
A New Approach
The implementation of remedial maintenance instrumentation may help clinicians improve periodontal therapy outcomes.
The protocol for treating periodontal maintenance patients who have completed initial therapy but still have bleeding points is not well established. Many practices use controlled-release local delivery antimicrobials/antibiotics in addressing bleeding on probing in this patient population. Chlorhexidine wafers, doxycycline biosorbable gel, and minocycline microspheres can be effective in reversing inflammation. When calculus is left behind, however, localized bleeding on probing (bleeding points) will still emerge because the low-grade infection persists.1
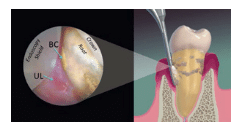
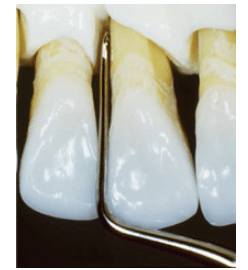
This type of relapse is often attributed to patients’ poor oral self-care, but even those who practice optimal oral hygiene can present with inflammation. The source of this problem is the partially scaled, burnished calculus that remains on the root surface. The pathogenic biofilm within the surface of the burnished calculus prohibits the resolution of the infection (Figure 1).1,2 While the superficial organisms responsible for initiating inflammation are easily dislodged, the indelible scaffold of calculus and biofilm that keeps the pathogens in contact with soft tissues is difficult to remove. As long as there is a speck of residual calculus left behind on the root surface, an ulcerated lesion—matching the size and shape of the deposit—will form in the soft tissue overlying it, and inflammation will continue.5–7 This is clearly demonstrated when periodontal pockets are viewed with the dental endoscope (Figure 2).
Initial instrumentation is aimed at removing mineralized root accretions that harbor Gram-negative pathogens.8 While studies show that the complete removal of calculus is unlikely—especially in pockets greater than 5 mm9,10—it still remains the goal of nonsurgical periodontal therapy.
EVALUATING EFFICACY
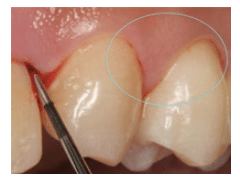
Dental hygienists must continually assess the effectiveness of treatment by objectively examining its outcomes and addressing its limitations. Noting the presence of bleeding points is one way to evaluate the status of a periodontal pocket in a nonsmoking patient. The goal is to eliminate these points. Bleeding often will present after probe insertion as a minute pinpoint or hairline trickle along the gingival margin of a maintenance patient (Figure 3).11 Highlight these areas on a quick reference chart (Figure 4), so they can be referred to throughout the maintenance appointment.
Prior instrumentation can make subgingival deposits difficult to detect. This is especially true when inadequate power is used during ultrasonic scaling. Calculus is rapidly smoothed down to a sheet or veneer.1 The residual burnished calculus mimics the texture of cementum, leading the clinician to assume the deposit has been completely removed. Therefore, tactile assessment is not a reliable indicator of the presence of calculus; instead, bleeding points should guide the approach. They will also provide evidence of success at the next periodontal assessment.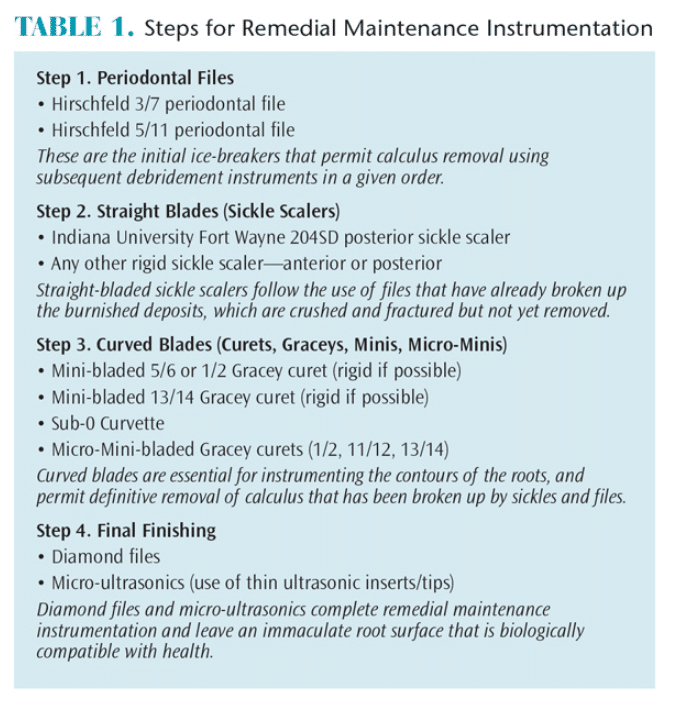
REMEDIAL MAINTENANCE INSTRUMENTATION
Once subgingival calculus becomes burnished onto the root surface, removal is difficult.1 Remedial maintenance instrumentation (RMI), explained in Table 1, is a new approach that may provide better results.
Instruments for RMI are listed in order of their sequence for use. Hirschfeld files, which have a series of tiny parallel blades positioned along a straight terminal shank, are mandatory. These files can bite into burnished calculus, effectively crushing and fracturing subgingival deposits that are otherwise impossible to remove.12
One of the benefits of the Hirschfeld file is its compact head that can easily slip under the tight or fibrotic tissues often seen in maintenance patients. A narrow width and depth at the head permit access to the base of deep, narrow pockets. An example of such an area is periodontal pathology overlying longitudinal root grooves.13
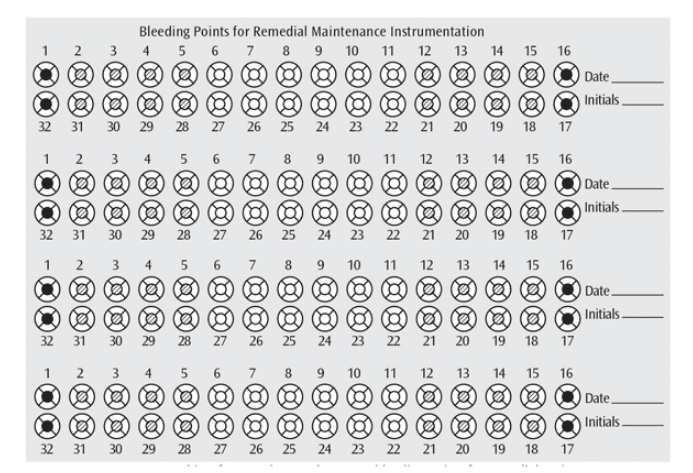
FIGURE 4 © PACIFIC NW INSTITUTE
To activate Hirschfeld files, a simple pull stroke that runs parallel to the terminal shank of the instrument is used. The stroke is always a straight vector that is perpendicular to the individual blades. Strokes may be horizontal, vertical, or oblique, according to the position of the instrument (Figure 5).
Sickle scalers, both anterior and posterior, follow the use of periodontal files. The Indiana University Fort Wayne 204SD is a large posterior sickle scaler (IUFW-204SD) with a rigid shank to maximize torque for removing burnished calculus.
Curets have curved blades that conform to root contours and are essential for definitive subgingival debridement. Mini-bladed and Micro-Mini-bladed Graceys offer the conformation and torque needed for the tight root contours of deep pockets and furcations, but they work equally well in shallow pockets—particularly at the cementoenamel junction. Anterior Curvettes, such as the Sub-0, with shorter, curved blades that resemble crochet hooks, are effective for the small-radius curvatures of lower anterior roots.14
Diamond files can be effective in root concavities and/or furcations that do not permit access to larger instruments. Position and activate diamond-coated instruments in any direction, but use only very light pressure to prevent excess removal of root structure. Ultrasonic instrumentation at medium-low power is the final step to flush out any remaining contaminants.
These four steps provide a winning formula for definitive debridement in the most challenging of circumstances—burnished subgingival calculus. The proof will be seen in subsequent bleeding point assessment and, more important, the long-term stabilization of the periodontium.
Complete calculus removal is usually never attained at the end of initial periodontal scaling and root planing. If periodontal referral and surgery are not possible, multiple continuing care appointments using this method of remedial maintenance instrumentation every 3 months to 4 months may be necessary to achieve the ultimate goal of zero bleeding points.
REFERENCES
- Stach D. Back to basics. Dimensions of Dental Hygiene. 2007;5(4):26–29.
- Sbordone L, Ramaglia L, Gulletta E, Iacono V. Recolonization of the subgingival microflora after scaling and root planing in human periodontitis. J Periodontol. 1990;61:579–584.
- Matsuda S. Instrumentation of biofilm. Dimensions of Dental Hygiene. 2003;1(1):26–30.
- Rabbani GM, Ash MM Jr, Caffesse RG. The effectiveness of subgingival scaling and root planing in calculus removal. J Periodontol. 1981;52:119–123.
- Checchi L, Montevecchi M, Checchi V, Zappulla F. The relationship between bleeding on probing and subgingival deposits. An endoscopical evaluation. Open Dent J. 2009;28:154–160.
- Stambaugh RV.A clinician’s 3-year experience with perioscopy. Compend Contin Educ Dent. 2002;23:1061–1070.
- Pattison AM, Pattison GL. Periodontal instrumentation transformed. Dimensions of Dental Hygiene. 2003;1(2):18–22.
- Drisko CL, Killoy WJ. Scaling and root planing: removal of calculus and subgingival organisms. Curr Opin Dent. 1991;1:74–80.
- Stambaugh RV, Dragoo M, Smith DM, Carasali L. The limits of subgingival scaling. Int J Periodontics Restorative Dent. 1981;1:30–41.
- Rabbani GM, Ash MM Jr, Caffesse RG. The effectiveness of subgingival scaling and root planing in calculus removal. J Periodontol. 1981;52(3):119–123.
- Sherman PR, Hutchens LH Jr, Jewson LG, et al. The effectiveness of subgingival scaling and root planing. I. Clinical detection of residual calculus. J Periodontol. 1990;61:3–8.
- Hodges K. Using files in periodontal therapy. Dimensions of Dental Hygiene. 2004;2(11):16–20.
- Brayer WK, Mellonig JT, Dunlap RM, et al. Scaling and root planing effectiveness: the effect of root surface access and operator experience. J Periodontol. 1989;60:67–72.
- Hodges K. Revisiting instrumentation in anterior segments. Dimensions of Dental Hygiene. 2007;5(2):30–33.
From Dimensions of Dental Hygiene. February 2015;13(2):34,36,38.

