Recognizing and Responding to Young-Onset Dementia
Though rare, young-onset dementia presents unique diagnostic, behavioral, and oral health challenges.
This course was published in the July/August 2025 issue and expires August 2028. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 750
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain the differences between young-onset dementia (YOD) and older-onset dementia.
- List the symptoms of YOD and describe the role of oral health professionals in identifying early signs of YOD and making referrals.
- Discuss the oral pathways of YOD.
While dementia is a neurodegenerative disease commonly associated with adults older than age 65, it can also impact younger individuals.1 Young-onset dementia (YOD) is a rare condition, affecting approximately 11 out of every 100,000 individuals between the ages of 30 and 64 each year.2,3 An estimated 6% to 9% of all individuals living with dementia worldwide are younger than age 65.4
The incidence of YOD is similar in men and women, though early symptoms often differ — men are more likely to show irritability, while women tend to experience more pronounced memory loss. Recognizing YOD can be difficult because the condition is rarely suspected in younger adults; it is often mistaken for other illnesses, such as depression, hormone deficiencies, or psychiatric problems.4-8 YOD is typically diagnosed after an average delay of 4.4 years — about 11.2 months longer than the average time to diagnose older-onset dementia (OOD) .1,3,9 To prevent delays, oral health professionals need to recognize YOD’s early signs and symptoms.
Symptoms, Diagnosis, and Risk Factors
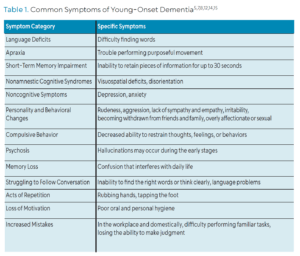
YOD symptoms vary depending on the subtype, with the most common being young-onset Alzheimer disease, frontotemporal dementia, vascular dementia, and Lewy body dementia.10-12 Across all subtypes, early symptoms commonly involve changes in behavior, language, and personality, along with challenges in managing thoughts, emotions, and actions.1,12,13
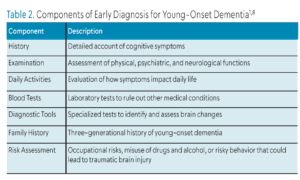
A systematic review and meta-analysis comparing clinical characteristics of YOD and OOD found that individuals with YOD had poorer baseline cognitive scores and faster cognitive decline, but a longer survival period after diagnosis.13 Additionally, YOD is less understood than OOD, resulting in limited resources and education for patients and their families.14 Table 1 lists the common symptoms of YOD while Table 2 includes the components for early diagnosis.1,5,7,8,12,14,15 Younger-onset patients will likely require dental care over a longer period, placing greater responsibility on oral health professionals to manage their treatment.
 Dental hygienists are often among the first healthcare providers to notice changes in a patient’s behavior. Recognizing symptoms and understanding the associated tests and diagnostic tools may better serve patients by promoting effective communication with both the patient and other healthcare providers. Various diagnostic tools and criteria are used to assess YOD. Some of the most commonly utilized imaging techniques and biomarker analyses include computerized tomography, magnetic resonance imaging, specialized cerebrospinal fluid analyses, and positron emission tomography with fluorodeoxyglucose.1,8,10
Dental hygienists are often among the first healthcare providers to notice changes in a patient’s behavior. Recognizing symptoms and understanding the associated tests and diagnostic tools may better serve patients by promoting effective communication with both the patient and other healthcare providers. Various diagnostic tools and criteria are used to assess YOD. Some of the most commonly utilized imaging techniques and biomarker analyses include computerized tomography, magnetic resonance imaging, specialized cerebrospinal fluid analyses, and positron emission tomography with fluorodeoxyglucose.1,8,10
Myriad factors may increase the risk of developing YOD, such as brain injury, heart disease, high blood pressure, neurodegenerative disorders, history of stroke, drug and alcohol use disorders, metabolic diseases, social isolation, and genetics.1,16,17 Those with a parent or grandparent with YOD are at increased risk of developing the disease.3,8,11 About 15% of all YOD cases are caused by an autosomal dominant mutation involving the genes encoding APP, PSEN1, or PSEN2; a person who inherits at least one copy of a mutated gene will likely develop Alzheimer disease before age 65.1,3
 Protective factors include attending college, consuming a Mediterranean diet, avoiding alcohol, staying socially active, exercising regularly, and participating in low-risk leisure sports.16-18 Dental hygienists can play an important role by recommending these beneficial lifestyle choices to patients who may be at risk for developing YOD.
Protective factors include attending college, consuming a Mediterranean diet, avoiding alcohol, staying socially active, exercising regularly, and participating in low-risk leisure sports.16-18 Dental hygienists can play an important role by recommending these beneficial lifestyle choices to patients who may be at risk for developing YOD.
Prognosis, Treatment Options, and Access Challenges
Obtaining an accurate differential diagnosis is essential for determining the disease progression and prognosis in people with YOD.1 Loi et al1 noted that those living with YOD typically live for many years after diagnosis, although there is an average life expectancy loss of 10 to 15 years. Individuals with YOD may benefit from a multidisciplinary approach to care including psychological support, home modifications and support, physiotherapy or exercise physiotherapy, daily living assistance, financial guidance, and future care planning.1
Feeling useful helps preserve a sense of control and self-esteem, especially in the early stages of the disease, as pleasant activities and hobbies can play a vital role in preserving a patient’s mental health and sense of self as dementia progresses. Dental hygienists can help these patients feel useful by keeping them involved in their oral care and by creating a safe environment in which their opinions matter. A thorough assessment of the specific disabilities experienced by the individual will help guide the best choices and modifications for nonpharmacological treatment and care.1
To manage YOD symptoms, patients often receive a combination of three or more central nervous system-acting medications (eg, antidepressants, benzodiazepines, opioids, and anticonvulsants).19 However, combining these medications can increase the risk of falls, opioid overdose, or accidental death.1,9 Medications that manage YOD symptoms, such as cholinesterase inhibitors, N-methyl-D-aspartate receptor blockers, and anti-amyloids, can help manage symptoms but they don’t slow the progression of the disease itself.1,20
Depression and anxiety can be managed through psychotherapy and antidepressants, with short-term benzodiazepines used in some cases. Those with YOD may experience sleep disturbances that can be addressed with melatonin or short-term, low-dose benzodiazepines. Individuals with YOD may not be able to express when they have pain therefore pain can be a significant issue and management strategies should be explored.1
If symptoms of YOD are severe, aggressive, or include psychosis, risperidone may be used for short periods of time, usually up to 12 weeks.1 Individuals will also need to make lifestyle changes, including managing cardiovascular risk factors and implementing healthy lifestyle habits, and doing brain stimulating tasks, such as playing video games, which may help slow cognitive decline.1,21,22
Patients with YOD require more healthcare than those without the disorder.Those residing in rural areas face higher barriers of access to care when compared to those living in urban areas, leading to a greater dependence on medications and higher mortality rates. Urban residents often have more geographic access to in-home or long-term care facilities.23
Oral Health and Inflammatory Pathways
Whether diagnosed with YOD or OOD, individuals with dementia often have poor oral health and more tooth loss due to impaired cognitive function, memory issues, and altered physical abilities. The effectiveness of oral care practices diminishes as finger dexterity and fine motor skills decrease.24 Poor oral conditions and tooth loss may not just be the result of dementia. Some studies suggest there may be a bidirectional causative relationship between dementia and poor oral health, as pathogens, such as Porphyromonas gingivalis, may invade the blood-brain barrier.24,25
Patients with periodontitis have a greater risk of developing dementia and neurodegenerative diseases due to systemic inflammation caused by the overexpression of pro-inflammatory cytokines. Systemic inflammation causes the reduction of important immune molecules, such as epidermal growth factor, interleukin 8 , interferon γ-induced protein 10, and monocyte chemoattractant protein-1. This decrease in immune molecules allows for P. gingivalis to play a dual role by evading the body’s natural defenses and by lowering interferon-γ (another immune molecule). The reduction of interferon-y makes it more difficult for the brain to remove the harmful substance amyloid beta plaque, which is related to neurodegenerative diseases.25
The Role of Oral Health Professionals
Patients diagnosed with YOD benefit from an established dental care routine as soon as possible following diagnosis.12 Consistency is essential for patients with dementia and establishing regular check-ups and daily oral care routines can address their oral health needs.26
The dental hygienist can help maintain the patient’s quality of life by providing compassionate care along with a sense of value and belonging.12 Dementia can affect individuals’ ability to care for their teeth, leading to increased plaque, significant gingival bleeding, and a greater need for assistance with oral hygiene.27,28
When treating a patient with dementia, the dental hygienist should consider the following:12,26,28-30
- Provide individualized care and allow patients to make informed decisions about their care as long as they are able
- Create a calm environment with mild stimulus to reduce confusion and agitation
- Use color and lighting to make sure chairs and floors are easy to see and identify
- Accompany the patient to and from the waiting room to prevent confusion and possible falls
- Keep patients with the same providers for consistency
- Ask one question at a time and allow ample time for responses
- Provide positive and clear directions while breaking down tasks into smaller steps
- Play calming or familiar music at a low volume to prevent overstimulation and improve mood
- Refer to people and objects or items by name
- If dentures are worn, encourage them to be cleaned regularly with a toothbrush or denture brush over a bowl or sink to prevent breaking if dropped
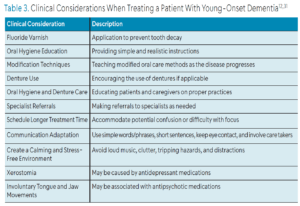 Individuals may experience mood changes, memory and behavioral issues, depression, self-injurious behaviors, show overly affectionate or sexual behavior, and refuse to cooperate during their treatment.12,31 Oral health professionals need to be compassionate and show empathy, understanding, and respect for the individual’s dignity.26 Table 3 provides a list of clinical considerations when treating a patient with YOD. Those with dementia may not be able to explain, describe, or understand oral pain.12,31
Individuals may experience mood changes, memory and behavioral issues, depression, self-injurious behaviors, show overly affectionate or sexual behavior, and refuse to cooperate during their treatment.12,31 Oral health professionals need to be compassionate and show empathy, understanding, and respect for the individual’s dignity.26 Table 3 provides a list of clinical considerations when treating a patient with YOD. Those with dementia may not be able to explain, describe, or understand oral pain.12,31
Conclusion
YOD is a chronic, terminal, neurodegenerative disease. It causes a variety of behavioral and cognitive changes. Those diagnosed with YOD often have reduced access to care with a greater need for healthcare visits. They can lose their sense of self and feelings of usefulness to society, leading to depression and anxiety. As the disease progresses, palliative care becomes necessary. Dental hygienists need to understand the physical, emotional, and societal difficulties faced by those with YOD.They need to educate patients and their caregivers on daily oral care practices.
References
- Loi SM, Cations M, Velakoulis D. Young-onset dementia diagnosis, management and care: a narrative review. Med J Aust. 2023;218:182-189.
- Hendriks S, Peetoom K, Bakker C, et al. Global incidence of young-onset dementia: a systematic review and meta-analysis. Alzheimers Dement. 2023;19):831-843.
- Mayo Clinic. When Alzheimer’s Symptoms Start Before Age 65. Available at mayoclinic.org/diseases-conditions/alzheimers-disease/in-depth/alzheimers/art-20048356. Accessed May 27, 2025.
- van de Veen D, Bakker C, Peetoom K, et al. An integrative literature review on the nomenclature and definition of dementia at a young age. J Alzheimers Dis. 2021;83:1891-1916.
- Edahiro A, Okamura T, Arai T, et al. Initial symptoms of early-onset dementia in Japan: nationwide survey. Psychogeriatrics. 2023;23:422-433.
- Hendriks S, Peetoom K, Bakker C, et al. Global prevalence of young-onset dementia: a systematic review and meta-analysis. JAMA Neurol. 2021;78:1080-1090.
- Australia H. Younger onset dementia. Available at healthdirect.gov.au/younger-onset-dementia. Accessed May 27, 2025.
- O’Malley M, Parkes J, Stamou V, LaFontaine J, Oyebode J, Carter J. Young-onset dementia: scoping review of key pointers to diagnostic accuracy. BJPsych Open. 2019;5:e48.
- Chiari A, Tondelli M, Galli C, et al. How long does it take to diagnose young-onset dementia? A comparison with late-onset dementia. Neurol Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol. 2022;43:4729-4734.
- Brown CW, Chen HY, Panegyres PK. Electroencephalography in young onset dementia. BMC Neurol. 2023;23:1-9.
- Csaban D, Illes A, Renata TB, et al. Genetic landscape of early-onset dementia in Hungary. Neurol Sci. 2022;43:5289-5300.
- Jeavons C. Dementia friendly dentistry. Dent Health (London). 2023;62:34-37.
- Seath P, Macedo-Orrego LE, Velayudhan L. Clinical characteristics of early-onset versus late-onset Alzheimer’s disease: a systematic review and meta-analysis. Int Psychogeriatr. 2024;36:1093-1109.
- Wiggins M, McEwen A, Sexton A. Young-onset dementia: A systematic review of the psychological and social impact on relatives. Patient Educ Couns. 2023;107:107585.
- Cascella M, Al Khalili Y. Short-term memory impairment. Available at ncbi.nlm.nih.gov/books/NBK545136. Accessed May 27, 2025.
- Bosi M, Malavolti M, Garuti C, et al. Environmental and lifestyle risk factors for early-onset dementia: a systematic review. Acta Bio Medica Atenei Parm. 2022;93:e2022336.
- Budson AE. A fresh look at risks for developing young-onset dementia. Available at health.harvard.edu/blog/a-fresh-look-at-risks-for-developing-young-onset-dementia-202401173008. Accessed May 27, 2025.
- Health Community Key. These 11 Sports Have the Lowest Risk of Injuries. Available at healthcommkey.org/11-sports-lowest-risk-injuries. Accessed May 27, 2025.
- Wei YJJ, Shrestha N, Chiang C, DeKosky ST. Prevalence and trend of central nervous system-active medication polypharmacy among US commercially insured adults with vs without early-onset dementia: a multi-year cross-sectional study. Alzheimers Res Ther. 2024;16:30.
- Fisher Center for Alzheimer’s Research Foundation. 5 Things to Know About Kisunla, the New Alzheimer’s Drug. Available at alzinfo.org/articles/treatment/5-things-to-know-about-kisunla-the-new-alzheimers-drug. Accessed May 27, 2025.
- Rao RV, Subramaniam KG, Gregory J, et al. Rationale for a multi-factorial approach for the reversal of cognitive decline in alzheimer’s disease and mci: a review. Int J Mol Sci. 2023;24:1659.
- Jia Y, Shi M, Yang P, et al. Associations of computer gaming with incident dementia, cognitive functions, and brain structure: a prospective cohort study and Mendelian randomization analysis. Alzheimers Res Ther. 2024;16:131.
- Arsenault-Lapierre G, Bui TX, Le Berre M, Bergman H, Vedel I. Rural and urban differences in quality of dementia care of persons with dementia and caregivers across all domains: a systematic review. BMC Health Serv Res. 2023;23:102.
- Nakamura T, Zou K, Shibuya Y, Michikawa M. Oral dysfunctions and cognitive impairment/dementia. J Neurosci Res. 2021;99:518-528.
- Said-Sadier N, Sayegh B, Farah R, et al. Association between Periodontal Disease and Cognitive Impairment in Adults. Int J Environ Res Public Health. 2023;20:4707.
- Mitchell G. Oral care for dementia – 10 top tips . Available at rcn.org.uk/news-and-events/Blogs/oral-care-for-dementia-10-top-tips-250823. Accessed May 27, 2025.
- Delwel S, Binnekade TT, Perez RSGM, Hertogh CMPM, Scherder EJA, Lobbezoo F. Oral hygiene and oral health in older people with dementia: a comprehensive review with focus on oral soft tissues. Clin Oral Investig. 2018;22:93-108.
- Dental Australia. Dental Care. Available at dementia.org.au/living-dementia/staying-healthy/dental-care. Accessed May 27, 2025.
- Digital T. 10 calming sensory activities for dementia patients. Available at bucknerwestminster.org/news-blog/10-calming-sensory-activities-for-dementia-patients. Accessed May 27, 2025.
- Mouth care. Dementia UK. Available at dementiauk.org/information-and-support/health-advice/mouth-care. Accessed May 27, 2025.
- Schaper S, Meyer-Rötz S, Bartels C, et al. Dental care of patients with dementia: a survey on practice equipment, training, and dental treatment. Front Oral Health. 2021;2:682139.
From Dimensions of Dental Hygiene. July/August 2025; 23(4):36-39.



