Developing A Plan of Action
Implementing and consistently updating an ergonomic care program that is based on a problem solving approach can help maintain musculoskeletal health.
Dental hygienists can achieve and maintain optimal health by identifying risk factors that threaten their musculoskeletal health and by identifying, selecting, and implementing interventions to control or eliminate these risk factors.
Lighting, air, and noise all affect the work environment. Insufficient task lighting may cause clinicians to flex forward to achieve better visibility. Glare from the sun emitting through a window may affect visual acuity.
Organizational issues that affect dental hygienists’ satisfaction at work and development of musculoskeletal disorders (MSDs) have recently been addressed. The size of the dental practice was examined relative to job content in a sample of Swedish dental hygienists. The study found that dental hygienists who worked in large practices (>9 hygienists) experienced higher stresses related to role anxiety, treating more patients, and managing business finances than those working in smaller practices. In smaller practices, dental hygienists were able to develop new skills, execute more control over their work, and be supportive to other coworkers.1,2
Scheduling of patients is another organizational factor to consider. The periodontal and deposit complexity of patients may impact the frequency of repetition, amount of force, and awkward posture, as well as the ability to recover from physical stresses. Most dental hygienists treat from five to 14 patients per day. Studies suggest that dental hygienists who practice longer hours and treat more than 11 to 12 patients per day may have a higher prevalence of MSDs than those who treat less than 10 patients per day.3 Further, hygienists who see patients with heavy calculus consistently use higher forces along with little time for rest. Hygienists who work more than 34 hours per week are similarly at higher risk for developing an MSD.3
The management strategies that predict MSD development are dental hygienists’ lack of control over job functions, physical exposure from clinical job tasks, lack of work breaks, and anxiety over role competition with other dental and health care professionals. Researchers concluded that more job control and role clarity are needed to improve working conditions along with opportunities for professional development and supportive relationships with dentists.4,5
Studies show that how clinicians perform their jobs and their level of striving for perfection may also impact their development of MSDs.3,6,7 Those who work with high levels of intensity use higher forces and take less time to rest muscles.8 In fact, those employees who work despite feeling pain and who report the need to perform perfectly at work may be predisposed to developing an MSD when exposed to other ergonomic factors.
Prioritizing Risk Factors
Developing an ergonomic care plan includes prioritizing risk factors and creating strategies to minimize them. Strategies that can be immediately implemented are the most important. Once clinicians develop the ability to continuously observe, self-assess, and evaluate their posture and work processes, minor adjustments can be implemented. Strategies ranked lower include those with cost involved.
A broad conceptual framework was created by the National Research Council9 to examine risk factors for MSDs. The model suggests that biomechanical risk factors probably initiate tissue damage. However, work organizational factors and culture may influence the development of illness.9-11 For example, compensation for services that pay dental hygienists on commission may motivate them to work faster, provide more services, and work longer hours, thus contributing to overuse of muscle groups. The organizational culture of the practice may create an atmosphere that strongly encourages or discourages employees to report the condition early enough to treat it at an acute stage. This impacts the management of the MSD and the stress level of the clinician. Thus, the model implies that factors are interdependent and rarely occur in isolation of one another. It also implies that higher exposures to risks increase the chances of developing an MSD. In a problem solving model of ergonomics, the highest weight is placed on the biomechanical risk factors and recognizing the impact of psychosocial and individual factors.
A Case Study
Liz is 40-years-old and has been practicing dental hygiene in the same general practice for more than 20 years. Liz typically works 4 days a week at two different locations. Liz manages her schedule and determines the length of time needed for each patient, altering the difficulty of cases throughout each day.
Liz contacted a dental hygiene educator and occupational therapist to help identify factors that may be contributing to neck symptoms. An ergonomic job analysis, including a risk factor data collection sheet, body map, and an interview, were completed. 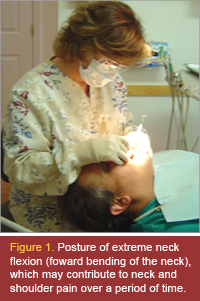
People/worker factors . Liz is married and has two children. Her two children are active with after school activities and weekend sports, which she and her husband attend. Liz’s hobbies include gardening, reading, and swimming.
She has identified muscle tightness and tenderness in the neck and shoulder region on the body map. She goes once a month for a massage, which alleviates her neck symptoms briefly.
Postures. Liz moves to various locations around the patient as needed. She sits with a round shouldered posture. Her neck is positioned in 30°-45° of flexion, shoulders in 30° abduction, and elbows at 90°. Liz occasionally abducts her right arm to 60°–70°. Her forearm moves from mid-position to full pronation. Liz tends to move forward on the seat and does not use the back of the chair for lumbar support. (See Figures 1 and 2).
Workstation design and work process factors. Both dental offices have relatively small rooms with the patient chairs located in the center of each room. Chairs have foot controls for height adjustment, tilt, and swivel. The clinician chairs are adjustable and have adjustable lumbar support. The delivery system is a transthorax/over-the-patient tray set-up with a mobile cart. 
Instrumentation. Liz uses an assortment of instruments varying in texture and size. She uses the ultrasonic scaler on almost every patient and then follows it with hand instrumentation. Her wrist posture is relatively neutral with flexion noted periodically. Liz wears small ambidextrous gloves and does not have any hand, finger, or arm problems.
Environmental factors . Overall lighting seems to be efficient with a window and shade in each room. The overhead light was adjusted to increase the intensity of the task light for better intraoral visibility. Air temperature is consistent throughout the entire office and is comfortable. There are speakers in each room that emit background music. Liz indicates that patients are also encouraged to bring in their own music to listen to via headphones. Environmental factors appear to be sufficient and do not have an impact on biomechanics or psychosocial work factors.
Organizational factors . The lengths of her appointments vary according to her patients’ needs but are typically 30-60 minutes. The hygienist determines the amount of time and interval needed for continuing care appointments based on the patient’s needs. If a patient needs other services, additional time is allotted.
Instruments are sterilized in the office and then sharpened by a service. The hygienist determines which instrument cassettes are to be sent for sharpening. Liz indicates that this is a time saver and alleviates the stress of needing to sharpen instruments. The employer provides a sufficient number of cassettes and instruments. Liz states her employer is very supportive and will provide instruments and equipment upon recommendation from employees. Overall, Liz works in a supportive organizational and team environment.
Symptoms and Strategies
According to the ergonomic assessment and body map, Liz demonstrates symptoms of muscle tightness and tenderness in her neck and shoulders. The cause of the symptoms appears to be primarily from her forward head and round shouldered posture. She holds her neck in excessive flexion and elevates her arms away from her body. Liz also indicated that she has not had a recent eye examination and does not routinely stretch. A dental hygienist who experiences neck pain may adjust the patient’s and clinician’s chair with no alleviation in symptoms. The hygienist needs to further investigate if there are psychosocial stresses causing muscles to tighten or a decrease in visual acuity causing neck flexion.
Developing an ergonomic plan to problem solve her risk factors is the next step. Liz determined the priority for each intervention based on what she could do immediately without a cost factor. An intervention implemented immediately was increasing the intensity of the overhead light for task lighting. Liz indicated that this intervention did increase visibility in the oral cavity but she would still move forward on the clinician’s chair to improve visibility. She commented that she needs to focus on sitting back in the clinician’s chair and make sure that the client’s chair is adjusted to the proper height (to decrease her neck flexion).
Liz was enthusiastic about developing a stretching routine, which can be implemented without cost and is considered both a prevention and rehabilitation strategy for maintaining musculoskeletal health.12 Stretching along with a light aerobic warm-up prepares muscles for active use and decreases the likelihood of a strain or sprain due to overexertion.12,13 Periodic stretching throughout the day reduces the accumulation of static muscle loads and minimizes muscle fatigue. Stretches must be safe, easily graded, and simple to reproduce without supervision. Stretching is just one component of a comprehensive ergonomics program.
Items that were deemed important but could not be implemented imediately included those requiring employer input, such as the purchasing of magnified mirrors and color-coded probes. Liz pointed out that her employer routinely uses magnification loupes. He will not do an examination without them. The cost associated with the loupes is a consideration but Liz will present the loupes to her employer as helping her provide better quality care based on visual acuity and improving her quality of life and career satisfaction.
Three months after the initial ergonomic plan a follow-up evaluation is conducted. Liz had an eye examination and requires reading glasses. The magnified mirror and color coded probes enhance her visual perception, although she still leans forward and does not use the lumbar support. Liz does not suffer with headaches and her neck tenderness and muscle tightness have decreased, although symptoms are intermittent. Liz’s employer has agreed to purchase magnification loupes. Liz has an increased awareness of symptoms and alters her posture and techniques to problem solve ergonomic problems throughout the day.
References
- Ylipaa V, Arnetz BB, Preber H. Factors that affect health and well-being in dental hygienists; a comparison of Swedish dental practices. J Dent Hyg . 1999;73:191-199.
- Ylipaa V, Arnetz BB, Preber H, Benko SS. Determinants of work satisfaction among Swedish dental hygienists. Scand J Caring Sci . 1996;10:247-253.
- Shenkar O, Mann J, Shevach A, Ever-Hadani P, Weiss P. Prevalence and risk factors of upper extremity cumulative trauma disorders in dental hygienists. Work . 1998;11:263-275.
- Ylipaa V, Szuster F, Spencer J, Preber H, Benko SS, Arnetz BB. Health well-being, and musculoskeletal disorders: a comparison between Swedish and Australian dental hygienists. J Dent Hyg . 2002;76:47-57.
- Dong H, Barr A, Loomer P, Rempel D. The effects of finger rest positions on hand muscle load and pinch force in simulated dental hygiene work. J Dent Educ . 2005;69:453-460.
- Atwood MA, Michalak C. The occurrence of cumulative trauma disorders in dental hygienists. Work . 1992;2(4):17-31.
- Osborn JB, Newell KJ, Rudney JD, Stotenberg JL. Musculoskeletal pain among Minnesota dental yygienists. J Dent Hyg. 1990;64132-138.
- Feurstein M. Workstyle: Definition, empirical support, and implications for prevention, evaluation, and rehabilitation of occupational upper-extremity disorders. In: Moon SD, Sauter SL, eds. Beyond Biomechanics: Psychosocial Aspects of Musculoskeletal Disorders In Office Work . Bristol, Pa: Taylor and Francis; 1996:177-206.
- National Research Council. Work-related Musculoskeletal Disorders : A Review of the Evidence. Washington, DC: National Academy Press; 1998.
- Karasek R, Theorell T. Healthy Work: Stress, Productivity and the Reconstruction of Working Life . New York: Basic Books; 1990.
- Smith MJ, Carayon P. Work organization, stress and cumulative trauma disorders. In: Moon SD, Sauter SL, eds. Beyond Biomechanics: Psychosocial Aspects of Musculoskeletal Disorders In Office Work . Bristol, Pa: Taylor and Francis; 1996:23-42.
- Melnik M. Implementing an effective injury prevention process. In: Sanders MJ, ed. Ergonomics and the Management of Musculoskeletal Disorders . Woburn, Ma: Butterworth-Heinemann; 2004.
- Keller K, Corbett J, Nichols D. Repetitive strain injury in computer keyboard users: Pathomechanics and treatment principles in individuals and group intervention. J Hand Ther . 1998;11:9-26.
From Dimensions of Dental Hygiene. Nov 2005;3(11):20, 22-23.

