Indications for CBCT Use
Cone-beam computed tomography has myriad uses in orthodontics.
This course was published in the September 2014 issue and September 30, 2017. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss how cone-beam computed tomography (CBCT) is used in the evaluation of developmental anomalies of tooth structure and impacted teeth.
- Identify how CBCT is used in the identification of dento-alveolar morphologies, dentofacial deformities, and craniofacial anomalies.
- Describe CBCT’s indications for use in malocclusion, skeletal discrepancies, and temporomandibular joint disorders.
- Explain the role of CBCT in post-therapy and airway assessment and oral pathology.
The ability to capture three-dimensional (3D) dental and skeletal relationships is a tremendous benefit in the specialty of orthodontics, and cone-beam computed tomography (CBCT) provides this advantage at a relatively low cost. The diagnostic capabilities of CBCT are far more advanced than traditional two-dimensional (2D), or traditional, radiography. As dental hygienists are leaders in patient education, it is important they understand how CBCT is used in orthodontic treatment. This article will discuss specific indications for CBCT in orthodontics.
DEVELOPMENTAL ANOMALIES IN DENTAL POSITION
CBCT imaging has indications for the assessment and diagnosis of a number of specific conditions in orthodontic patients.1–4 Developmental anomalies of tooth structure can lead to disturbances in maxillary and mandibular dental arch lengths, occlusal arch discrepancies resulting in crowding and poor esthetics, and inter-arch differences producing malocclusions. These anomalies may have local or more generalized effects, producing regional or more widespread disturbances. Developmental anomalies include variations in tooth morphology (eg, fusion, gemination, microdontia, or peg-shaped maxillary and mandibular lateral incisors, macrodontia, dilacerated tooth, and transposed roots); number (eg, oligodontia, hypodontia, or congenitally missing maxillary lateral incisors, mandibular incisors and canines, and maxillary and mandibular premolars, and hyperdontia, or supernumerary teeth, as seen in Figure 1); and structure (eg, internal root resorption or congenital conditions affecting the entire dentition, such as amelogenesis imperfecta).
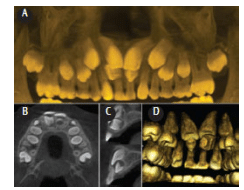
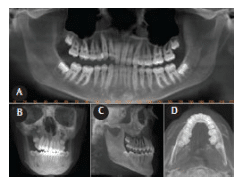
Imaging can play a role in the evaluation of impacted teeth, commonly the mandibular third molars or maxillary canines (Figure 2); the presence of unerupted and impacted supernumerary teeth, like the mesiodens seen in Figure 1; anomalies in dental eruption sequence; and ectopic eruption, including teeth associated with jaw clefts. Visualization of these conditions can assist in decisions, such as whether to remove the tooth, and on surgical approaches and techniques. Important information includes determining the size of the crown of the tooth; localizing the position of the tooth, such as inclination of the long axis of the tooth; relative buccal and palatal positions; the amount of bone covering the tooth; determining the effect on adjacent teeth, such as resorption of the roots of adjacent teeth and the condition of adjacent teeth; identifying local anatomic surgical considerations, such as location of the nasopalatine canal, mental foramen, or inferior alveolar canal; determining the overall stage of dental development; and the assessment of associated pathology.
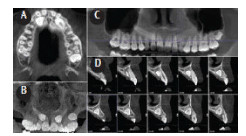 FIGURE 2. The axial (A), frontal maximum intensity projection rendering (B), reformatted panoramic (C), and multiple cross-sectional 1 mm thick sections (D) of the left anterior region show the location, orientation, and position of the severely mesio-angular, palatally positioned, completely bony impacted and unerupted maxillary canines bilaterally.
FIGURE 2. The axial (A), frontal maximum intensity projection rendering (B), reformatted panoramic (C), and multiple cross-sectional 1 mm thick sections (D) of the left anterior region show the location, orientation, and position of the severely mesio-angular, palatally positioned, completely bony impacted and unerupted maxillary canines bilaterally.
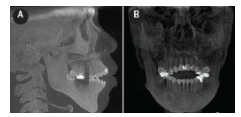
 FIGURE 3. This maximum intensity projection lateral cephalometric image is reformatted from cone-beam computed tomography data. Figure 3A demonstrates an anterior open bite and excessive interincisal angle between the maxillary and mandibular incisors, requiring a change in the position of the anterior mandibular incisors. The axial image (B) shows a very thin alveolar bone width associated with the roots of the mandibular incisor teeth. This restricts the range of orthodontic movement possible for the mandibular anterior incisors without dehiscence or fenestration of the roots through the cortical plate.
FIGURE 3. This maximum intensity projection lateral cephalometric image is reformatted from cone-beam computed tomography data. Figure 3A demonstrates an anterior open bite and excessive interincisal angle between the maxillary and mandibular incisors, requiring a change in the position of the anterior mandibular incisors. The axial image (B) shows a very thin alveolar bone width associated with the roots of the mandibular incisor teeth. This restricts the range of orthodontic movement possible for the mandibular anterior incisors without dehiscence or fenestration of the roots through the cortical plate.
DENTO-ALVEOLAR MORPHOLOGY
The width of the alveolus of the jaws defines anatomic facio-palatal/lingual boundaries for orthodontic torque movement of teeth, or retraction, arch expansion, or labial movement of incisors (Figure 3). Evaluation of fenestrations and dehiscence on the buccal and lingual surfaces can be an important consideration in certain patients, such as those with bimaxillary protrusion, compromised periodontal status, and/or clefts of the alveolus. In addition, determination of dento-alveolar volume is important for patients who are potential candidates for dental implants, bone grafts, or temporary anchorage devices.2,5,6
DENTOFACIAL DEFORMITIES AND CRANIOFACIAL ANOMALIES
Three-dimensional volumetric imaging is a particularly useful tool in the analysis of severe skeletal discrepancies producing facial or mandibular asymmetry (Figure 4), and anteroposterior, vertical, and transverse deficiencies, as well as an assessment of their dental effects.7–13 Appreciation of the complexity of these abnormalities demands visualization of the inter-relationships of the dental, skeletal, and soft tissue elements. CBCT data can be exported to specific software programs that can be used for virtual treatment simulations to plan orthopedic corrections, such as orthognathic surgery or distraction osteogenesis.
MALOCCLUSIONS AND SKELETAL DISCREPANCIES
Identification of Class II and Class III skeletal malocclusions (Figure 5)8,14–16 and increased or decreased vertical facial height and asymmetry,17 either alone or in combination, involves an appreciation of the contribution of maxillary and mandibular anterior-posterior, vertical, and transverse discrepancies that are well-visualized with CBCT images. These anomalies may present clinically as the following: chin or mandibular deviation; dental midline deviation; occlusal cant (tilt) discrepancies; anterior open bite; deep overbite; skeletal lingual or buccal crossbites; or excessive dental compensation of the bucco-lingual inclination of posterior teeth.
TEMPOROMANDIBULAR JOINT
Visualizing the morphology of the temporomandibular joint (TMJ) articulation can be necessary if orthopedic treatment is anticipated that may affect structural development during growth—such as head gear, functional appliances, or if the patient has a history of previous condylar trauma (Figure 6). TMJ pathologies that result in alterations in the size, form, quality, and spatial relationships of the osseous joint components may lead to skeletal and dental discrepancies, such as progressive bite changes, including bite opening and limitation; deviation upon opening or closing; and changes in tooth position, occlusion, and the TMJ of the unaffected side. Such TMJ instabilities can lead to unpredictable orthodontic outcomes.
Affected joints are particularly important to image in patients with diminishing quality of life issues, such as persistent pain or limited opening. TMJ conditions include developmental disorders such as condylar hyperplasia, hypoplasia, or aplasia, and patients with moderate to severe arthritic degeneration. In these situations, CBCT imaging provides additional diagnostic information, such as the size, shape, and position of mandibular condyle heads in established positions and the presence of active disease that may influence management.
POST-THERAPY AND AIRWAY ASSESSMENT
CBCT may be useful in assessing the treatment outcomes of orthognathic surgery, grafting procedures, and the use of nonsurgical devices to affect vertical or transverse discrepancies (Figure 7).2,5
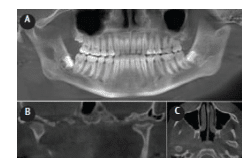 FIGURE 6. Reformatted panoramic (A), 2 mm orthogonal coronal (B), and axial (C) sections through the mandibular condyles show left healed and remodeled condylar fracture. Note the remodeling of both the temporal glenoid fossa and mandibular condylar components such that there is no overall vertical discrepancy on the left side.
FIGURE 6. Reformatted panoramic (A), 2 mm orthogonal coronal (B), and axial (C) sections through the mandibular condyles show left healed and remodeled condylar fracture. Note the remodeling of both the temporal glenoid fossa and mandibular condylar components such that there is no overall vertical discrepancy on the left side.
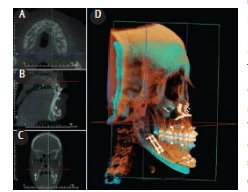 FIGURE 7. A screen shot of a computer program allowing superimposition of initial cone-beam computed tomography (CBCT) data (blue) with post-orthognathic treatment CBCT data (orange). Superimposition of reference anatomic landmarks in axial (A), sagittal (B), and coronal (C) reference planes provides a three-dimensional volumetric representation (D). FIGURE 7 COURTESY OF ANATOMAGE, SAN JOSE, CALIFORNIA.
FIGURE 7. A screen shot of a computer program allowing superimposition of initial cone-beam computed tomography (CBCT) data (blue) with post-orthognathic treatment CBCT data (orange). Superimposition of reference anatomic landmarks in axial (A), sagittal (B), and coronal (C) reference planes provides a three-dimensional volumetric representation (D). FIGURE 7 COURTESY OF ANATOMAGE, SAN JOSE, CALIFORNIA.
CBCT imaging also can be used to assess the airway—particularly for patients with obstructive sleep apnea (OSA)/hypopnea syndrome—but measurements should be interpreted with caution (Figure 8). For these individuals, CBCT images of the airway are most often acquired in the standing or seated position, whereas imaging should ideally be made with patients in the supine position. Although a number of studies have measured airways and changes in airways over time (particularly with regard to OSA), the reliability and validity of such measurements present a number of challenges. The boundaries of the nasopharynx with the maxillary/paranasal sinuses and the boundaries of the oropharynx with the oral cavity are not consistent among subjects and image acquisitions, and airway shapes and volumes vary markedly with dynamic processes, such as breathing and head postures.18–20
PATHOLOGY
CBCT imaging demonstrates the location, size, shape, extent, and full involvement of pathology of the jaws. Various conditions which may be encountered—most commonly infections (Figure 9), benign cysts, and tumors of the jaws—may require surgical intervention prior to orthodontic therapy.
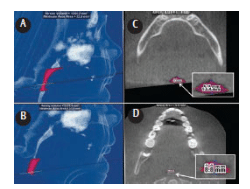 FIGURE 8. Lateral three-dimensional images of the segmented airway of a patient with obstructive sleep apnea/hypopnea syndrome showing the segmented volumes of retroglossal (A) and retropalatal (B) airway space. The software algorithm identifies and displays the axial images at which the minimum cross-sectional area is present (C and D) and allows for measurement of anteroposterior and transverse dimensions (inserts).
FIGURE 8. Lateral three-dimensional images of the segmented airway of a patient with obstructive sleep apnea/hypopnea syndrome showing the segmented volumes of retroglossal (A) and retropalatal (B) airway space. The software algorithm identifies and displays the axial images at which the minimum cross-sectional area is present (C and D) and allows for measurement of anteroposterior and transverse dimensions (inserts).
FIGURE 8 CREATED USING DOLPHIN 3D, DOLPHIN IMAGING AND MANAGEMENT SOLUTIONS, CHATSWORTH, CALIFORNIA
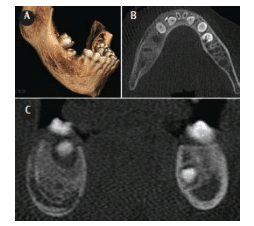 FIGURE 9. Volumetric three-dimensional rendering (A), axial (B), and coronal (C) images of a young patient with expansion of the right mandibular body and pain after failure of eruption of the right mandibular second molar with removal of an infected deciduous tooth. In view of the patient history, the regional intra-medullary sclerosis and “onion-skin” cortical laminations are suggestive of an exaggerated response to the infection Garre’s osteomyelitis with proliferative periostitis.
FIGURE 9. Volumetric three-dimensional rendering (A), axial (B), and coronal (C) images of a young patient with expansion of the right mandibular body and pain after failure of eruption of the right mandibular second molar with removal of an infected deciduous tooth. In view of the patient history, the regional intra-medullary sclerosis and “onion-skin” cortical laminations are suggestive of an exaggerated response to the infection Garre’s osteomyelitis with proliferative periostitis.
SUMMARY
CBCT is a valuable supplemental imaging modality to 2D radiography for the assessment and diagnosis of many specific conditions in the orthodontic patient. While evidence does not currently support CBCT imaging as a replacement for extraoral (lateral cephalometric and panoramic) radiography in orthodontics, it serves a valuable purpose in the diagnosis, treatment, and post-therapy stages of orthodontic treatment. CBCT imaging in orthodontics, however, should be used prudently, as it emits more radiation than traditional radiography. Its use among children should be very conservative, as their radiation risk is three to five times greater than that of adults for the same exposure.21–23
ACKNOWLEDGMENT
Some of this information was provided with permission from the American College of Radiology (ACR) and taken from the ACR Appropriateness Criteria®. The ACR is not responsible for any deviations from the original ACR Appropriateness Criteria content.
REFERENCES
- Scarfe WC, Pinheiro LR, Farman AG. Conebeam computed tomography. Dimensions of Dental Hygiene. 2014;12(4):60–64.
- Cevidanes LH, Tucker S, Styner M, et al. Threedimensional surgical simulation. Am J Orthod Dentofacial Orthop. 2010;138:361–371.
- Kapila S, Conley RS, Harrell WE Jr. The current status of cone beam computed tomography imaging in orthodontics. Dentomaxillofac Radiol. 2011;40:24–34.
- van Vlijmen OJC, Kuijpers MAR, Berge SJ, et al. Evidence supporting the use of cone-beam computed tomography in orthodontics. J Am Dent Assoc. 2012;143:241–252.
- Hechler SL. Cone-beam CT: applications in orthodontics. Dent Clin N Am. 2008;52:753–759.
- American Academy of Oral and Maxillofacial Radiology. Clinical recommendations regarding use of cone-beam computed tomography in orthodontics. [corrected]. Position statement by the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:238–257.
- Cevidanes LH, Alhadidi A, Paniagua B, et al. Three-dimensional quantification of mandibular asymmetry through cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:757–770.
- Engelbrecht WP, Fourie Z, Damstra J, Gerrits PO, Ren Y. The influence of the segmentation process on 3D measurements from cone beam computed tomography-derived surface models. Clin Oral Investig. 2013;17:1919–1927.
- White SC, Pae EK. Patient image selection criteria for cone beam computed tomography imaging. Semin Orthod. 2009;15:19–28.
- Edwards SP. Computer-assisted cranio maxillo – facial surgery. Oral Maxillofac Surg Clin North Am. 2010;22:117–134.
- Jayaratne YS, Zwahlen RA, Lo J, Tam SC, Cheung LK. Computer-aided maxillofacial surgery: an update. Surg Innov. 2010;17:217–225.
- Gateno J, Xia JJ, Teichgraeber JF. New 3-dimensional cephalometric analysis for orthognathic surgery. J Oral Maxillofac Surg. 2011;69:606–622.
- Orentlicher G, Goldsmith D, Horowitz A. Applications of 3-dimensional virtual computerized tomography technology in oral and maxillofacial surgery: current therapy. J Oral Maxillofac Surg. 2010;68:1993–1999.
- Tucker S, Cevidanes LHS, Styner M, et al. Comparison of actual surgical outcomes and 3-dimensional surgical simulations. J Oral Maxillofac Surg. 2010;68:2412–2421.
- Jayaratne YS, Zwahlen RA, Lo J, Tam SC, Cheung LK. Computer-aided maxillofacial surgery: an update. Surg Innov. 2010;17:217–225.
- Gateno J, Xia JJ, Teichgraeber JF. New 3-dimensional cephalometric analysis for orthognathic surgery. J Oral Maxillofac Surg. 2011;69:606-22.
- Schlicher W, Nielsen I, Huang JC, Maki K, Hatcher DC, Miller AJ. Consistency and precision of landmark identification in three-dimensional cone beam computed tomography scans. Eur J Orthod. 2012;34:263–275.
- Popat H, Richmond S. New developments in: three-dimensional planning for orthognathic surgery. J Orthod. 2010;37:62–71.
- Ogawa T, Enciso R, Memon A, Mah JK, Clark GT. Evaluation of 3D airway imaging of obstructive sleep apnea with cone-beam computed tomography. Stud Health Technol Inform. 2005;111:365–368.
- El H, Palomo JM. Measuring the airway in 3 dimensions: a reliability and accuracy study. Am J Orthod Dentofacial Orthop. 2010;137(Suppl 4):S50.
- van Vlijmen OJC, Kuijpers MAR, Berge SJ, et al. Evidence supporting the use of cone-beam computed tomography in orthodontics. J Am Dent Assoc. 2012;143:241–252.
- American Dental Association Council on Scientific Affairs. The use of cone-beam tomography in dentistry. An advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2012;143:899–902.
- Grünheid T, Kolbeck Schieck JR, Pliska BT, Ahmad M, Larson BE. Dosimetry of a cone-beam computed tomography machine compared with a digital x-ray machine in orthodontic imaging. Am J Orthod Dentofacial Orthop. 2012;141:436–443.
From Dimensions of Dental Hygiene. September 2014;12(9):71–74.



