 ayo888 / iStock / Getty Images Plus
ayo888 / iStock / Getty Images Plus
All that Implant Therapy Has to Offer
Flapless surgical implant placement is a viable option for many patients.
As implant therapy has grown in popularity and less invasive approaches have emerged, improving our understanding of the current techniques is key. This Perio Update focuses on flapless surgical implant placement.
The term “flapless implant surgery” involves preparing the implant osteotomy and placing the implant without the elevation of a mucoperiosteal flap.1,2 Ledermann pioneered the flapless surgical technique in the late 1970s in an attempt to minimize the bone resorption process associated with implant osseointegration.3
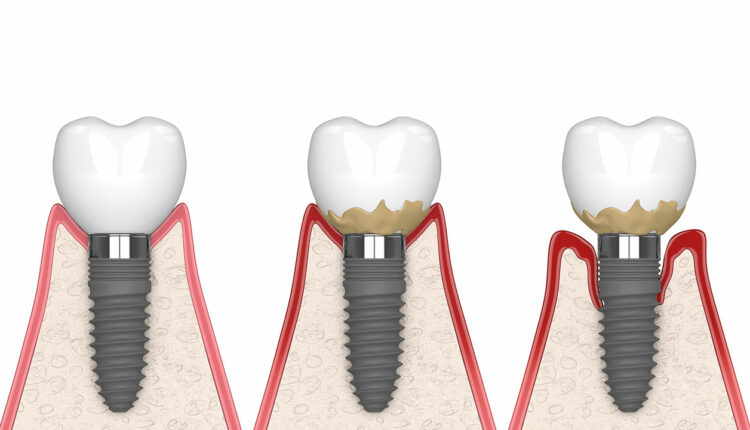
Osseointegration is when living bone is in direct contact with the implant surface, establishing a nonmovable integration between the implant and bone.4,5 The degree of osseointegration is a key determinant of implant success. Additionally, the adaptation of the epithelium to the abutment or implant plays a significant role in its longevity.6
Should the biologic seal be broken, a cascade of tissue and cell injury will result within the internal milieu that supports the implant device, triggering an inflammatory response in the surrounding soft tissues. The underlying hard tissue will then undergo osteoclastic activity, followed by chronic resorption of the supporting bone. As the supporting bone continues to deteriorate, granulation tissue will develop, causing implant failure.6
Primary variables related to different types of surgical procedures, as well as secondary factors associated with the development of marginal bone loss, may impact the long-term clinical performance of dental implant therapy.4 The traditional technique for implant surgery entails flap elevation, which gives direct access to implant sites, improves placement angulation control, and minimizes the risk of bone fenestrations and dehiscence.2
Some studies, however, found that this method resulted in higher or receded soft tissue and bone resorption, post-operative edema, discomfort, and delayed recovery due to increased surgical stress and longer surgical time.7 Maintaining the papillae and gingival contour intact around the implant is critical, particularly with patients whose soft tissue is visible while performing functions such as speaking and smiling.3 By eliminating the need for an incision, there is less chance of interrupting blood flow from the bone membranes or soft tissues, which could otherwise lead to inadequate blood circulation and the necessary nutrients to the recipient site, resulting in poor bone regeneration or osseointegration surrounding the implants.8
The bone receives its blood supply through three distinct pathways: the periodontal ligaments, connective tissue above the periosteum, and the alveolar bone. When a tooth is lost or extracted, the periodontal ligament loses its blood supply, leaving only the soft tissues and bone to supply the necessary blood in the area.3
Compared to bone marrow, cortical bone has few blood vessels flowing through it. When soft tissue is flapped, the available blood from the soft tissue to the bone (supraperiosteal blood supply) is taken, leaving behind an inadequately vascularized cortical bone, which contributes to bone resorption during the initial phase of healing.3
Although few studies have evaluated the crestal bone height between flapless and flap surgical procedures, one study compared the clinical manifestations of marginal bone loss and swelling, patients’ reported pain assessment, and number of analgesics taken between flapless and conventional flap implant insertion. Researchers found that the flapless implant placement resulted in more positive outcomes concerning marginal bone loss, patient pain perception, and number of post-operative analgesics taken. No significant difference was noted in post-operative swelling between the two implant techniques. 3
References
- Naeini EN, Atashkadeh M, De Bruyn H, D’Haese J. Narrative review regarding the applicability, accuracy, and clinical outcome of flapless implant surgery with or without computer guidance. Clin Implant Dent Relat Res. 2020;22:454–467.
- Yadav MK, Verma UP, Parikh H, Dixit M. Minimally invasive transgingival implant therapy: a literature review. Natl J Maxillofac Surg. 2018;9:117–122.
- Divakar TK, Gidean Arularasan S, Baskaran M, et al. Clinical evaluation of placement of implant by flapless technique over conventional flap technique. J Maxillofac Oral Surg. 2020;19:74–84.
- Buser D, Sennerby L, De Bruyn H. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontol 2000. 2017;73:7–21.
- Gehrig JS, Shin DE, Willmann DE. Foundations of Periodontics for the Dental Hygienist. 5th ed. Burlington, Massachusetts: Jones & Bartlett Learning; 2019:165.
- Jayesh RS, Dhinakarsamy V. Osseointegration. J Pharm Bioallied Sci. 2015;7(Suppl 1):S226–S229.
- Cai H, Liang X, Sun DY, Chen JY. Long-term clinical performance of flapless implant surgery compared to the conventional approach with flap elevation: a systematic review and meta-analysis. World J Clin Cases. 2020;8:1087–1103.
- Gao X, Qin S, Cai H, et al. Comparison of general and aesthetic effects between flapless and flap techniques in dental implantation: a meta-analysis of randomized controlled trials. Int J Implant Dent. 2021;7:100.
This information originally appeared in Monchik C, Marsh I. Innovations in implant therapy. Dimensions of Dental Hygiene. 2023;21(3)34-37.

