Develop a Documentation Protocol
Effective documentation of oral pathology can mean the difference between early and late detection of cancerous lesions.
 The early detection of oral lesions is integral to the effective diagnosis and treatment of oral cancer, an often deadly disease that affects more than 37,000 Americans each year.1 Dental hygienists are frequently the first clinicians to examine the oral cavity and their acumen in detecting and documenting the presence of oral lesions can mean the difference between early and late stage diagnosis. The proper documentation of oral lesions can rule out or confirm life-threatening lesions in patients. It is the dental hygienist’s professional responsibility to document the details associated with observed lesions within the oral cavity. A patient’s life may depend on the clinician’s thorough examination, documentation, and follow-up.
The early detection of oral lesions is integral to the effective diagnosis and treatment of oral cancer, an often deadly disease that affects more than 37,000 Americans each year.1 Dental hygienists are frequently the first clinicians to examine the oral cavity and their acumen in detecting and documenting the presence of oral lesions can mean the difference between early and late stage diagnosis. The proper documentation of oral lesions can rule out or confirm life-threatening lesions in patients. It is the dental hygienist’s professional responsibility to document the details associated with observed lesions within the oral cavity. A patient’s life may depend on the clinician’s thorough examination, documentation, and follow-up.
RIGHT START
When documenting findings in the oral cavity, dental hygienists should develop a consistent pattern or sequence to their examination to ensure that no areas are missed. Developing a routine for oral pathology examination helps dental hygienists provide detailed summaries of their findings regardless of the system used (traditional or paperless).2,3 The first steps in effective and legally-binding documentation include the availability of enough space for written information and the use of permanent black ink in all documentation. Black ink is preferred for handwritten documentation because it photocopies clearly. Sufficient space is necessary for documentation to take place on each line without adding information within the margins of the document. Data added off to the side and information noted with pencil or nonpermanent ink are not legally viable because they suggest that the documentation could have been tampered with. In addition, sufficient space has to be reserved for future appointments with the patient.2,4,5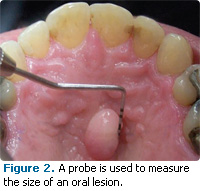
LESION HISTORY
Proper documentation of potential pathology must include the history of the condition. The length of time that the suspicious area has been present should be noted. In addition, any changes or presence of pain should be documented. Recurrences of the area with the date of the last incidence and any related discomfort or symptoms need to be included. The successful management of the lesion is dependent on the correct documentation of this information. It is also important to note whether patients are aware that the lesion is present or if they are being informed of its presence for the first time. Dental hygienists need to be careful when informing patients of the presence of a lesion in order to prevent undue fear and anxiety regarding the detection. Proper follow-up must be thoughtfully and strongly encouraged.2,3,6
LOCATION
Additional documentation and assessment pertaining to the specific location should be described in a detailed anatomical manner. These details must be specific so that any dental professional can immediately find the correct area and identify it. A diagram of the oral cavity should be included in the record so a detailed drawing of the area of concern can be included. Figure 1 provides a sample form used to document intraoral and extraoral examinations. It is also helpful to include actual photos of the lesion. Intraoral cameras and photo management software make the creation and storage of images simple.2,3,6,7
TABLE 1. TERMS COMMONLY USED TO DESCRIBE EXTENT
Localized: Confined to small focal area.
Generalized: Involves a majority of an area.
Single lesion: One lesion exists with a confined border.
Multiple lesions: More than one lesion exists.
- May be separate existing in a group.
- May be close with no distinct borders
DESCRIPTION
The extent of the suspect area must be documented, eg, “lesion involves one quarter of the right side of the dorsum area of the tongue.” Examples of commonly used terms to describe extent are listed in Table 1.2,3,6The size of lesions is usually noted in millimeters. Documentation of items such as length, width, and height of the lesion are a significant part of documentation. A probe can be used to accurately and precisely obtain these measurements (Figure 2).2,3,6 A color description of the area should use adjectives such as red, pink, white, bluish, purple, gray, yellow, black, and brown.2,3,6
Surface texture and configuration may be described as smooth or having irregular surfaces. Additional descriptors frequently include papillary, verrucous/wartlike, fissured, flat, depressed, traumatic, corrugated, or encrusted.2,4,6 Common terms used to describe consistency as related to lesions include soft, spongy, resilient, hard, and indurated.2,3,6 Table 2 includes additional terms used to describe lesions.2
Morphology
TABLE 2. OTHER FREQUENTLY USED TERMS TO DESCRIBE LESIONS
Crust: Outer layer or scab formed from dried fluid.
Erythema: Area red in color of inconsistent size and shape.
Exophytic: Outward growth.
Papillary: Small nipple-like protrusion.
Petechia: Very small hemorrhagic spots.
Pseudomembrane: Loose layer of cells that occur during inflammation of the tissue.
Polyp: Lesion that projects out or up from the level of the tissue.
Punctate: Lesion consisting of spots that are delineated by differences in color, height, or texture.
Verrucous: Wart-like and rough in texture.
The morphology of most lesions falls under three categories: elevated, depressed, or flat. Elevated lesions are situated above the plane of the tissue and are noted as either blister-like or nonblister-like. When lesions are blister-like in appearance, they are fluid filled, soft, translucent, and can show fluid movement when manipulated. These lesions are further classified as vesicles (small and circumscribed lesions with surface coverings that contain fluid and appear white in color). Additional classification categories within the blister-like category include pustule (larger in diameter and containing yellow-colored pus) and bulla (larger than vesicles and may contain blood).2,3,6 There are four types of lesions classified as nonblister-like. The word tumor describes a nonblister-like lesion that is usually 20 mm or larger. Plaque, a slightly raised lesion with a broad, flat top larger than 5 mm in diameter, is also included within this particular group.2,3,6 These nonblister-like lesions are solid in nature and do not contain fluid. They are further referred to as papules, which are very small, solid lesions that present as pointed, rounded, and flattopped in appearance. The term nodule is used to describe nonblister-like lesions larger than papules.
Depressed lesions appear below the line of the tissue. They take on a defined or irregular border and may be raised or flat around the existing border. Additional adjectives used in their description include superficial or deep (3 mm or more). Depressed lesions are grouped into the ulcer and erosion categories. Ulcers most often contain a loss of epithelium with the center appearing gray to yellow circled by a red border. Ulcers are frequently caused by the opening up of an elevated lesion, such as a vesicle, pustule, or bulla. The term erosion refers to a lesion that is shallow and depressed in appearance. It does not travel through the epithelium to the underlying layers of the tissue.2,3,6
Flat lesions occur on the same plane as the tissue. They may occur as individual or numerous lesions and can have either irregular or defined borders. The term macule is used to describe a circumscribed area not raised above the tissue that takes on a contrasting color when compared to its surroundings.2,6
PROPER FOLLOW-UP
Proper follow-up with documentation should occur immediately. A biopsy of the lesion can be facilitated with a referral to a specialist for additional diagnosis. A biopsy includes the removal and microscopic examination of tissue in order to determine a diagnosis. A biopsy is indicated when the lesion has not disappeared or showed improvement within 7 days to 14 days. A biopsy is always needed to confirm the diagnosis and begin proper treatment.
There are two types of biopsies: excisional and incisional. Excisional is when the entire lesion is removed and examined and incisional is when a sample section of the lesion is removed and examined. Any suspicious lesion that cannot be identified visually must be examined closer along with any lesion that has not exhibited healing within a 2-week period. If a lesion is thick, white, hyperkeratotic, and does not break through the surface tissue, a biopsy is indicated.2,3,6,7
TABLE 3. CLASSIFICATIONS OF FINDINGS FROM THE LABORATORY REPORT2
Unsatisfactory: Slide cannot be used for diagnosis purposes. Sample may not be adequate. Another one should be prepared as soon as possible.
Class I: Normal.
Class II: Atypical report. Not suggestive of the presence of malignant cells.
Class III: Uncertain (possibility of cancer).
Class IV: Indication probable for cancer.
Class V: Test positive for cancer.
All documentation regarding biopsy results must be included within patients’ records in addition to proper follow-up for the various reports. Class I and Class II reports require that the patient be monitored closely during the healing process. If healing does not take place within a reasonable period, another biopsy should be obtained.
Results reported as Class III indicate a need for the re-evaluation of clinical findings where biopsies are usually indicated to confirm the presence or absence of cancer. In Class IV or Class V reports, follow-up should automatically include a referral for further biopsy. If a lesion remains visible and creates suspicion, it is always smart to rule out the possibility of a false negative test result and conduct another biopsy.2,3,8 Table 3 provides a summary of biopsy classifications.
CONCLUSION
Meticulous examination and extensive documentation of existing conditions observed from intraoral and extraoral exams are imperative to the total assessment of patients for proper treatment planning. Lesions are often identified without the patient even knowing they exist because many are asymptomatic. It is our professional responsibility to make every effort possible to detect suspicious lesions early and rule out the presence of cancer.4,9,10
REFERENCES
- Oral Cancer Foundation. Oral Cancer Facts. Available at: http://oralcancerfoundation.org/facts/index.htm. Accessed March 17, 2011.
- Wilkins EM. Clinical Practice of the Dental Hygienist. 10th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2009:181-194.
- Newland RJ, Meiller TF, Wynn RL, Crossley HL. Oral Soft Tissue Diseases: A Reference Manual for Diagnosis and Management. 2nd ed. Hudson, NY: Lexi Comp Inc; 2002:4-13.
- Bernoni L, Leeuw W. Maintaining proper dental records. Dent Assist. 2008;77:6-15.
- Cummins R, Ganser T. Documentation guide lines protect against lawsuits. Provider. 1992; 18:47.
- Daniel SJ, Harfst SA, Wilder RS, Budenz AW, Young DA. Mosby’s Dental Hygiene Concepts, Cases, and Competencies. 2nd ed. Philadelphia: Mosby Inc; 2008:291-306.
- Alexander RE, Wright JM, Thiebaud S. Evaluating, documenting and follow up oral pathological conditions: a suggested protocol. J Am Dent Assoc. 2001;132:329-335.
- Ibsen O, Phelan JA. Oral Pathology for the Dental Hygienist. 5th ed. Philadelphia: Saunders/Elsevier; 2009:1-26.
- Osborn JB, Stoltenberg JL, Newell KJ, Osborn SC. Adequacy of dental records in clinical practice: a survey of dentists. J Dent Hyg. 2000;74:297-306.
- DeVore L, Fried JL, Dailey J, Ganssle QC. Dental hygiene self-assessment: a key to quality care. J Dent Hyg. 2000;74;271-279.
From Dimensions of Dental Hygiene. April 2011; 9(4): 38, 40, 42-43.

