Oral Pathology
A complete medical, dental, and family history can provide important clues in the oral pathology diagnostic process.
Sometimes historical background is important but additional information is still necessary for a final diagnosis. Let’s use a case study to demonstrate this concept. A patient presents with overall gingivostomatitis, sore throat, fever, malaise, fatigue, and cervical lymphadenopathy. If the patient is 4 years old, the dentist would most likely diagnose the child with herpes simplex virus (HSV) because HSV occurs most commonly in children 6 months to 6 years of age. However, HSV can occur in adults as well. If the patient is 18, initially the dentist would more likely suspect mononucleosis, which is caused by the Epstein Barr virus and most commonly seen in adolescents in their late teens or in young adults. Children also can become infected with mononucleosis through contaminated saliva on fingers, toys, and other items. The systemic and clinical characteristics in both of these viral conditions are similar but the age of the patient is certainly relative to the diagnosis. Additionally with HSV, oral ulcerations are usually present and the condition resolves in 10 to 14 days. In mononucleosis, oral petecchiae, and tonsillitis may be characteristic but this condition takes 4 to 6 weeks to resolve. A blood test is required to confirm the diagnosis for mononucleosis.
Personal Medical History
The patient’s personal medical, and dental history can also play a key role in the final diagnosis. Diabetes is a chronic disorder of carbohydrate metabolism characterized by hyperglycemia. There are many oral complications associated with this condition when the blood glucose is uncontrolled.
This clinical picture of a patient shows hyperplastic, erythematous gingiva (Figure 1). Several areas of periapical disease were noted on her full mouth series and a periodontal charting confirmed significant bone loss. Infection and periodontal disease are clearly related to diabetes. Since the patient indicated that she was diabetic on the medical history, the clinician should definitely be concerned about the link between the patient’s dental findings and an association with her diabetic condition. Clearly, uncontrolled diabetic patients—usually Type I—can exhibit these clinical features. Consultation with the patient’s physician may be extremely helpful in treatment planning, especially if the patient’s diabetes is uncontrolled.
The patient’s occupation can also be helpful in establishing the underlying cause of a condition. For example, a 38-year-old woman went to the dental office for a recare appointment. After reviewing the patient’s medical and dental history, the hygienist began the intra-oral examination. The dental hygienist observed brown discoloration of the fungiform papillae on the dorsal (toward the back) surface of the tongue (Figure 2) and brown extrinsic stain on several of the patient’s teeth. Calling these areas to the attention of the patient, the hygienist attempted to establish a cause by asking a series of questions: Do you smoke?; Do you use a chlorhexidine rinse?; What toothpaste and mouthwash do you use?; Do you brush your tongue?; Do you drink a lot of coffee or tea?; and Have you consumed any particular food or drink on a regular basis that could contribute to these stains? The patient commented that she was a professional wine taster and was currently evaluating red wines at work. She went on to describe the procedure for doing this, explaining that the wine was “snapped” off her palate by her tongue and that there were times when her anterior palate was irritated. At this time, the palatal tissues were found to be within normal limits. Although the stains on the teeth and tongue were not of serious concern, the clinician should be motivated to identify the cause.
|
Figure 1. Hyperplastic erythematous gingiva. |
Figure 2. Discoloration of the fungiform papillae. |
|
Figure 3. Amalgam tattoo. |
Figure 4. Bruxism. |
|
Figure 5. Typical appearance of white sponge nevus in an adult. |
Figure 6. Typical appearance of white sponge nevus in an 11-year-old boy. |
|
Figure 7. Apthous ulcer. |
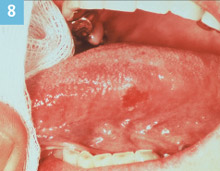
Figure 8. Squamous cell carcinoma. |
| Figure 3 reprinted from Ibsen OAC, Phelan A, Oral Pathology for the Dental Hygienist, 4th ed, Philadelphia: WB Saunders; 2004, with permission from Elsevier. | |
Dental History
The patient’s past dental history should be a significant part of the medical/dental history form. The dental history can tell the hygienist a great deal about patient compliance.
Reviewing these details with the patient during the dental examination can also provide more complete information. Surely, an amalgam tattoo is diagnosed through clinical diagnosis. However, an amalgam tattoo is usually observed on the gingiva or mucosa near a tooth where an amalgam restoration is or had been located. This patient had a blue-grey macule (a stain or a spot) on the labial aspect of alveolar mucosa near the apex of the maxillary central incisor (Figure 3). Clearly, it is an amalgam tattoo. However, there were no amalgam restorations in the area and the maxillary labial anterior is not the most common site for an amalgam tattoo. Additionally, radiographs revealed no radiopaque particles in the area. Questioning the patient provided the answer. The patient said, “I had root canal procedures on my baby tooth.” The tattoo resulted from endodontic procedures involving retrofill on a deciduous tooth. Past dental history is an essential component in the evaluation and examination process.
A mother brings her 7-year-old son to the dental office for a recare visit. The medical history provided by the mother was negative. During the clinical examination, the dental hygienist notes significant bruxism involving the deciduous posterior teeth in the child’s mixed dentition (Figure 4). Upon showing the mother the flat, worn, occlusal surfaces of the child’s teeth, the mother states that her son grinds his teeth at night. Additionally, she says that the grinding is often so loud that she can hear it from another room in the house. The hygienist brings her clinical findings and the mother’s input to the attention of the dentist. Because this condition in a child can be stress related, the dental hygienist felt it was beneficial for the child to receive counseling at school if the mother was receptive. The dentist advised the hygienist to discuss the option with the mother. The mother was most receptive because she was concerned about the child’s habit. Communicating with parents can assist in the optimal health of the patient.
Family History
Family history is another valuable component of historical diagnosis. White sponge nevus (Cannon disease, familial white folded dysplasia) is an autosomal dominant inherited condition (if the gene is inherited, there is a 50% incidence that the condition will appear in the carrier’s offspring) characterized by a white, velvety, corrugated folding of the buccal mucosa that is usually bilateral. It is caused by a defect of the normal mucosal keratin. This mother shows the typical clinical appearance of white sponge nevus (Figure 5). Her 11-year-old son also exhibits characteristics associated with the condition but not with the same degree of folding as seen in the mother (Figure 6). It is a benign condition that requires no treatment but because it is an inherited condition, understanding the family history and the mother’s diagnosis prior to seeing the son is helpful.
The History of the Lesion
The history of the lesion or condition can also be helpful in establishing a diagnosis. Minor apthous ulcer is a condition characterized by discrete, round, or oval ulcerations, under 1 cm in diameter with a yellow fibrin center and an erythema halo. The first episode may occur during adolescence and the patient is often able to associate trauma, stress, or certain foods, ie, citrus, to the onset of the ulcerations. Systemic diseases can also trigger the onset of episodes. The patient also experiences a symptomatic period for 1 to 2 days prior to the eruption of one or several ulcers. The ulcers appear on moveable mucosa, are quite painful, and heal within 6 to 10 days. The diagnosis of this condition is usually made based on how the patient describes the episodes.
This 27-year-old male patient is seen in the dental office for a recare visit (Figure 7). The medical history is reviewed with negative findings. During the oral examination, the hygienist notes a discrete ulceration with a yellow center and an erythamatous boarder in the mucobuccal fold. She asks the patient: “How long has this ulcer been there?” The patient responds: “It has been there several days and it hurts but, eventually, it goes away. I get them every few weeks.” The patient has just described the classic characteristics of minor apthous ulcer. The hygienist questions the patient regarding stress at work, trauma, or foods that he could associate with the onset of the episode. The patient cannot recall anything specific. This patient continued to have many episodes of minor apthous ulcer every few weeks. At one recare, the hygienist decided that perhaps nutritional counseling could provide information relevant to what triggers the onset. The hygienist asked the patient: “What did you have for breakfast?” The patient answered: “Three quarts of orange juice.” Clearly, this excessive citrus intake was the trigger for the frequent episodes of minor apthous ulcer in this patient. The patient was educated concerning foods that could indeed trigger the onset of episodes. The patient decreased his intake of orange juice to 1 quart a day through a straw and his episodes of minor apthous ulcer decreased by more than 50%. Questions, questions, and more questions need to be asked. Even when you know what the diagnosis is, try to figure out what may have caused or contributed to it. This may not always be possible but when appropriate, give it a try.
History of the lesion is not always helpful in the early stages of a lesion or condition. This lesion is indeed a classic! An erythroplakic lesion is observed in the dental office on a recare visit. It is on the left lateral boarder of the tongue, at the junction of the anterior and middle thirds, measuring 5 mm x 7 mm. (Figure 8). The patient has not noticed it and it is asymptomatic. The dental hygienist asks the patient questions related to the lesion. The dentist cannot establish a cause, eg, if the patient had a rough surface on a fractured tooth that could have caused this lesion or if the patient bit his tongue. This lesion was diagnosed as squamous cell carcinoma upon microscopic evaluation. However, the patient would have never seen the oral surgeon for the biopsy if the dentist said, “Let’s watch it until next recare.” These subtle lesions are the challenges. So again, when in doubt, refer it out!

.jpg)
.jpg)
.jpg)