Addressing Adverse Drug Effects
The common indirect oral effects caused by drugs and the appropriate treatment modifications necessary to ensure the safe treatment of patients in the dental office.
Reviewing a patient’s drug history is vital to determining potential oral and physiologic effects. Not only are the primary drug effects noted, but medication side effects are as well, which could influence the oral care management plan. The clinical manifestations of adverse drug effects may reflect primary (planned) side effects, ie, what the drug is supposed to accomplish, or secondary (indirect) side effects, which include xerostomia, candidiasis, increased bleeding, and gingival hyperplasia. One serious secondary effect strongly associated with bisphosphonate medications is osteonecrosis of the jaw.1 Physiologic drug effects that can influence oral care include postural hypotension, blood pressure or pulse alterations, blood dyscrasia, and gastrointestinal (GI) changes. These effects can develop from either pharmacologic products or herbal products. All medications listed in a drug history should be investigated in a drug reference before initiating treatment.2
ADVERSE DRUG EFFECTS
Serious adverse drug effects and medication errors in the United States increased by 2.6 fold from 1998 to 2005,3 most likely due to the increased use of medications and the mistaking of drugs by patients. Secondary (indirect) side effects are classified as Type A or Type B.4 They range from mild to severe and can lead to hospitalization, disability, or death. Type A adverse drug effects are associated with the administration of therapeutic dosages of a drug (rather than high doses), are usually predictable and avoidable, and are responsible for most adverse drug effects.4 Some Type A reactions occur as a result of drug interactions, interactions with food components, or effects caused by physical changes of the disease. Type B adverse drug effects are usually independent of the dose and are rarely predictable or avoidable. These include hypersensitivity reactions; tissue harm from chronic administration of a drug, which might be a factor in bisphosphonate- related osteonecrosis of the jaw (BRONJ); or idiosyncratic responses associated with genetic variations or age-related variables. These reactions are uncommon, but often serious. Type B reactions often affect the liver, hematopoietic system (spleen, bone, and marrow), or the skin and mucosa.4 Most drug effects are minor.5 A thorough oral examination is required to identify oral changes that could be due to medication effects.
XEROSTOMIA
Many drugs can affect salivary glands, resulting in reduced salivary levels. The major classes of drugs capable of inducing xerostomia include anticholinergics, antidepressants, antihypertensives, antipsychotics, diuretics, gastrointestinal (GI) acid reducers, antihistamines, antineoplastics, central nervous system (CNS) stimulants, systemic or inhaled bronchodilators, and some cancer chemotherapeutic agents.4 Dry mouth can cause difficulties in tasting, chewing, swallowing, and speaking.5 When dry mouth is noted in the drug reference, questioning should determine if the patient is aware of the side effects. The answer may be negative, but a clinical examination for signs and symptoms of low salivary flow should be completed because clinical diagnosis is often made following the oral examination. When used as a retractor, the dental mirror may stick to the xerostomic patient’s buccal mucosa. Look for the presence of caries, especially a class V or gumline caries pattern. Characteristic clinical findings include a noticeable lack of wetness on mucosal tissues, thick or “ropey” salivary consistency, absence of saliva pooling in the floor of the mouth, and red, dry and atrophic mucosa and/or fissured tongue.4 Examine the soft tissue mucosa for candidal infection which is associated with chronic xerostomia.
When there is strong suspicion that xerostomia is related to medication and oral disease has developed, the patient’s physician may be consulted to discontinue, reduce the dose, or change any medications that predispose to xerostomia. Patient education regarding over-the-counter drugs, which may be a factor in reduced salivary flow, should be provided. Patients should be advised to maintain hydration during the day, to use a fluoride dentifrice twice daily, and rinse with a 0.05% sodium fluoride rinse each day. When oral manifestation of xerostomia is problematic, products that irritate the mucosa should be avoided, such as alcohol, tobacco, acidic or spicy food, and fruits and vegetables with high acid content.4 When candidiasis has developed, an antifungal agent typically resolves the infection.4 A variety of salivary substitutes are available as well as over-the-counter products designed to ease the symptoms of xerostomia. When chapped lips develop, a lip balm that contains vitamin E may be helpful. When xerostomia is severe, a sialogogue tablet may prove beneficial, such as pilocarpine or cevimeline. Chewing xylitol gum stimulates salivation and may help reduce Streptococcus mutans levels in the mouth.6 When active caries or mucosal infection has developed an accelerated maintenance schedule (every 3 months to 4 months) should be considered.4
Candidiasis
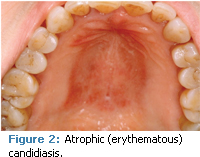
Candidiasis, an infection from Candida albicans, is the most frequently occurring opportunistic fungal infection that infects humans.4 It exists in a commensal state in warm, moist environments, such as oral mucosa. When the body systems are in harmony and the host immune system is at an optimal level, the organism is not a problem. The shift from a state of commensalism to a pathogenic infection is almost always associated with an underlying predisposing factor, including immunosuppression, certain medications, salivary reduction, malignancies, numerous endocrinopathies (eg, diabetes), nutritional deficiencies, and smoking.4 Oral candidiasis can manifest a variety of clinical presentations, including pseudomembranous (Figure 1), atrophic or erythematous (Figure 2), or hyperplastic lesions (Figure 3). Median rhomboid glossitis and some cases of angular chelitis are related to candidal infection.7
Essential to any management strategy is a thorough review of the medical and dental histories to identify predisposing factors because conditions that involve immunosuppression are a major factor in candidiasis. Short term antibiotic use can also be a factor in the etiology. In this case, it is a secondary effect of the primary antimicrobial drug effect. In all cases, the goal of therapy is to remove predisposing factors when possible and to prevent recurrence and nonresponse to pharmacologic therapy. Topical antifungal agents, such as nystatin, clotrimazole, or ketoconazole, are usually effective for mild localized lesions. Nystatin is supplied as a rinse and a pastille. The rinse is swished for 5 minutes five times each day and swallowed or expectorated. Swallowing the product does not kill candida microorganisms in the GI tract as the length of time needed for antimicrobial/microorganism contact is not possible. Since nystatin is not absorbed by the GI tract, it passes through the intestines and is excreted in feces. The pastille is allowed to slowly dissolve in the mouth, fluids swallowed, and is used four to five times per day. Therapy may take up to 4 weeks for lesions to resolve.4 The pastille is not to be chewed or swallowed whole. The doseform for clotrimazole is a troche (lozenge). The troche is dissolved slowly in the mouth five times/day for 14 days. Saliva should be retained (not swallowed), if possible, to increase the contact time with the antifungal agent.4 The troche should not be chewed or swallowed whole. Doseforms for ketoconazole include a 200 mg tablet taken once daily (up to 400 mg) and a 2% cream, which is to be applied to the affected area once daily for 2 weeks to 4 weeks.4,8
INCREASED BLEEDING
A variety of drugs and herbs may be factors in increased gingival bleeding. Antithrombolytic agents, such as aspirin and clopidogrel (Plavix), alter the ability of platelets to stick or clump together and form a clot. This primary effect of these agents can lead to increased bleeding in association with invasive procedures, such as periodontal debridement. A different anticoagulant drug, warfarin (Coumadin), leads to bleeding due to a different mechanism of action. Warfarin reduces clot formation by inhibiting the formation of vitamin-K dependent clotting factors.4 Another anticoagulant drug—heparin—is parenterally administered and is commonly used short term following a total joint replacement procedure. The most common side effect of both warfarin and heparin is hemorrhage, which may present as gingival bleeding or submucosal bleeding with hematoma formation. Common herbs that are associated with increased bleeding include anise, capsicum, chamomile, clove, cranberry, feverfew, garlic, ginger, ginko biloba, ginseng, and saw palmetto.8 Vitamin E is also associated with increased bleeding.8
When antiplatelet drugs (aspirin, clopidogrel) are reported and increased bleeding develops, digital pressure often induces clot formation. When this is unsuccessful, hemostatic agents can be used, such as oxidized cellulose (Surgicel), topical thrombin, or absorbable gelatin sponge (Gelfoam). When anticoagulant agents are reported in the drug history, the clinician should secure the results of the most recent International Normalized Ratio (INR) laboratory test. Individuals who take anticoagulants must take this test each month to determine the level of efficacy. The acceptable range is 2 to 3, but it has been determined that periodontal debridement is safe when the INR is 3.5 or less.4 Individuals with cardiac valve replacements are kept at a 3.5 INR level. When INR level is ?3.5, treatment should be delayed until values are adjusted downward.
GINGIVAL HYPERPLASIA (GH)
Hyperplasia of the gingival connective tissue is associated with three main drugs: phenytoin used to control epilepsy, some calcium channel blocking drugs used to manage cardiovascular disease, and cyclosporine, an immunosuppressant often taken to prevent transplanted organ rejection.7 The mechanism responsible for the development of drug-induced GH is unknown. Whatever the mechanism, poor oral hygiene plays a role because it speeds the condition’s rate of development.9
Effective removal of bacterial plaque may decrease the rate of gingival enlargement, although this practice does not prevent the condition from occurring.9 The dental professional may contact the drug prescriber to determine if another drug less likely to cause GH and with equivalent therapeutic action could be substituted. All strategies for effective plaque control should be recommended and a more frequent maintenance care appointment schedule may slow the rate of enlargement.
BRONJ
Much has been hypothesized regarding the role of bisphosphonate drugs as a causative factor in BRONJ. This class of drugs is used to reduce bone mineral changes associated with cancer chemotherapy and to increase bone mineral density in cases of osteoporosis. The American Association of Oral and Maxillofacial Surgeons (AAOMS)10 states that the intravenous (IV) administered bisphosphonates (zoledronic acid, pamidronate) most likely play a causative role in the condition; there is less evidence for causation with oral doseforms (alendronate, risedronate, ibandronate). More research must be completed to determine the mechanism for osteonecrosis as a causative factor. AAOMS has defined the condition as exposed bone that fails to develop a mucosal coverage with the following additional features: patient has taken a bisphosphonate drug; has not been exposed to head and neck radiation; and exposed bone has been present for more than 8 weeks. Preventive factors are unknown but since most cases developed following invasive oral procedures, maintaining oral health is possibly a preventive goal.11 The American Dental Association (ADA) recommends11 conducting an oral examination prior to initiating bisphosphonate therapy. Some cases developed under dentures or over large tori, which emphasizes the importance of ensuring a proper denture fit when bisphosphonates have been taken or are planned.
The management recommendations include education that informs the patient of the need to maintain excellent oral health and have regular oral exams when bisphosphonates are received. Before oral procedures are implemented the patient should be informed of the rare possibility of developing BRONJ following the oral procedure and asked to sign a consent form giving permission for any oral care. Individuals who have taken oral doseforms of bisphosphonates can receive oral care and there is no restriction for oral procedures.10 However, BRONJ is a newly discovered adverse effect related to bisphosphonate use and a small percentage of cases have been linked to oral bisphosphonates. The clinician needs to keep abreast of current research as recommendations may change based on evidence.
POSTURAL HYPOTENSION
Drugs can affect physiologic systems and can be related to systemic effects, such as blood pressure changes or gastrointestinal effects. Many antihypertensive agents are associated with postural hypotension.12 When a patient is in a supine position, the heart does not have to work as hard to get oxygenated blood to the brain. The body adapts to this change by dilating blood vessels, leading to a drop in blood pressure. When a patient changes to an upright position, the body adapts to this new position by constricting blood vessels leading to an increase in blood pressure. Postural hypotension can develop if the patient is unable to adapt to this change in blood pressure quickly enough. When drugs that lead to hypotension are taken, it is not unusual for blood pressure to drop even more when the patient is moved from the supine position to an upright position.2 Symptoms range from light-headedness, pallor, dizziness, blurred vision, and nausea to loss of consciousness. Clinical criteria include a standing pulse rate that increases at least 30 beats per minute; standing systolic blood pressure that decreases at least 25 mm Hg; and a standing diastolic blood pressure that decreases at least 10 mm Hg.13
In order to minimize this effect, raise the back of the dental chair slowly. Have the patient sit in the upright position for a few minutes before standing. All signs of postural hypotension must be resolved before the patient assumes the full upright position. As a precaution, the blood pressure should be checked and compared with the baseline blood pressure before allowing the patient to stand.
BLOOD DYSCRASIA
Blood dyscrasias, such as thrombocytopenia (reduced number of platelets), leukopenia (reduced number of white blood cells), agranulocytosis (reduction in polymorphonuclear leukocytes), and neutropenia (reduction in neutrophils), are rare side effects listed with a variety of drugs. They occur because they inhibit bone marrow function or as a result of hypersensitivity reaction to a drug.2 Methemoglobinemia is a rare and uncommon adverse reaction usually with high doses of prilocaine, but it may also occur with articaine and topical benzocaine.14
Leukopenia, agranulocytosis, and neutropenia reduce the number of cells that play a role in the host immune response. Consequently, this can lead to an increase in infection and a reduction in healing. Treating patients with dental infections can be a challenge when blood dyscrasia reduces the host response to infection. Oral procedures that could result in the creation of a wound should not be attempted.2 Methemoglobinemia should not develop in a healthy ambulatory dental patient, provided doses of local anesthetic remain within recommended levels.15 In individuals with a history of the condition, an alternate local anesthetic should be selected. Blood dyscrasia adverse drug effects are uncommon.
GI CHANGES
GI effects such as nausea, vomiting, abdominal pain, diarrhea, and constipation are common adverse drug effects. Digoxin may cause nausea, vomiting, diarrhea, and abdominal pain.16 Aspirin and nonsteroidal anti-inflammatory agents (ibuprofen) may cause nausea and vomiting. Analgesic doses of narcotics often produce nausea and vomiting. The opioids also increase the smooth muscle tone of the GI tract and, therefore, decrease both propulsion and motility. This effect makes opioids useful in the treatment of diarrhea.17 All anti-infective drugs can produce a variety of GI complaints.17 The degree of the effects depends on what drug was taken, the dose, and whether or not the drug should be taken with food. Erythromycin has the highest incidence of GI complaints of any of the antibiotics.17 When GI symptoms are reported, a semi-supine position may be suggested.4
The clinician must investigate all prescribed and over-the-counter medications in a dental drug reference before initiating oral care. The adverse drug effects identified will help the clinician determine what, if any, treatment modifications need to be considered and provide guidance regarding appropriate oral hygiene home care instructions.
REFERENCES
- Woo SB, Hellstein JW, Kalmar JR. Systematic review: bisphosphonates and osteonecrosis of the jaws. Ann Intern Med. 2006;144:753.
- Pickett FA, Gurenlian JR. Use of the medical history. In: Preventing Medical Emergencies. 2nd ed. Wolters Kluwer LWW: Baltimore, 2009:48,51,54.
- Moore TJ, Cohen MR, Furberg CDE. Serious adverse drug events reported to the Food and Drug Administration, 1998-2005. Arch Intern Med. 2007;167:1752-1759.
- Pickett FA, Terezhalmy GT. Basic Principles of Pharmacology with Dental Hygiene Applications. WoltersKluwerLWW: Baltimore, 2009:50, 58, 163-164, 57.
- United States Department of Health and Human Services. National Institutes of Health. Dry Mouth. NIH Publication 08-3174. March 2008.
- Ly KA, Milgrom P, Roberts MC, Yamaguchi DK, Rothen M, Mueller G. Linear response of mutans streptococci to increasing frequency of xylitol chewing gum use. A randomized controlled trial. BMC Oral Health. 2006;6:6.
- DeLong L, Burkhart NW. General and Oral Pathology for the Dental Hygienist. Baltimore: Lippincott, Williams & Wilkins; 2008:330, 398, 533.
- Pickett FA, Terezhalmy GT. Lippincott, Williams & Wilkins’ Dental Drug Reference with Clinical Implications. 2nd ed. Baltimore: Lippincott, Williams & Wilkins; 2009:492- 784.
- Philstrom B. Prevention and treatment of dilantin-associated gingival enlargement. Compendium. 1990;14(Suppl):5506-5510.
- Ruggiero SL, Dodson TB, Assael LA et al. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaw—2009 update. J Oral Maxillofac Surg. 2009;67(Suppl):2S-12S.
- Council on Scientific Affairs. American Dental Association. Dental management of patients receiving oral bisphosphonate therapy—expert panel recommendations. 2008. Available at: www.ada.org/prof/resources/topics/topics_osteonecrosis_bisphosphonate_report.pdf. Accessed December 18, 2009.
- Little JW, Falace DA, Miller CS, Rhodus NL, Falace D. Dental Management of the Medically Compromised Patient. 6th ed. Mosby: St. Louis; 2002:71.
- Malamed SF. Medical Emergencies in the Dental Office. 6th ed. Mosby: St. Louis; 2007:151.
- Weinburg MA, Westphal C, Fine JB. Oral Pharmacology for the Dental Hygienist. Pearson Upper Saddle River, NJ: Prentice Hall; 2008:161.
- Malamed SF. Handbook of Local Anesthesia. 5th ed. St.Louis: Elsevier Mosby; 2004:156.
- Wynn RL, Meiller TF, Crossley HL. Drug Information Handbook for Dentistry. 15th ed. Hudson, Ohio: LexiComp; 2009-2010:537.
- Haveles EB. Applied Pharmacology for the Dental Hygienist. 5th ed. St. Louis: Mosby Elsevier; 2007:108,128.
From Dimensions of Dental Hygiene. January 2010; 8(1): 38, 40-42.

