 RUSSELL KIGHTLEY/SCIENCE PHOTO LIBRARY
RUSSELL KIGHTLEY/SCIENCE PHOTO LIBRARY
Implant Instrumentation
We explain what the evidence says about the proper armamentarium for maintaining implant health.
Implant therapy has become a routine treatment for tooth loss due to its high success rates and positive effect on patient quality of life. Implant failure caused by infection surrounding soft or hard tissue, however, can occur. Peri-implant mucositis—inflammation of the soft tissue surrounding an implant with no resultant bone loss—is reversible with excellent oral hygiene and regular, professional cleaning of the implant surface and periodontal sulcus. Peri-implantitis, on the other hand, is characterized by soft tissue inflammation in addition to bone loss around the implant.1
Current evidence shows that peri-implant mucositis occurs in about 50% of implants placed within 9 years to 14 years,2 while peri-implantitis occurs in 12% to 47% of implants 5 years after placement.3 The inflammatory response due to the presence of bacterial biofilm in peri-implant tissue is comparable to periodontal tissues that develop gingivitis and periodontitis. Therefore, treatment and prevention of peri-implant mucositis and peri-implantitis are similar to that of gingivitis and periodontitis. In essence, the removal of bacterial biofilm and calculus is an essential principle in maintaining the long-term success of implants.4
ARMAMENTARIUM
Instruments for cleaning dental implants should effectively remove deposits and cause minimal damage. A variety of instruments have been proposed and reviewed for the proper maintenance of dental implants. However, mechanical procedures to clean the dental implant may negatively affect its biocompatibility by altering the titanium surface. Meschenmoser et al used scanning electron microscopy (SEM) to evaluate implant surfaces after instrumentation with a stainless steel curet, plastic curet, pure titanium curet, air abrasive polishing system, and ultrasonic scaler.5 The SEM revealed surface alterations for all instruments and systems except the plastic curet, which did not roughen the surface at all. The titanium curet and the air abrasive system registered only minor effects. These surface defects have an unpredictable peri-implant tissue reaction, so the titanium curet and air-powder polisher are recommended with restrictions. The stainless steel curet and ultrasonic scaler using a traditional metal insert/tip are not suitable for cleaning dental implants5,6 because they roughen the implant surface, which may change the response of the surrounding periodontal tissues, increasing biofilm retention and making it more difficult to remove.7
Scaling procedures with curets affect the cell adherence to the implant surface.8 The SEM demonstrated that both stainless steel and titanium-alloy curets had fewer attached cells, with the surfaces instrumented by the stainless steel curet showing the greatest reduction in cell attachment.5 This may be due to the possible chemical alteration produced by stainless steel that may result in changes to the oxide layer, alteration, or contamination to the implant surface, causing an increase in corrosion.8,9 These results are indicative of the biocompatibility of the titanium curet instruments.
Although Teflon-coated sonic and ultrasonic scalers, plastic curets, and air powder systems cause minimal damage to the implant surface, material residues have been found on rough surface implants.10,11 Deposits left on the surface may affect the tissue healing process, which can lead to the development of peri-implant mucositis or peri-implantitis.10 The ability to mechanically remove residual cement and calculus deposits is a consideration when choosing an implant scaler. Wilson found excess dental cement associated with signs of peri-implant disease in 81% of the cases evaluated.12 Clinical and endoscopic signs of peri-implant disease were absent in 74% of the test implants after the removal of excess cement was completed.12 Calculus deposits on implants are usually softer than on natural teeth and are generally supragingival rather than subgingival, which allows for easier removal.13 Mengel et al evaluated various instruments to determine the quantity of substance removal.6 The results showed that an ultrasonic scaler, sonic scaler with universal tips, and stainless steel Gracey curet left pronounced roughness on the titanium surface, but removed a considerable amount of deposits. The titanium curet and the sonic scaler left almost no alterations to the surface, but removed little of the deposits. The rubber cup, plastic curet, and air polishing system left the implant surfaces unchanged.6
INSTRUMENT SELECTION
With a wide variety of implant scalers available, dental hygienists need to select the proper instrument for specific implant surfaces, such as pure titanium, titanium alloy, titanium plasma spray, or hydroxyapatite-coated. Many studies have investigated the effects of hand scaling instruments on implant surfaces. Louropoulou et al found that nonmetal instruments cause minimal or no damage to both smooth and rough titanium surfaces, while metal instruments create the most damage to smooth surfaces.14 However, plastic instruments and inserts/tips may not be able to effectively removing calculus or leftover cement.11,15 Additionally, they may leave behind plastic particles on the implant surface.11,15
Before choosing an instrument, dental hygienists should know the name, type, and company that manufactured the implant. A visual examination or tactile sensation is not sufficient to determine what type of surface an implant is made from. As such, dental hygienists are responsible for inquiring about the texture of the implant prior to treatment if the implant is exposed above the bone level due to bone loss. Clinicians should also refer to radiographs to determine whether the implant surface is within reach of the instrument or if it can only reach the abutment surface. Comparing radiographs at the time of implant placement with current radiographs is also helpful in determining if there is a change in bone level and implant exposure.
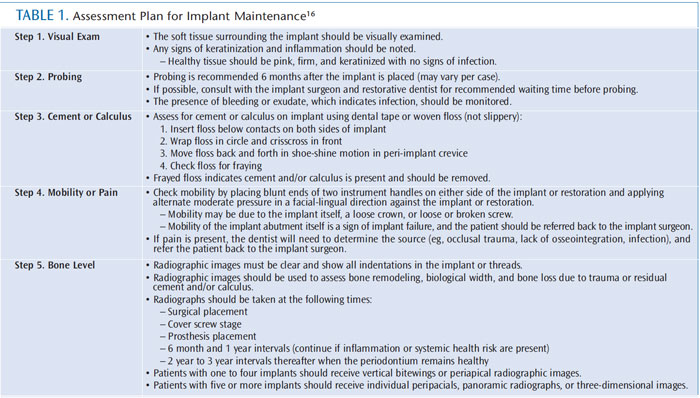
ASSESSMENT
Prior to selecting an instrument, dental hygienists must assess the health of the periodontium in order to identify the necessary instrument for the maintenance of the implant. Table 1 provides a five-step assessment plan for comprehensive implant maintenance—from the visual examination to monitoring bone levels.16 The use of the dental endoscope can be helpful in the subgingival assessment of dental implants and surrounding peri-implant tissue. Chemotherapeutic agents can also be considered to aid in the disruption of biofilm that contaminate the exposed surface of titanium implants.17 Studies have shown conflicting results with the use of chemotherapeutic agents so the proper course of treatment should be based on the individual needs of the patient.18 Hand instrumentation is still needed for complete removal of the biofilm, calculus, and residual cementum. When peri-implantitis is present, the use of Er:YAG and CO2 lasers may be indicated in decontamination treatment. 19 Although beyond the scope of this article, the use of lasers in implant care shows promise, but more research is needed to determine the long-term results.
SUMMARY
Thorough assessment techniques, use of cutting-edge technology, and continuing education are all important parts of effective implant maintenance. However, maintenance programs should be customized on a case-by-case basis due to the lack of data defining the precise recare intervals and instrumentation methods for proper maintenance of dental implants.20
REFERENCES
- Berglundh T, Lindhe J, Ericsson I, Marinello CP, Liljenberg B, Thomsen P. The soft tissue barrier at implants and teeth. Clin Oral Implants Res. 1991;2:81–90.
- Roos-Jansaker AM, Lindahl C, Renvert H, Renvert S. Nine-to-fourteen-year follow-up of implant treatment. Part II: Presence of peri-implant lesions. J Clin Periodontol. 2006; 33:290–295.
- Zitzmann NU, Berglundh T. Definition and prevalence of peri-implant diseases. J Clin Periodontal. 2008;35(Suppl):286–291.
- Hultin M, Komiyamma A, Klinge B. Supportive therapy and the longevity of dental implants: a systematic review of the literature. Clin Oral Impl Res. 2007;18:50–62.
- Meschenmoswer A, Berndt d’Hoedt, Melyle J, et al. Effects of various hygiene procedures on the surface characteristics of titanium abutments. J Periodontol. 1996;67:229–235.
- Mengel R, Buns CE, Mengel C, Flores-de-Jacoby L. An in vitro study of the treatment of implant surfaces with different instruments. Int J Oral Maxillofac Implants. 1998;13:91–96.
- Meffert RM. The soft tissue interface in dental implantology. J Dent Educ. 1988;52:810–811.
- Dmytiyk JJ, Fox SC, Moriarty JD. The effects of scaling titanium implant surfaces with metal and plastic instruments on cell attachment. J Periodont. 1990;61:491–496.
- Rimondini L, Fare S, Brambilla E, et al. The effect of surface roughness on early in vivo plaque colonization on titanium. J Periodontol. 1997;68:556–662.
- Ramaglia L, di Lauro AE, Morgese F, Squillace A. Profilometric and standard error of the mean analysis of rough implant surfaces treated with different instruments. Implant Dent. 2006;15:77–82.
- Rühling A, Kocher T, Kreusch J, Plagmann HC. Treatment of subgingival implant surfaces with Teflon-coated sonic and ultrasonic scaler tips and various implant curettes. An in vitro study. Clin Oral Implants Res. 1994;5:19–29.
- Wilson TG Jr . The positive relationship between excess cement and periimplant disease: a prospective clinical endoscopic study. J Periodontol. 2009;80:1388–1392.
- Darby ML, Walsh MM. Dental Hygiene Theory and Practice. Philadelphia: WB Sauders Co; 1995.
- Louropoulou A, Slot D, Van der Weijden F. Titanium surface alterations following the use of different mechanical instruments: a systematic review. Clin Oral Implants Res. 2012;23:643–658.
- Mann M, Parmar D, Walmsley AD, Lea SC. Effect of plastic-covered ultrasonic scalers on titanium implant surfaces. Clin Oral Implants Res. 2012;23:76–82.
- Wingrove SS. Peri-implant Therapy for the Dental Hygienist: Clinical Guide to Maintenance and Disease Complications. Hoboken, NJ: Wiley-Blackwell; 2013.
- Henderson E, Schneider S, Peterson FC, et al. Chemical Debridement of contaminated titanium surfaces: an in vitro study. Acta Odontol Scand. 2013;71:957–964.
- Norton MR. The history of dental implants. US Dentistry. 2006;9:24–26.
- Peters N, Tawse-Smith A, Leichter J, Tompkins G. Laser therapy: the future of peri-implantitis management? Braz J Periodontol. 2012;22:26–33.
- Iacono VJ; Committee on Research, Science and Therapy, the American Academy of Periodontology. Dental implants in periodontal therapy. J Periodontol. 2000;71:1934–1942.
From Dimensions of Dental Hygiene. June 2013; 11(6): 16–18.

