 FATCAMERA/E+/GETTY IMAGES PLUS
FATCAMERA/E+/GETTY IMAGES PLUS
Managing Patients Undergoing Cancer Therapy
Dental hygienists must be knowledgeable about cancer therapies and the implications for oral healthcare.
This course was published in the November 2021 issue and expires November 2024. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the types, possible side effects, and oral manifestations of cancer therapy.
- Create an informed treatment plan for patients undergoing cancer therapy.
- Describe how to work with healthcare professionals to optimally care for patients undergoing cancer therapy.
The National Cancer Institute estimates the number of new cancer cases—diagnosed at any site in the body—in the United States in 2021 will be 1,898,160.1 Cancer is most frequently diagnosed in people ages 65 to 74, with 66 being the mean age of diagnosis.1 The 5-year relative survival rate is 67.7%.1 Sex impacts risk as well, as men have a 40.1% chance and women have a 38.7% chance of developing cancer in an invasive site.2 Because of this high likelihood, dental hygienists need to understand the types of cancer therapies, their effects on the oral cavity, and the treatment considerations for patients undergoing cancer therapy.
Cancer Therapies
Dental hygienists need to gather additional information about the type, duration, and side effects of cancer therapy. Individual treatment options may vary significantly among patients based on cancer type and stage, goals of treatment, and available therapies. Categories for cancer management include cancer rehabilitation, psychosocial care, palliative care, and the transition to long-term survivorship.3
Cancer rehabilitation—including surgery, chemotherapy, radiation therapy, targeted therapy, immunotherapy, stem cell or bone marrow transplant, and hormone therapy—is the most extensive of the categories due to the plethora of cancer treatments available.3 These treatment options are for patients actively battling cancer and may be provided locally or systemically. Local treatments include radiation therapy or surgery, while systemic treatments include drug therapies that affect the whole body, such as chemotherapy, immunotherapy, or targeted therapy.3
Psychosocial care focuses on managing the psychosocial repercussions of undergoing cancer therapies such as difficulty coping, fear of death and dying, financial stress, and grief.4 Support may consist of counseling, group support, spiritual support, and educational resources with psychiatrists, psychologists, social workers, licensed counselors, or pastoral counselors.
Palliative care focuses on improving quality of life rather than immediate remission.5 This is most often offered on an outpatient basis or short-term hospital care. The care team typically comprises a palliative care doctor, palliative care nurse, social worker, dietitian, and patient navigator. Some teams also include a pastoral counselor. This team also provides support to family members or caregivers.6
The American Cancer Society defines “cancer survivor” as “anyone who has ever been diagnosed with cancer no matter where they are in the course of their disease.”4 Transition to long-term survivorship may include those in remission from cancer or those living with active cancer diseases. Both groups must undergo frequent checkups and treat cancer as a chronic illness to reduce the chance of recurrence.4
Role of the Dental Hygienist
With the rapidly evolving healthcare delivery system, dental hygienists are likely to transition into multidisciplinary roles. The national scope of practice for dental hygienists has also drastically changed. Dental hygienists who practice outside of the traditional private practice setting have more involvement in hospital dental clinics, schools, long-term care facilities, and community health centers.7,8 This expansion into nontraditional settings increases the diversity of patient populations, and, in turn, the likelihood of dental hygienists providing care to patients with a potential cancer diagnosis. Dental hygiene care for patients includes their time in the dental chair for their dental visits and communication and collaboration with the whole healthcare team.
Dental hygienists must be prepared to consistently communicate with the patient and the entire healthcare team about ongoing cancer diagnoses, treatment, and medications. While the patient’s oncologist is the primary resource for information related to the patient’s cancer treatment, interprofessional collaboration may include a variety of other professionals, including oncology nurses, primary care physicians, pharmacists, radiologists, psychologists, social workers, physical therapists, spiritual support, and other providers.9 Conversations about oral hygiene instructions and management with caregivers may also be warranted for patients undergoing more complex treatments.10
 Dental hygienists should also view their role as preventive by completing assessments for all patients, regardless of cancer diagnosis, to provide adequate prevention education. These prevention strategies include gathering a comprehensive health history, conducting oral cancer screenings, and assessing risk factors. Head and neck examinations, including oral cancer screening, can be beneficial for the early detection of oral cancers and potential sites for metastasis of other types of cancer. Dental hygienists should conduct extraoral and intraoral screenings to evaluate abnormal findings such as red or white features, thickening of tissues, soreness, difficulty chewing or swallowing, pain, numbness, and swelling of the jaw.11 Any detectable lesions should be measured, photographed, and carefully monitored. If lesions or other symptoms persist for more than 2 weeks, biopsy or referrals to a primary care physician or specialist are warranted.11
Dental hygienists should also view their role as preventive by completing assessments for all patients, regardless of cancer diagnosis, to provide adequate prevention education. These prevention strategies include gathering a comprehensive health history, conducting oral cancer screenings, and assessing risk factors. Head and neck examinations, including oral cancer screening, can be beneficial for the early detection of oral cancers and potential sites for metastasis of other types of cancer. Dental hygienists should conduct extraoral and intraoral screenings to evaluate abnormal findings such as red or white features, thickening of tissues, soreness, difficulty chewing or swallowing, pain, numbness, and swelling of the jaw.11 Any detectable lesions should be measured, photographed, and carefully monitored. If lesions or other symptoms persist for more than 2 weeks, biopsy or referrals to a primary care physician or specialist are warranted.11
Dental hygienists must also note risk factors associated with high cancer risk among their patients.12 Identifying these risk factors early in dental appointments may be an excellent tool for prevention education. Completing a thorough medical and social history before beginning treatment should be the primary method of assessing risk factors for cancer. The most common risk factors associated with invasive cancers include smoking and tobacco use, poor diet and lack of physical activity, exposure to sun and other types of radiation, viruses, and other infections.12
Dental Hygiene Care
When caring for patients undergoing cancer treatment, clinicians should ask the following questions:
- What information do I need from my patient and his or her oncologist before beginning treatment?
- What steps do I need to take during the appointment process to ensure quality care?
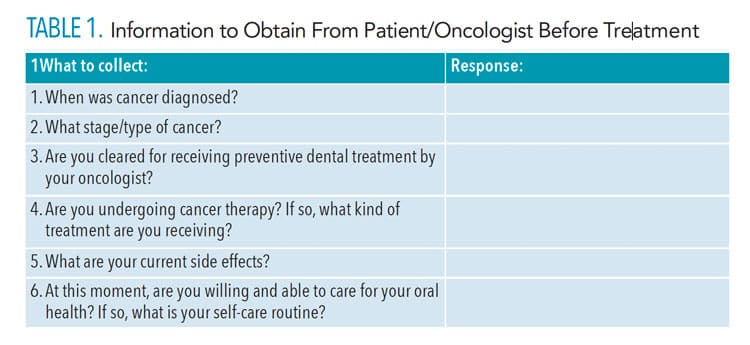
See Table 1 for a list of information needed prior to treating patients with cancer. The dental team should communicate directly with the patient or contact the patient’s oncologist to collect these details. Table 2 (page 38) provides a checklist for the appointment sequence.
Oral health professionals are responsible for early recognition and ongoing care of patients before, during, and after cancer therapies.13,14 Care includes preventive and therapeutic measures to ensure optimum oral health throughout cancer therapy. The better the patient’s oral health, the lower his or her risk for dental infections.14
![ABLE 2. Checklist for Appointment Sequence for Dental Hygiene Treatment]() Before Cancer Therapy
Before Cancer Therapy
When a patient is about to begin cancer treatment, the dental hygienist and dental team need to record the type of treatment that is planned.14 Next, a comprehensive dental evaluation should be done to eliminate existing oral disease, which may worsen during cancer therapy. The evaluation provides a baseline to compare and monitor the patient’s oral health. Upon initial assessment, the dental team should detail a treatment plan including prognosis, treatment options, and risks and benefits. Determining whether the cancer therapy is palliative or curative is important because it may impact goals for dental treatment.
Oral health professionals should prioritize treating infections, performing extractions, and providing periodontal care. Extractions may be warranted depending on the patient’s disease state and if the patient is receiving radiation in the head or neck regions. All extractions should be done before cancer therapy begins.14 The next phase of treatment should include caring for caries lesions and faulty restorations. If there is not enough time to complete a comprehensive treatment plan before cancer therapy begins, temporary restorations should be placed.
Dental hygienists should also provide prophylaxis to minimize the risk of oral complications when treatment begins and to optimize oral health. Further, individualized oral hygiene instructions should also be provided during these appointments.14 Information on the possible oral side effects of specific cancer therapies (eg, xerostomia) and what products may help with potential side effects. Patients should also receive written communication of the recommended self-care instructions and products. Nutritional counseling with a focus on a noncariogenic diet should also be conducted during this time. Following the preventive appointment and alongside the medical team’s recommendations, the dental hygienist should discuss a recare interval for the duration of ongoing cancer therapy.14
![TABLE 3. Possible Oral Manifestations of Patients Undergoing Cancer Therapy]() During Cancer Therapy
During Cancer Therapy
Many patients undergoing active cancer therapies develop oral complications.15 Consistent maintenance should be preventive but may also include active management of side effects and oral manifestations related to cancer therapies such as radiation and chemotherapy. Table 3 outlines a general guide for common oral manifestations, clinical presentation, and recommended oral hygiene instructions. Ongoing communication with the oncology team must also continue throughout cancer therapy.
Secondary complications, such as discomfort, malnutrition, treatment delays, and infections due to cancer therapy, may result.16 Oral health may not be a priority for patients with cancer due to the extraordinary amounts of physical and mental stressors they are experiencing.17 However, oral complications are common.17 Patient awareness of oral health manifestations and complications can positively impact their motivation to manage their oral health conditions.18 Additionally, emphasizing the bidirectional relationship between oral health and cancer treatment outcomes may help motivate patients.19
After Cancer Therapy
Following active cancer therapy, conversations with the patient’s oncology team must continue to assess whether the patient is in remission or has moved into palliative care. If the patient is in remission, the dental team should establish a short 1-month to 3-month recare interval for the first 2 years, before transitioning into a more standard 3-month to 6-month recare interval.14,20–22 Consistent recare intervals should continue due to patients’ increased risk for recurrent lesions, new lesions, or metastases; to assess complications from cancer therapies; and to emphasize excellent oral hygiene instructions.14,22 After undergoing cancer therapies, patients may experience chronic xerostomia, dysgeusia, altered bone, increased caries risk, muscle trismus, tooth sensitivity, and fungal infections. Many of these complications result from damage or alteration of tissues following cancer therapies.14,20–22
Conclusion
Dental hygienists play a key role in helping patients undergoing cancer therapy. Understanding cancer therapies and their effects on the oral cavity, in addition to composing questions for patients and other healthcare providers are fundamental in caring for patients with cancer. Further, an interprofessional approach ensures the patient receives the appropriate care and aids in quality of life.
References
- National Cancer Institute Surveillance, Epidemiology, and End Results Program. Cancer Stat Facts: Cancer of Any Site. Available at: seer.cancer.gov. Accessed October 19, 2021.
- American Cancer Society. Lifetime Risk of Developing or Dying from Cancer. Available at: cancer.org/cancer/cancer-basics/lifetime-probability-of-developing-or-dying-from-cancer.html Accessed October 19, 2021.
- American Cancer Society. Treatment Types. Available at: cancer.org/treatment/treatments-and-side-effects/treatment-types.html. Accessed October 19, 2021.
- American Cancer Society. Psychosocial Support Options for People with Cancer. Available at: cancer.org/treatment/survivorship-during-and-after-treatment/coping/understanding-psychosocial-support-services.html. Accessed October 19, 2021.
- American Cancer Society. What Is Palliative Care? Available at: cancer.org/treatment/treatments-and-side-effects/palliative-care/what-is-palliative-care.html. Accessed October 19, 2021.
- American Cancer Society. How and Where Is Palliative Care Provided and How Is it Paid for? Updated May 10, 2019. Available at: cancer.org/treatment/treatments-and-side-effects/palliative-care/who-provides-palliative-care.html. Accessed October 19, 2021.
- Fried JL, Maxey HL, Battani K, Gurenlian JR, Byrd TO, Brunick A. Preparing the future dental hygiene workforce: knowledge, skills, and reform. J Dent Educ. 2017;81:eS45-eS52.
- Westphal Theile C. Strengths and weaknesses of the current dental hygiene educational system. J Dent Educ. 2017;81:e38-e44.
- Cancer Support Community. Your Cancer Care Team. Available at: cancersupportcommunity.org/article/your-cancer-care-team. Accessed October 19, 2021.
- National Cancer Institute. Support for Caregivers of Cancer Patients. Available at: cancer.gov/about-cancer/coping/caregiver-support. Accessed October 19, 2021.
- American Dental Association. Cancer (Head and Neck). Available at: ada.org/en/member-center/oral-health-topics/cancer-head-and-neck. Accessed October 19, 2021.
- National Cancer Institute. Risk Factors for Cancer. Available at: cancer.gov/about-cancer/causes-prevention/risk. Accessed October 19, 2021.
- Rhodus NL. Oral cancer and precancer: improving outcomes. Compend Contin Educ Dent. 2009;30:486-498.
- Little JW, Miller CS, Rhodus NS. Dental Management of the Medically Compromised Patient. 9th ed. St. Louis: Elsevier; 2018.
- Pai RR, Ongole R. Nurses’ knowledge and education about oral care of cancer patients undergoing chemotherapy and radiation therapy. Indian J Palliat Care. 2015;21:225-230.
- Manne DS. Oncology nurse and dental hygienist: finding success at the crossroad of two professions. Oncol Nurs Forum. 2003;30:913–915.
- Hartnett E. Integrating oral health throughout cancer care. Clin J Oncol Nurs. 2015;19:615–619.
- Daniel BT, Damato KL, Johnson J. Educational issues in oral care. Semin Oncol Nurs. 2004;20:48–52.
- Epstein JB, Parker IR, Epstein MS, Gupta A, Kutis S, Witkowski DM. A survey of National Cancer Institute-designated comprehensive cancer centers’ oral health supportive care practices and resources in the USA. Support Care Cancer. 2007;15:357–362.
- Million RR, Cassisi NJ. Management of Head and Neck: Cancer: A Multidisciplinary Approach. Philadelphia: J.B. Lippincott Co; 2006.
- National Cancer Institute. Drugs Approved for Head and Neck Cancer. Available at: cancer.gov/about-cancer/treatment/drugs/head-neck. Accessed October 19, 2021.
- D’Cruz A, Gupta S, Vaish R, et al. Elective versus therapeutic neck dissection in head and neck cancer treatment. N Engl J Med. 2015;373:2475–2478.
From Dimensions of Dental Hygiene. November 2021;19(11)36-39.





