Minimally Invasive Soft Tissue Grafting for Mucogingival Defects
This case report showcases the successful use of acellular dermal matrix with a subperiosteal tunneling technique to treat generalized gingival recession and enhance gingival phenotype in a patient with a thin biotype. The procedure achieved complete root coverage, improved tissue health, and provided a viable alternative to autogenous grafting for addressing extensive mucogingival defects.
Mucogingival defects, such as gingival recession and a lack of attached gingiva, pose significant challenges to periodontal health. These conditions not only compromise aesthetics but can also lead to issues such as dentinal hypersensitivity, root caries, and increased vulnerability to inflammation and plaque retention. Soft tissue augmentation, whether through autogenous or non-autogenous grafting techniques, offers effective solutions for managing these defects. This case report highlights the application of acellular dermal matrix (ADM) in conjunction with a subperiosteal tunneling technique to address generalized gingival recession and improve gingival phenotype in a patient with a thin gingival biotype.
CASE REPORT
Figure 1A shows a patient with generalized recession and a thin phenotype extending from teeth #19 to 30. Additionally, there is lack of attached gingiva in the areas of #19, 25, 26, and 30. Teeth #19 and 30 presented with Grade I incipient furcation involvement. The primary goal of the procedure was to gain root coverage, with a secondary goal of gaining attached gingiva. Due to the number of teeth involved, ADM was selected as the graft material of choice.


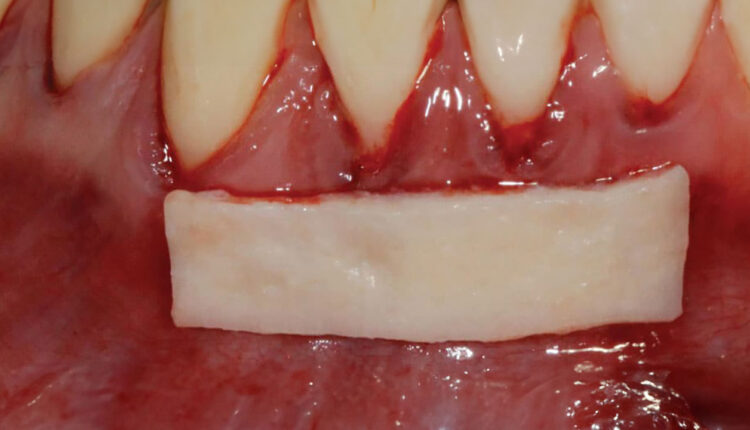
A subperiosteal tunneling technique was used extending from teeth #19 to 30. Care was taken to ensure passive coronal mobility of the tunnel. Figure 1B depicts the tunneled recipient site prior to ADM insertion. Once the ADM was inserted, the tunnel was coronally sutured at the level of the cementoenamel junction with nonresorbable 5-0 polypropylene sutures. A subpapillary continuous sling suturing technique was utilized to suture the tunnel to the graft, with external and internal application of enamel matrix derivatives (Figure 1C). A surgical dressing was not required in this case, as the graft was secured to the overlying soft tissue and remained unexposed.
Post-operative instructions included a soft diet, no brushing and flossing in the area, and utilization of an antibacterial mouthrinse. The sutures were retained for 4 weeks, and oral hygiene instructions were reviewed with the patient at the 4-week post-operative visit. The 3-month follow-up appointment showed complete root coverage in the anterior region, and a wide zone of attached gingiva in the area of teeth #19, 25 and 26 (where previously it was absent). An improvement in the patient’s gingival phenotype was also observed (Figure 1D).


This case demonstrates the effectiveness of acellular dermal matrix combined with the subperiosteal tunneling technique in achieving significant root coverage, enhancing gingival phenotype, and establishing a healthy zone of attached gingiva. The minimally invasive nature of ADM and its predictable outcomes provide a valuable alternative to autogenous grafts for treating extensive mucogingival defects. This approach underscores the importance of selecting appropriate graft materials and techniques tailored to individual patient needs to optimize clinical outcomes and promote long-term periodontal health.
This information originally appeared in Shaikh S, Regahi P. Soft tissue graft alternatives for treating mucogingival defects. Decisions in Dentistry. 2023;9(1):26-29.

