Strategies to Minimize Scatter and Movement Artifacts
Learn how to optimize digital impression accuracy and overcome challenges in intraoral and extraoral scanning for precise dental imaging.

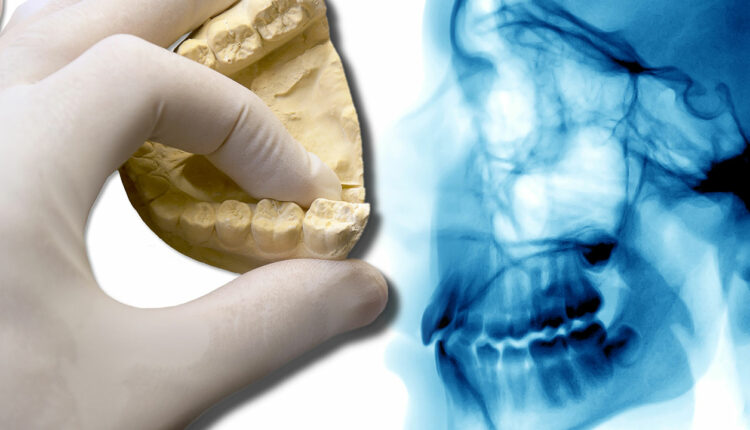
Scatter is a common phenomenon that usually reduces the accuracy of merging data sets and linear measurements. This usually occurs when the X-ray beam strikes high-density objects, such as amalgam restorations, crowns with metal, gutta-percha, posts, sealers, or dental implants, creating a beam-hardening artifact (Figures 1A and 1B).1 Use of cotton rolls to separate maxilla from mandible is a way to minimize the effect of scatter from the opposing arch. Additionally, clinicians can use composite-resin markers on teeth to act as common landmarks in each digital data set for accurate registration.2
Movement artifacts, which usually occur when patients move, can lead to lack of sharpness in images, and therefore difficulty in merging STL and DICOM data sets. Therefore, it is important to avoid these artifacts through proper patient head immobilization and short imaging times.
Conventional or digital impressions transfer information related to teeth, soft tissue and implant position data into stone or virtual models that are utilized for treatment planning and prostheses fabrication. Conventional impressions use impression material translated into stone casts. Digital impressions produce a virtual model in an STL format. This format does not include teeth or mucosa color. Intraoral scans that contain colors are usually in an OBJ geometry format or polygon file format. Although digital impressions are somewhat new, they are becoming more commonly used due to their accuracy and high patient acceptance.3,4 Additionally, clinicians find this method less time consuming compared to conventional impressions in terms of impression material storage, handling and stone pouring.
Cumulative errors in intraoral scans can occur due to the alignment and stitching of the images taken during the scanning process. This tends to occur more frequently in edentulous patients, where the patient lacks distinctive anatomy, and when a larger area is to be scanned, since more images are taken and therefore more images need to be aligned.5 Additional factors to keep in mind when utilizing intraoral scanners are the limited intraoral space for the scanner head, and reflection due to metallic restorations or salivary flow.5 Depending on the scanner technology used, reflection can sometimes be corrected by utilizing a titanium dioxide powder on reflective surfaces.6
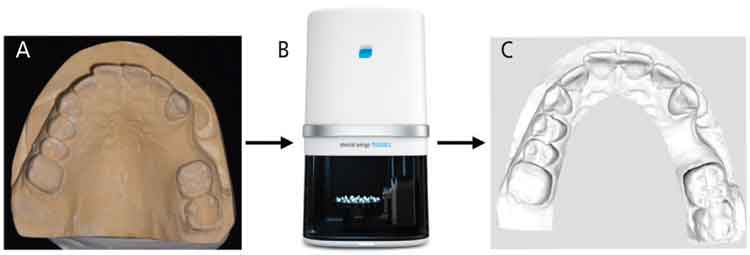
In some cases, the clinician can start with a conventional impression to transfer the details onto a stone cast model and perform an extraoral scan of the stone cast using intraoral scanning devices or dental laboratory scanners (Figures 2A through 2C). Laboratory scanners work by continuously projecting lines or patterns on the stone cast model surface. Reflection and distortion of the projected light are usually detected by one or more cameras that calculate the surface geometry. Inaccuracies with extraoral model scanning usually result from errors that occur during impression-taking and pouring of the stone cast.7
References
- Schulze RK, Berndt D, d’Hoedt B. On cone-beam computed tomography artifacts induced by titanium implants. Clin Oral Implants Res. 2010;21:100–107.
- Hamilton A, Jamjoom F, Doliveux S, Gallucci GO, Friedland B. Radiographic markers for merging virtual data sets. J Prosthet Dent. 2019;122:5–9.
- Papaspyridakos P, Gallucci GO, Chen CJ, et al. Digital versus conventional implant impressions for edentulous patients: accuracy outcomes. Clin Oral Implants Res. 2016;27:465–472.
- Karl M, Graef F, Schubinski P, Taylor T. Effect of intraoral scanning on the passivity of fit of implant-supported fixed dental prostheses. Quintessence Int.2012;43:555–562.
- Gan N, Xiong Y, Jiao T. Accuracy of intraoral digital impressions for whole upper jaws, including full dentitions and palatal soft tissues. PLoS One. 2016;11:e0158800.
- Flügge T, van der Meer WJ, Gonzalez BG, et al. The accuracy of different dental impression techniques for implant-supported dental prostheses: a systematic review and meta-analysis. Clin Oral Implants Res. 2018;29(Suppl 16):374–392.
- Kernen FF. Pre-operative analysis and treatment planning in digital implant dentistry. Forum Implantologicum. 2019;15:8.
This information originally appeared in Alqallaf H, Su FY, Goel A, Lin WS. Utilizing a digital workflow for implant treatment planning. Decisions in Dentistry. 2021;7(5)12-14,16-17.

