9 Myths About Caries Prevention in Older Adults
New research discredits the traditional emphasis on restorative care for older patients—paving the way for more effective prevention strategies.
This course was published in the January 2012 issue and expires January 2015. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the risk of caries among older adults.
- Detail the best strategies for preventing and treating caries in older adults.
- Identify the role of the dental hygienist in reducing tooth decay among this patient population.
During the aging process, general health and well-being must be maintained in order to optimize quality of life. Looking and feeling good are important parts of health. When oral health is compromised, quality of life can suffer. Oral health includes the ability to eat, speak, and socialize properly without pain, discomfort, or embarrassment. New research shows that caries can be prevented and effectively cured—debunking the traditional emphasis on restorative care.1 This change in thinking challenges previous protocols used in caries treatment. Let’s shed some light on nine common myths about caries prevention in older adults.
Myth #1
The first myth is that children are at the greatest risk of tooth decay. Dental caries is the most common chronic disease of childhood,2,3 but older adults are at greater risk than children. Caries remains the most prevalent disease among older adults—affecting 93% of those age 65 or older.4,5 Data show that adults in this age range have more caries than children younger than 14 who reside in areas without community water fluoridation.6 The high caries rate among older adults is due to their increased risk factors, including a higher rate of xerostomia due to medication use; heavy intake of sugar/carbohydrates; and the presence of restored teeth, recession, and fixed or removal partial dentures. They may have difficulty adequately performing their selfcare routines because of disability or diminished dexterity.6–10
Myth #2
The widely held belief that carious lesions develop most often on the occlusal surfaces of teeth among older adults is another misconception. According to the National Institute for Dental and Craniofacial Research, 49.7% of people aged 75 or older have root caries affecting at least one tooth.4 As patients grow older, gingival margins often recede and root surfaces are exposed—making them more susceptible to root caries. Although anyone with gingival recession can develop root caries, older adults are usually more vulnerable because of systemic medical conditions or medications that contribute to xerostomia.11
Dietary habits, microbial plaque, and a decreased salivary flow all affect the risk of root caries.11 Even mild xerostomia can induce a more sticky, thick plaque that is difficult to remove. Plaque biofilm tends to accumulate at the gingival margin and on root surfaces, and brushing with a manual toothbrush may be inadequate at plaque disruption and removal. Risk reduction therapies and self-care education should include recommending a power toothbrush, instruction on proper brushing technique at the gingival margin, and diet assessment and instruction.
Myth #3
Another misconception is that brushing and flossing are the best ways to reduce the risk of caries among older adults. Before the caries management by risk assessment (CAMBRA) protocol was introduced in 2007,12 dental professionals recommended brushing and flossing as the primary tools in caries management and prevention—mainly because caries is caused by certain bacteria (Streptococcus mutans and Lactobacillus, Figure 1). The theory was that because brushing and flossing reduce bacteria levels in the oral cavity, they would also decrease the risk of caries. An adequate self-care regimen is important, but it is only one of the many strategies needed to reduce caries risk.
Flossing is also not the most effective form of daily plaque disruption for this population because it is effective only if the proper type of floss and technique are used. In addition, flossing simply may not be possible for those who have impaired dexterity or reduced mental capacity. Additionally, xerostomia causes thick, sticky plaque that is not easily removed with floss. If large embrasures are present or concave root surfaces are exposed, floss cannot properly adapt to the surfaces to effectively remove plaque or food debris. Floss holders may be used, but specific instructions are needed in order to ensure their proper subgingival use. Older adults should be provided with floss alternatives—such as rubber tip stimulators, interdental brushes, water irrigators, and power flossers—which can help provide supragingival and subgingival plaque disruption.13–18
Myth #4
The fourth myth is that daily brushing of removable partials or dentures is enough to keep caries at bay. In reality, removable dental appliances should be cleaned after brushing using a denture cleaner that carries the American Dental Association (ADA) Seal of Acceptance. The tongue and tissue located under appliances must also be brushed. Older adults are often unaware of the need for these additional steps—leaving them at increased risk of caries and bacterial pneumonia. Bacterial pneumonia is the second most common hospital-acquired infection in the US—accounting for 18% of all infections and between 40,000 deaths and 70,000 deaths each year.19 Oral hygiene intervention may prevent pneumonia in vulnerable patients (Table 1).20–22
![]() Myth #5
Myth #5
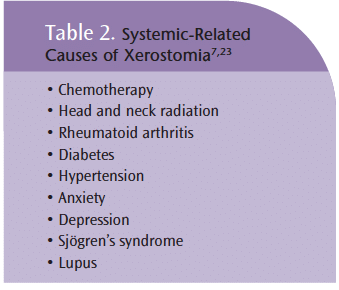
The belief that xerostomia risk can be determined by asking patients if they are experiencing a reduction in salivary flow may be one of the most dangerous myths. Xerostomia is a significant risk factor for caries because it creates an oral environment that is highly acidic.6,8–10 Saliva provides a natural protective mechanism against caries because it provides an environment rich in acid-buffering agents and calcium and phosphate (needed to reduce demineralization of enamel). Without the proper amounts of saliva, there is an enhanced risk of demineralization.1,6,8–10
The oral cavity does not naturally acquire dryness as the body ages.7 Xerostomia can be related to many diseases, disorders, and medications (Table 2).6,8,23 Medication use, however, is the most common cause. More than 400 medications (over-the-counter and prescription) list xerostomia as a side effect.6 Antihypertensives, antidepressants, analgesics, diuretics, decongestants, and antihistamines are common examples of medications that can induce varying levels of xerostomia. Patients’ medication regimens often change between dental hygiene visits, so health histories and medications must be updated at every opportunity.6
The experience of “dry mouth” is not an effective diagnostic factor for this condition. People are often unaware of dryness in their mouths. The question “Have you noticed any dryness in your mouth recently?” is frequently answered with a firm no. Xerostomia status needs to be determined by an intraoral exam, evaluation of all medications the patient is taking, and a health history review. Saliva flow testing is an option, but it can be time consuming and expensive. Dental hygienists have the unique opportunity to evaluate salivary flow during patient treatment. Look for signs of decreased salivary flow, such as bubbly-frothy saliva, stringy saliva, and lack of salivary production during prophylaxis.24,25 Patients presenting with thicker, stickier plaque than at previous appointments may also be a sign of xerostomia. If direct inquiry is warranted, the question should be worded in a specific manner. For example: “Does your mouth ever feel dry at night or when you wake up?” or “Do you have difficulty swallowing dry foods?”26
![]() Myth #6
Myth #6
A common misconception is that reviewing the diets of older adults to ascertain sugar intake is unnecessary. People of all ages who have even a mild case of xerostomia are drawn to sugary substances because they immediately increase salivary flow.26,27 People with xerostomia typically consume hard candies, mints, chewing gum, and cough drops, which may be coupled with sipping on sodas or fruit juices. The dentition is then constantly bathed in sugars—increasing the risk of decay.
Myth #7
Many dental professionals believe that prescribing a 5,000 ppm fluoride dentifrice to seniors will reduce their risk of caries. Fluoride alone, however, cannot remineralize tooth structure in the absence of calcium and phosphate.28,29 Calcium and phosphate are available naturally within saliva. Decreases in salivary quality and quantity affect the naturally-available calcium and phosphate levels needed for remineralization to occur.28,29 In order to enhance the uptake of fluoride, calcium and phosphate are key additions for older adults with xerostomia.28,30–33
Myth #8
Professionally-applied fluoride treatments are only indicated for children is another myth. According to current ADA standards, fluoride varnish is recommended for both children and adults who are at moderate or high risk of caries.34
Myth #9
The final myth is that watching and re-evaluating an early carious lesion at the next recare appointment is the most advantageous strategy. With proper risk assessment and treatment protocols, early carious lesions can be prevented and even reversed. Once diagnosed, an early carious lesion or demineralization should be treated with the current risk reduction protocols recommended by the ADA and CAMBRA research, and then re-evaluated.19,35 Early carious lesions detected radiographically should be monitored by a single bitewing radiograph at the 6-month to 12-month interval.19 The lesion can be evaluated for progression and then restored or continually remineralized. Early carious lesions that are detected clinically should be re-evaluated after 4 weeks of remineralization therapy.35
Bottom Line
All dental professionals have an ethical obligation to reduce the risk of caries among their older adult patients. Dental hygienists, as prevention experts, are at the forefront of this battle. In order to be well prepared, dental hygienists need to stay abreast of the latest research in the area of caries risk assessment and reduction for older adults. Patients’ health histories and medication use must be updated at each appointment. A drug reference book or electronic resource can be used to review medication side effects, including xerostomia.
Electronic drug reference tools accessible from computers or mobile devices are available. Dental hygienists must evaluate risk factors for caries at every appointment. Dietary habits should also be reviewed with an emphasis on sugar/refined carbohydrate intake and frequency. Educate seniors about the use of sugar-free candies, mints, chewing gums, and drinks to address sugar cravings.1,26,27 Alcohol-free mouth rinses should be recommended to reduce dryness in the mouth.35 Recommend the use of chewing gums, candies, and/or mints containing polyols as they stimulate salivary flow naturally.1,35 Xylitol, specifically, may also reduce the levels of S. mutans.35,36 Instruct older adults on how to use power toothbrushes. Provide instruction on brushing not just the teeth but also the gums, because caries is more prevalent at the gingival margins than on occlusal surfaces.
Offer caries risk reduction and remineralization products. Recommend some over-the-counter and professionally-dispensed products containing calcium, phosphate, and fluoride to boost remineralization.1,16,18,23,24 Fluoride varnish is recommended at all recare appointments for patients at moderate to high caries risk. Provide handouts that include personalized instructions and clinician contact information for follow-up questions.
It used to be that people expected to lose their teeth as they aged, but we know now that this is not a predetermined part of growing old. Dental hygienists can help seniors maintain their oral health and prevent the trauma, expense, and reduced quality of life that often accompanies tooth loss.
PHOTO CREDIT: DR. KARI LOUNATMAA/PHOTO RESEARCHERS INC
References
- Young D, Buchanan P, Lubman R, Norton- Badway N. New directions in interorganizational collaboration in dentistry: the CAMBRA coalition model. J Dent Educ. 2007;71:595-600.
- US Department of Health and Human Services. A National Call to Action to Promote Oral Health. Rockville, Md: National Institute of Dental and Craniofacial Research; 2003. Publication 03-5303.
- Kagihara L, Niederhauser V, Stark M. Assessment, management, and prevention of early childhood caries. J Am Acad Nurse Pract. 2009;21:1-10.
- National Institute of Dental and Craniofacial Research. Dental caries in Seniors. Available at: www.nidcr.nih.gov/DataStatistics/FindDataByTopic/DentalCaries/DentalCariesSeniors65older. Accessed December 20, 2011.
- National Institute of Dental and Craniofacial Research. The Magnitude of the Problem. Available from: www.nidcr.nih.gov/Data Statistics/SurgeonGeneral/sgr/chap4.htm. Accessed December 20, 2011.
- Ettinger R. Oral health and the aging population. J Am Dent Assoc. 2007;138:5S-6S.
- Carmona R. Ageism in Healthcare: Are Our Nation’s Seniors Receiving Proper Oral Health Care? Remarks before the Special Committee on Aging United States Senate. Available at: www.surgeongeneral.gov/news/testimony/ageism09222003.htm. Accessed December 20, 2011.
- Turner M, Ship J. Dry mouth and its effects on the oral health of elderly people. J Am Dent Assoc. 2007;138:15S-20S.
- Leal SC, Bittar J, Portugal A, Falcao DP, Faber J, Zanotta P. Medication in elderly people: its influence on salivary pattern, signs and symptoms of dry mouth. Geriodontology. 2010;27:129-133.
- Stookey G. The effect of saliva on dental caries. J Am Dent Assoc. 2008;139(Suppl): 11S-17S.
- Gupta B, Marya CM, Juneja V, Dahiya V. Root caries: an aging problem. The Internet Journal of Dental Science. 2007;5(1).
- Jenson L, Budenz AW, Featherstone JD, Ramos-Gomez FJ, Spolsky VW, Young DA. Clinical protocols for caries management by risk assessment. J Calif Dent Assoc. 2007;35:714-723.
- Yankell SL, Shi S, Emling RC. Efficacy and Safety of BrushPicks, a new cleaning aid, compared to the use of Glide floss. J Clin Dent. 2002;13:125-129.
- Yost KG, Mallatt ME, Liebman J. Interproximal gingivitis and plaque reduction by four inter – dental products. J Clin Dent. 2006;17:79-83.
- Cronin MJ, Dembling WZ, Cugini M, Thompson MC, Warren PR. A 30-day clinical comparison of a novel interdental cleaning device and dental floss in the reduction of plaque and gingivitis. J Clin Dent. 2005;16:33-37.
- Warren PR, Chater BV. An overview of established interdental cleaning methods. J Clin Dent. 1996;7:65-69.
- Eberhard J, Damm S, Freitag S, Albers HK, Jepsen S. Plaque removing capacity of a novel high pressure water irrigator. Am J Dent. 2004;17:199-202.
- Gorur A, Lyle DM, Schaudinn C, Costerton JW. Biofilm removal with a dental water jet. Compend Contin Educ Dent. 2009;30:1:1-6. J Periodontol. 2006;77:1421-1429.
- Iregui MG, Kollef MH. Ventilator-associated pneumonia complicating the acute respiratory distress syndrome. Semin Respir Crit Care Med. 2001;22:317-326.
- Scannapieco F. Pneumonia in nonambulatory patients. J Am Dent Assoc. 2006; 137(Suppl): 21S-25S.
- Scannapieco F. Role of oral bacteria in respiratory infection. J Periodont. 1999; 70: 793-802.
- Limeback H. Implications of oral infections on systemic diseases in the institutionalized elderly with a special focus on pneumonia. Ann Periodont. 2002;3:125-129.
- Scully C, Ettinger RL. The influence of systemic diseases on oral health care in older adults. J Am Dent Assoc. 2007;138:7S-13S.
- Wick JY. Xerostomia: causes and treatment. Consult Pharm. 2007;22:985-992.
- Zunt S. The importance of saliva. Dimensions of Dental Hygiene. 2006;4:28-29.
- Guggenheimer J, Moore P. Xerostomia, etiology, recognition, and treatment. J Am Dent Assoc. 2003;134:61-69.
- Quandt SA, Savoca M, Leng X, et al. Dry mouth and dietary quality in older adults in North Carolina. J Am Geriatr Soc. 2011;59:439-445.
- Featherstone JDB. Remineralization, the natural caries repair process-the need for new approaches. Adv Dent Res. 2009;21:4-7.
- Karlinsey R, Mackey A. Solid-state preparation and dental application of an organically modified calcium phosphate. J Mater Sci. 2008; 44:346-349.
- Tung MS, Eichmiller FC. ACP for tooth mineralization compendium. Cont Educ Dent. 2004;9:9-13.
- Cochrane NJ, Saranathan S, Cai F, Cross KJ, Reynolds EC. Enamel subsurface lesion remineralization with casein phosphopeptide stabilised solution of calcium, phosphate and fluoride. Caries Res. 2008;42:88-97.
- Schemehorn BR, Orban JC, Wood GD, Fischer GM, Winston AE. Remineralization by fluoride enhanced with calcium and phosphate ingredients. J Clin Dent. 1999;10: 13-16.
- Zhang F, Zhu M, She W. A study on the cariogenic bacteria of plaque on abutment teeth of casting and wrought wire clasp removable partial dentures. Zhonghua Kou Qiang Yi Xue Za Ahi. 1999;34:37-39.
- American Dental Association Council on Scientific Affairs. Professionally applied topical fluoride: evidence-based clinical recommendations. J Dent Educ. 2007; 71:393-402.
- Spolsky V, Black B, Jenson L. Products-old, new and emerging. J Calif Dental Assoc. 2007;35:724-737.
- Rothen M. The wonder of xylitol. Dimensions of Dental Hygiene. 2005;3:18-20.
From Dimensions of Dental Hygiene. January 2012; 10(1): 60-63.