Top-Of-License Dental Hygiene Practice
Dental hygiene scope of practice regulation significantly impacts oral health outcomes in state populations.
Rapid changes in health care systems during the first decades of the 21st century have significantly affected the delivery of oral health care services. In the policy arena, the new emphasis on high-quality, value-based services;1 improvements in diagnostic and treatment technologies and materials; proliferation of information systems and health information exchanges; team-based service delivery models; and integration of primary care and oral health care2 has influenced the deployment of health and oral health workforces. The move toward prevention and management of oral disease and away from the historical treatment paradigm requires the engagement of a comprehensive professional team.3 Dental hygienists are well positioned to contribute to improvements in access to preventive oral health services and, ultimately, to oral health outcomes.3
Numerous economic factors—including the most recent recession, growing proportion of the population with public insurance, and ever-increasing costs associated with dental services delivery—have created pressure to achieve practice efficiencies and improve access to care.4 In addition, the growing diversity and aging of dentists and the United States population, uneven distribution of dentists in certain geographic areas,4 and ongoing concerns about poor oral health outcomes in particular populations are driving change.
The oral health delivery system is reacting to these influences by consolidating dental practices, encouraging support for and funding of dental safety net providers, fostering improvements in population oral health literacy, and urging the establishment of dental homes. There is now growing emphasis on risk assessment to individualize treatment protocols and collaborations with primary health care providers for assessment and referral of patients. These efforts have resulted in not only the development of new oral health workforce models, but also the expansion of roles and functions for existing workforces.
Coincidental with these environmental shifts, interest among policymakers and providers in the impact of evolving roles for dental hygienists on access to oral health care for underserved populations has increased. The traditional perception of the dental hygiene profession as a dental extender—working only under the direction and supervision of dentists—is shifting. Dental hygienists are now more broadly viewed as oral health prevention experts, acting in autonomous roles in a variety of public settings where they often serve as the first point of contact for patients.5 Their roles as not only clinical professionals, but also as case managers and care coordinators are recognized as important in current efforts to increase access to care.
This change in perspective is due, at least in part, to expansions in dental hygiene scope of practice. State legislators and regulators have reduced the levels of required supervision for many dental hygiene services in public health settings. Several states now also permit properly trained dental hygienists to perform basic restorative services.5 Changes in scope of practice have mostly occurred in an incremental fashion and at varying rates in states for more than two decades, with little evaluation of their actual impact on oral health outcomes. While there is pervasive anecdotal evidence and support for the importance and effectiveness of these changes, actual research on their impact is only just emerging.
WHAT THE EVIDENCE SAYS
The Center for Health Workforce Studies (CHWS) at the University at Albany in New York has been studying the evolution of the dental hygiene scope of practice for 15 years. In 2001, CHWS developed a numerical scope of practice scale for dental hygienists, called the Dental Hygiene Professional Practice Index (DHPPI).6 The background research and building of the index was sponsored by the US Health Resources and Services Administration (HRSA).6 Focus groups and interviews were conducted with more than 100 dental hygienists from over 30 states to describe characteristics of practice that were conducive to the full use of dental hygiene competencies and to direct access to dental hygiene services.
The DHPPI scored numerous variables relevant to dental hygiene practice, including the regulatory environment, tasks permitted, levels of required supervision by setting, and reimbursement for services. Each of the variables included carried a weighted score determined by its hypothetical impact on permitting dental hygienists to practice in public health settings under the least restrictive circumstances.6 For instance, if a dental hygienist was permitted to provide preventive services to a patient without a requirement that the patient had first seen a dentist, the score on the DHPPI was higher than if the state required a dental diagnosis and treatment plan before a dental hygiene service. The possible score on the instrument ranged from 0 to 100. The index was scored after examination of the relevant statute and regulation governing dental hygiene practice in each state. In 2001, state scores ranged from 10 in West Virginia to 97 in Colorado (mean score was 43.5), with the majority of states scoring below 50 on the index (Figure 1).5–7
The 2001 scores were used in statistical analysis with population oral health surveillance data from a survey managed by the US Centers for Disease Control and Prevention—the Behavioral Risk Factor Surveillance System (BRFSS)—to determine if there was a relationship between scope of practice and utilization of oral health services by the state’s population. The DHPPI scores in 2001 were positively but not significantly correlated with the percentage of a state’s population that received a prophylaxis by a dentist or dental hygienist within the past year. The higher the score in the state, the more likely was the utilization of preventive services.6
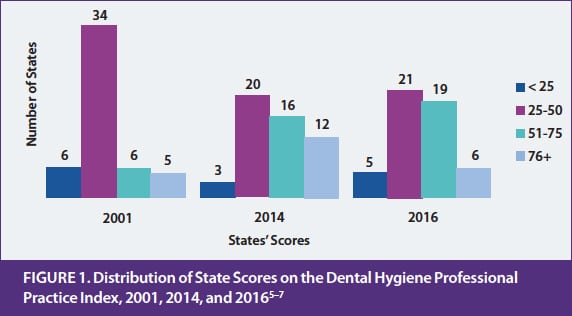 In 2014, CHWS updated the DHPPI scores using the same instrument as in 2001.7 All statutes and regulations in effect in the 50 states and the District of Columbia in 2014 were reviewed and DHPPI scores were revised to reflect legal practice for dental hygienists in that year. State scores ranged from 18 in Mississippi and Alabama to 98 in Maine. A comparison with the 2001 scores showed that the mean score had increased from 43.5 in 2001 to 57.6 in 2014, reflecting an overall increase in the ability of dental hygienists to work under lower levels of supervision in public health settings in many states (Figure 1).
In 2014, CHWS updated the DHPPI scores using the same instrument as in 2001.7 All statutes and regulations in effect in the 50 states and the District of Columbia in 2014 were reviewed and DHPPI scores were revised to reflect legal practice for dental hygienists in that year. State scores ranged from 18 in Mississippi and Alabama to 98 in Maine. A comparison with the 2001 scores showed that the mean score had increased from 43.5 in 2001 to 57.6 in 2014, reflecting an overall increase in the ability of dental hygienists to work under lower levels of supervision in public health settings in many states (Figure 1).
The 2014 scores were used in rigorous statistical analysis to determine if scope of practice impacted oral health outcomes. First, the variables in the index were subjected to exploratory and confirmatory factor analysis to determine if the four categories of variables—regulation, supervision, tasks, and reimbursement—represented a unified construct of scope of practice. Once that was confirmed, the scores were used in multilevel logistic modeling, along with population oral health surveillance data from the BRFSS, while controlling for other individual and state-level variables. The analysis showed that dental hygiene scope of practice was positively and significantly associated with an improved oral health outcome (absence of teeth removed due to decay or disease) in a state’s population.7 As the DHPPI score increased in states, the likelihood of the population having no teeth removed due to decay or disease also increased.
This was an important finding because it suggested that more favorable conditions for dental hygiene practice positively impacted outcomes. This finding was published in 2016.3 There appears to be rising interest among policymakers and stakeholders in the contributions of the dental hygiene profession to improved population oral health outcomes.
One of the findings from the 2014 update was that the variables in the scale, which were originally selected in 2001, no longer adequately reflected conditions for dental hygiene practice. In fact, in 2014, several states had almost progressed to the ideal practice environment (score of 100) that was envisioned when the instrument was built in 2001. Maine, Colorado, Oregon, California, and Washington scored between 94 and 98 on the 2014 update.
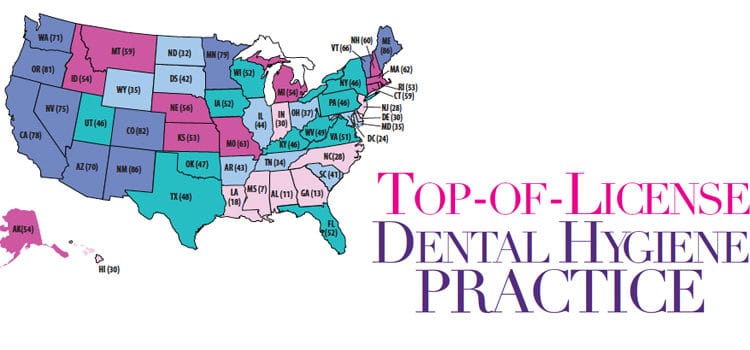
HRSA once again provided the OHWRC with funding to develop a new DHPPI in 2016.5 The new index clustered variables under the same categories as the previous instrument, but the variables were changed: some were revised, some were kept, and new variables were added, while others were eliminated. The scoring was also re-weighted. For instance, independent practice or dental hygiene therapy received a score if the practice was allowed in a state. In 2001, these options were not available (with the exception of Colorado, which permitted unsupervised dental hygiene practice). Examples of new variables include permission to use lasers for debridement or to place atraumatic restorations; this technology and materials were not available when the original scale was devised in 2001. In 2016, Maine and New Mexico scored a high of 86 on the 100 point scale; Mississippi scored a low of 7 (see the map on page 18).
The 2016 DHPPI included variables that measured emerging practice that was not permitted for dental hygienists in all states so it was expected and found that state scores overall were lower in 2016 than in 2014. In the comparative analysis of state scores over time, several states emerged as consistent innovators, meaning that scores were higher in those states in each of the 3 years (2001, 2014, and 2016) than in other states. Maine, Colorado, Washington, Oregon, California, New Mexico, Minnesota, and Nevada all ranked as excellent policy environments for dental hygiene practice. For the details of the comparative analysis and the scoring instrument for each state, view the full 2016 report available at oralhealthworkforce.org.5
POLICY IMPLICATIONS
These DHPPI analyses are useful for state legislators to compare practice in one state with others to evaluate the impact of scope of practice expansions on oral health outcomes. Policymakers, planners, and providers with interest in enabling better access to preventive oral health services for underserved populations will find these results useful for strategic program planning. Researchers are also now using these numerical scores in a variety of economic analyses to describe the impact of the regulation of oral health professions on labor markets and health outcomes.
One important conclusion from these analyses is that positioning dental hygienists to fully utilize their skills and competencies without burdensome supervision in community settings is a strategy that impacts not only the availability of preventive care but also benefits population oral health.
REFERENCES
- Glassman P. Oral health quality improvement in the era of accountability. Available at: wkkf.org/resource-directory/resource/2012/01/pacific-center-for-special-care-report. Accessed September 6, 2017.
- Diringer J, Phipps K, Carsel B. Critical trends affecting the future of dentistry: assessing the shifting landscape. Available at: ada.org/~/media/ADA/Member%20Center/FIles/Escan2013_Diringer_Full.ashx. Accessed September 5, 2017.
- Langelier M, Continelli T, Moore J, Baker B, Surdu S. Expanded scopes of practice for dental hygienists associated with improved oral health outcomes for adults. Health Affairs. 2016;35:2207–2015.
- American Dental Association Health Policy Resources Center. A Profession in Transition: Key Forces Reshaping the Dental Landscape. Available at: ada.org/~/media/ADA/Member%20Center/FIles/Escan2013_ADA_Full.ashx. Accessed September 6, 2017.
- Langelier M, Baker B, Continelli T, Moore J, Maxey H. Development of a new Dental Hygiene Professional Practice Index by state, 2016. Available at: oralhealthworkforce.org/ohwrc-reports-briefs. Accessed September 5, 2017.
- United States Health Resources and Services Administration. The Professional Practice Environment of Dental Hygienists in the Fifty States and the District of Columbia, 2001. Available at: http://docplayer.net/13728482-The-professional-practice-environment-of-dental-hygienists-in-the-fifty-states-and-the-district-of-columbia-2001-april-2004.html. Accessed September 6, 2017.
- Langelier M, Baker B, Continelli T, Moore J. A Dental Hygiene Professional Practice Index by state, 2014. Available at: oralhealthworkforce.org/ohwrc-reports-briefs. Accessed September 6, 2017.
From Perspectives on the Midlevel Practitioner, a supplement to Dimensions of Dental Hygiene. October 2017;4(10):18-21.

