
Posture Makes Perfect
Follow these ergonomic strategies to improve your musculoskeletal health.
Dental hygienists are at risk of musculoskeletal disorders, despite paying careful attention to preventive strategies. The overall prevalence of musculoskeletal disorders among dental hygienists may be as high as 96%.1-5 Dental professionals experience more neck pain,3,4,6 shoulder pain,3,4 and hand pain1,4,5 than the general population.  Musculoskeletal pain impacts not only comfort on the job and self-perceived competency, but also quality of personal life.7-9 Bylund7 found that musculoskeletal discomfort interfered with activities of daily living, in addition to delivery of dental hygiene services among female dental hygienists. Ultimately, the physical demands of sustained and awkward postures in the dental profession are key reasons for job attrition.8,9
Musculoskeletal pain impacts not only comfort on the job and self-perceived competency, but also quality of personal life.7-9 Bylund7 found that musculoskeletal discomfort interfered with activities of daily living, in addition to delivery of dental hygiene services among female dental hygienists. Ultimately, the physical demands of sustained and awkward postures in the dental profession are key reasons for job attrition.8,9
Ergonomic interventions can help minimize common musculoskeletal risks in dental practice.4,10,11 Ergonomics—the study of the interaction between individuals and their jobs—promotes comfort, productivity, and workplace safety through the recommendation of optimal work environments and processes.12 For dental professionals, environment includes clinical instruments, equipment, and office setup. Work tasks or processes refer to proper use of the body while performing preventive treatment, radiographs, intraoral and extraoral examinations, charting, administration of local anesthesia, scaling and root planing, and other tasks. By adhering to three key ergonomic principles, dental professionals can reduce their risk of injury and sustain their ability to practice clinically.
Ergonomic Principle #1
The first ergonomic principle important to dental professionals is that neutral posture promotes a balance of muscle forces in the body. Workers should minimize time spent in awkward postures—the cause of many musculoskeletal disorders. When dental professionals use their bodies in unnatural positions, muscles must generate higher forces to accomplish a task than when muscles contract efficiently in a balanced, neutral posture.13 A neutral posture includes keeping the head upright, shoulders relaxed, elbows flexed to 90º, forearm in a mid-position (thumbs up), wrists straight, back straight (maintaining the natural curves), knees bent at 90º, and feet flat on the floor.4,10
Dental professionals often assume a forward head and trunk flexed posture. Over time, this posture may lead to shortened neck and shoulder muscles (scalene, upper trapezius, and pectoral minor) and lengthened upper back or “posture muscles” (middle trapezius, rhomboids, and serratus anterior), which lead to round-shouldered posture. Muscle imbalances may also develop in the forearm and finger muscles so that finger flexor muscles, wrist extensor muscles, and forearm muscles become tight with continual use.4,6,10 Table 1 defines awkward postures for different parts of the body.
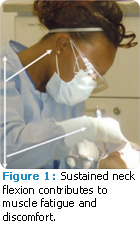
Positions of neck flexion greater than 20º may cause neck fatigue and pain because neck muscles must generate higher forces just to maintain a forward head position (Figure 1). In order to maintain an upright neck and head position, clinicians should adjust their seats so the patient’s mouth is close to the height of their elbows. Clinicians should seat themselves comfortably around and under the patient’s head. This provides access to the oral cavity while minimizing forward flexing of the neck and trunk. Branson’s Posture Assessment Instrument (BPAI),14 a validated posture assessment tool, can help clinicians examine the posture of their peers and document neck angle during instrumentation. Depending on the length of the clinician’s torso, the maxillary occlusal plane should be placed perpendicular to the floor (chin up) when treating the maxilla. When treating the mandible, clinicians should position the mandibular occlusal plane parallel to the floor (chin down). Magnification loupes also promote upright neck posture; lenses and prisms are used to magnify and focus the line of sight without compromising neck position.10,11,14 The use of doublesided mouth mirrors for indirect vision also minimizes the need to laterally bend the neck to view the oral cavity.10
When dental practitioners hold their arms away from the body during instrumentation, excessive forces are generated in shoulder musculature. Such muscle force translates to shoulder fatigue, trigger points, and even shoulder tendinitis.6 Dental professionals are encouraged to reduce reach distances by positioning the patient’s oral cavity at the height of their elbows.4,10 Upper back (thoracic spine) and lower back (lumbar spine) positions that are flexed or leaning forward demand greater muscle exertion and create high spinal compression forces.4,13 Clinicians can improve weak posture by asking patients to change positions, such as lifting or lowering the chin, turning the head right or left, or adjusting the head rest. The headrest on the patient’s chair can be extended to allow clinicians to position themselves closer to the oral cavity, with legs placed under the headrest. This strategy can prevent twisting of the torso and bending the trunk forward. The position of the patient’s occlusal line of the maxillary teeth becomes a focal point that affects the spinal positioning and overall posture of the clinician.
Patient chairs should enable clinicians to get as close to the patient as possible without flexing their trunks. If the chair design prohibits this strategy, clinicians can extend the headrest and position the patient to the headrest (Figure 2B). Standup dentistry is another option for individuals with long torsos, or those with existing back pain. In stand-up dentistry, the entire body must be erect and the patient’s chair should be adjusted up. Alternating between sit-down and stand-up dentistry may be a healthy option for some dental hygienists.
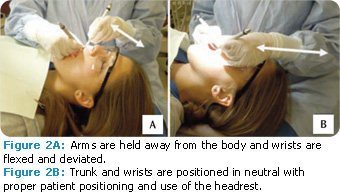
Extremes of wrist flexion (bent down), extension (bent back), and deviation (bent to the side) create excessive forces, especially when combined with pincer grasp for holding instruments.4,12 During extremes of wrist flexion and extension, nerves and tendinous structures push against the carpal bones and the flexor retinaculum (band) while keeping structures within the carpal canal. Over time, compression, friction, and irritation within the carpal tunnel may lead to carpal tunnel syndrome or tendinitis. Dental professionals should strive to keep wrist motions in a middle range (Figure 2).
Ergonomic Principle #2
The second ergonomic principle is that dynamic movement of the body minimizes static forces. Static forces are created when individuals hold their bodies in one position (usually against gravity) for an extended period of time.12 Although static positions appear to be restful or nonfatiguing, the opposite is true. When clinicians actively move muscles, muscle contraction and relaxation promote blood flow, circulation of nutrients, and removal of muscle waste.12 During static positions, such as holding the shoulder away from the body, tensed muscles compress blood vessels and reduce blood flow, decreasing oxygen and energy supply to the muscle. Waste products from muscles accumulate, causing muscle fatigue and, eventually, pain. Even at very low levels of effort, static contractions can cause fatigue.12 Abdominal and back muscles statically support the trunk to allow mobility in arms and hands.
Solutions to the static forces problem include supporting the trunk, moving periodically, and stretching. Traditional dental chairs should provide support for the back, buttocks, and legs with options for seat tilt. Chair designs are becoming more innovative with options to stabilize the body from posterior and anterior positions. The anteriorest, a proximal support attached to the patient chair, allows for anterior support of the trunk, while arms are free for movement. Clinicians should move regularly, whether standing up to change positions, procure instruments, retrieve charts, or access the computer. Any change in position improves blood flow.
Stretching can promote dynamic movement that is important for muscle health, balance of forces, and blood flow. Dental professionals should perform stretches throughout the day (not just at lunch), using the time between patients or procedures to sneak in a stretch—such as back stretches after treating a patient, wrist stretches between instrument changes, and neck stretches between patients or after charting. Dental professionals should make sure to hold stretches for 10 seconds to 30 seconds, stretching muscle groups in the opposite of static positions.4
Ergonomic Principle #3
The last ergonomic principle is to use as little force as possible to accomplish the job. Larger diameter handles decrease exerted grip forces. Dental hygienists use finger musculature repetitively throughout the day, exerting high forces during instrumentation for some scaling procedures. The combination of repetitive use and high forces places strain on tendon structures and increases the potential for carpal tunnel syndrome. Thus, clinicians are encouraged to minimize hand forces whenever possible.10 Strategies for reducing force during instrumentation include: keeping instruments sharpened; working in a neutral position (avoid excessive wrist flexion); using an ultrasonic scaler or automated equipment; choosing ergonomic instruments; and using extraoral (palm up or palm down) or intraoral built-up fulcrums.4,10,11,15,16 Dong et al15 found that although finger stabilization is typically used for precision, finger rests (using fourth and fifth fingers as a fulcrum to stabilize the hand) actually decrease thumb and pinch forces during instrumentation.
Two-finger rests consistently lowered thumb muscle forces, while one-finger rests sometimes lowered forces. Using the ring and pinky fingers as a fulcrum, however, may not be practical in some areas of the oral cavity. Lightweight instruments (ie, hollow) with large-diameter handles are designed to minimize the required pinch forces to manipulate the instrument because minimal force is needed to hold the instrument.10,12 Handle designs with large diameters (up to 10 mm) and minimal weight (15 gm) require the least amount of muscle effort and pinch forces.16
In summary, ergonomic principles can help clinicians minimize the muscle forces needed while maintaining optimal posture. Attention to these key principles will help reduce the risk of musculoskeletal disorders frequently faced by dental professionals.
REFERENCES
- Akesson I, Johnsson B, Rylander L, Moritz U, Skerfving S. Musculoskeletal disorders among female dental personnel—clinical examination and a 5-year follow-up study of symptoms. Int Arch Occup Environ Health. 1999;72:395-403.
- Lalumandier JA, McPhee SD, Parrott CB, Vendemia M. Musculoskeletal pain: Prevalence, prevention, and differences among dental office personnel. General Dentistry. 2001;49(2):160-166.
- Morse T, Bruneau H, Michalak-Turcotte, C, et al. Musculoskeletal disorders of the neck and shoulder in dental hygienists and dental hygiene students. J Dent Hyg. 2007;81:10.
- Sanders M, Michalak-Turcotte C. Preventing work-related MSDs in dental hygienists. In: Sanders M, ed. Ergonomics and the Management of Musculoskeletal Disorders. St. Louis: Butterworth Heinemann; 2004:448-469.
- Szeluga R. A survey of work-related musculoskeletal complaints among dental hygienists in Kentucky. Paper presented at: American Industrial Hygiene Association Conference; New Orleans: 2001.
- Wazzan KA, Almas K, Shethri SE, Qahtani MQ. Back and neck problems among dentists and dental auxiliaries. J Contemp Dent Pract. 2001;2:17-30
- Bylund SH, Ahlgren C. Experiences and consequences for women with hand-arm vibration injuries. Work. 2010;35:431-439.
- Ylipää V, Arnetz BB, Preber H. Factors that affect healthy and well-being in dental hygienists: a comparison of Swedish dental practices. J Dent Hyg. 1999;73:191-199.
- Ylipää V, Arnetz BB, Preber H, Benkö SS. Determinants of work satisfaction among Swedish dental hygienists. Scand J Caring Sci., 1996;10:247-253.
- Murphy DC, ed. Ergonomics and the Dental Care Worker. Washington, DC: American Public Health Association; 1998.
- Smith CA, Sommerich CM, Mirka GA, George MC. An investigation of ergonomic interventions in dental hygiene work. Appl Ergon. 2002;33:175-184.
- Kroemer E, Grandjean E. Fitting the Task to the Human: a Textbook of Occupational Ergonomics. 5th ed. Philadelphia: CRC Press; 2001.
- LeVangie PK, Norkin CC. Joint Structure and Function: a Comprehensive Analysis. 4th ed. Philadelphia: FA Davis; 2005.
- Branson BG, Black MA, Simmer-Beck M. Changes in posture: a case study of a dental hygienist’s use of magnification loupes. Work. 2010;35:467-476.
- Dong H, Barr A, Loomer P, Rempel D. The effects of finger rest positions on hand muscle load and pinch force in simulated dental hygiene work. J Dent Ed. 2005; 69:453-460.
- Dong H, Barr A, Loomer P, LaRoche C, Young E, Rempel D. The effects of periodontal instrument handle design on hand muscle load and pinch force. J Am Dent Assoc. 2006;137:1123-1130.
From Dimensions of Dental Hygiene. November 2011; 9(11): 30-32, 35.

