pharmacist as prescribed by a dentist.8 Patients should rinse with this mixture 30 minutes prior to eating. Over-the-counter mouthrinses designed specifically as barriers for oral tissues are also available. A preparation of viscous lidocaine may be effective in soothing painful mucosal tissues.
MASCC/NCCN does not recommend using chlorhexidine to treat established oral mucositis in patients receiving chemotherapy or to prevent oral mucositis in patients with solid tumors of the head and neck who are undergoing radiotherapy.7 Research has not shown chlorhexidine, an antimicrobial, to be effective in reducing the incidence, severity, or resolution of mucositis.7 Hydrogen peroxide is also not recommended because it can actually break down granulation tissue and impede recovery from mucositis.9
Systemic painkillers may provide relief when topical medications are not sufficient. COX-1 inhibitors are contraindicated for patients at risk of hemorrhage. Acetaminophen and opioidreceptor agonists in combination with acetaminophen are the most appropriate systemic analgesics.8
Demineralization and radiation caries are a concern for patients receiving head and neck radiation. During radiation therapy, instructions should be provided for the once a day use of fluoride in custom fabricated trays. An unflavored 1.1% neutral pH sodium fluoride gel or a 0.4% stannous fluoride should be prescribed. If the patient has porcelain crowns or resin restorations, only neutral sodium should be used. Fluoride rinses should be avoided due to the possibility of mucosal irritation. The trays should cover all the tooth surfaces and be left in the mouth for 5 minutes.4 Special attention should be taken so the gel does not lie on the gingival tissue or mucosa tissue. The patient should be instructed to avoid eating or drinking for 30 minutes.4 If unable to tolerate the trays, the patient should be advised to brush the fluoride gel on the teeth.4 This regimen should begin several days before radiation treatment is scheduled to begin.
To help soothe the symptoms of xerostomia, the patient should be advised to suck on ice chips and sugar-free candy, sip water frequently, use water-soluble moisturizing jellies, chew gum with xylitol, and use saliva substitutes.6 Patients can also incorporate soups into their diet and sip liquids while eating to ensure sufficient moisture. Patients should be warned about the risk of difficulty swallowing and choking due to the lack of saliva.
Amifostine (Ethyol®) is a systemic therapeutic agent used for the prevention of xerostomia during head and neck radiation. It is administered through an intravenous infusion 15 minutes to 30 minutes prior to radiation therapy. Its use may reduce moderate to severe xerostomia.
For patients who present with oral pain during chemotherapy, a thorough medical history and oral physical examination should be performed, including radiographs and vitality testing of the dental pulp.8 After neurotoxicity is appropriately diagnosed, management includes pain support and patient counseling. The symptoms generally resolve within a week following cessation of the causative chemotherapy.8
To prevent intraoral hemorrhage during chemotherapy, any sharp restorations or teeth should be repaired.8 Orthodontic bands and appliances should be removed and the wearing of prosthetics should be limited. The oral mucosa must be kept moistened with saline rinses to avoid hemorrhagic complications.8 If hemorrhage does occur, patients should be advised to soak a disposable oral swab, piece of gauze, or cotton swab in an antimicrobial agent and apply to the site.8
ORAL CARE MANAGEMENT POST-CANCER TREATMENT
Once treatment has been completed, the patient should continue to be monitored. When chemotherapy has ended and all side effects, including immunosuppression, have resolved, the patient can be placed on a personalized dental maintenance schedule.5
Because the effects of radiation therapy are long term, additional care should be provided following the completion of treatment. For the first 6 months after radiation treatment, the recall interval should be every 4 weeks to 8 weeks.4
If the patient has had mucositis, once it subsides, the managing oncologist should be consulted before dentures or other appliances are fabricated.5 If the patient has chronic xerostomia, it may be difficult, if not impossible for the patient to resume wearing appliances. The patient should be continually assessed for signs of trismus, demineralization, and caries. Daily applications of prescription fluoride (either gel or mouthrinse) are needed for patients with chronic xerostomia.5
CONCLUSION
Dental hygienists play an important role in the health of patients before, during, and after they are treated with chemotherapy and/or head and neck radiation. Implementing a dental care plan before cancer treatment begins is crucial to preventing unexpected delays and setbacks in treatment and recovery.
REFERENCES
- National Cancer Institute. Surveillance Epidemiology and End Results. Available at: www.seer.cancer.gov. Accessed August 23, 2010.
- Head and neck cancer. Available at: www. radiologyinfo.org. Accessed August 23, 2010.
- Oral Cancer Foundation. Treatment. Available at: http://oralcancerfoundation.org/treatment/index.htm. Accessed September 1, 2010.
- Wilkins EM. Clinical Practice of the Dental Hygienist. 10th ed. Philadelphia: Lippincott Williams & Wilkins; 2009:862-867.
- Dodd MJ. The pathogenesis and characteri za – tion of oral mucositis associated with cancer therapy. Oncol Nurs Forum. 2004; 31 (4 Suppl): 5-11.
- National Cancer Institute. Head and neck cancer. Available at: www.cancer.gov/cancertopics/types/head-and-neck. Accessed August 23, 2010.
- Rubenstein EB, Peterson DE, Schubert M, et al. Clinical practice guidelines for prevention and treatment of cancer therapy induced oral and gastrointestinal mucositis. Cancer. 2004;100(9 Suppl):2026-2046.
- Duncan M, Grant G. Oral and intestinal mucositis—causes and possible treatments. Aliment Pharmacol Ther. 2003;18:853-874.
- Spijkervet FK, van Saene HK, van Saene JJ, Panders AK, Vermey A, Mehta DM. Mucositis prevention by selective elimination of oral flora in irradiated head and neck cancer patients. J Oral Pathol Med. 1990;19:486-469.
- Cancer Treatment and Oral Health. Available at: www.nidcr.nih.gov/OralHealth/Topics/CancerTreatment. Accessed August 23, 2010.
- Rahn AO, Matalon V, Drane JB. Prosthetic evaluation of patients who have received irradiation to the head and neck regions. J Prosthet Dent. 1968;19:174-179.
- ‘McGettigan S, Stricker Tompkins C. Managing mucositis in head and neck cancer patients undergoing radiation therapy. Community Oncology. 2006;3:653-656.
- Keefe DM, Schubert MM, Elting LS, et al. Updated clinical practice guidelines for the prevention and treatment of mucositis. Cancer. 2007;109:820-831.
- Sonis ST, Elting LS, Keefe D, et al. Perspectives on cancer therapy induced mucosal injury: pathogenesis, measurement, epidemiology, and consequences for patients. Cancer. 2004;100:1995-2025.
- Pickett FA, Terezhalmy GT. Basic Principles of Pharmacology with Dental Hygiene Applications. 1st ed. Philadelphia: Lippincott Williams & Wilkins: 2009:278-288.
- Worthington HV, Clarson JE, Eden OB. Interventions for preventing oral mucositis for patients with cancer receiving treatment. Cochrane Database Syst Rev. 2007;4:CD000978.
From Dimensions of Dental Hygiene. September 2010; 8(9): 66-69.



