Identifying At-Risk Patients
Much has been written about systemic inflammation and its association with serious comorbid diseases.
Inflammatory Burden
Much has been written about systemic inflammation and its association with serious comorbid diseases. Research has provided an understanding of how genetics can modify inflammatory response and the clinical expression of a number of diseases, including coronary artery disease, Alzheimer’s disease, and periodontitis. Many sources elicit a state of chronic inflammation and contribute to cumulative inflammatory burden. For example, an imbalance in the intake of omega-6 and omega-3 fats; a diet high in red meat, processed foods, refined carbohydrates, and saturated fatty acids; food sensitivities; psychosocial stressors; smoking; lack of quality sleep; environmental toxins; infection; and obesity all have the potential to add to the inflammatory burden, ultimately promoting cardiometabolic risk. There is a strong rationale for implementing a risk assessment model that considers patients’ cumulative inflammatory burden, which may be amplified by obesity and chronic infection from periodontal disease.
Photo Credit: koto_feja / iStock / Getty Images Plus
Fat Cells
In white adipose tissue (fat cells), there is a moderate, but continuous increase in the release of a “cocktail” of inflammatory factors that are systemically dumped. Hence, obesity is widely recognized as a state of low-grade inflammation, fueling the risk for many diseases. Periodontal infection, another source of low-grade inflammation, is also fueled by cytokines that mediate inflammation. If periodontitis is left untreated, ongoing low-grade bacteremia is produced—and, like obesity, it adds to the cumulative inflammatory burden. The greater the burden, the greater the risk and incidence of inflammatory-driven disease.
Photo Credit: Design Cells / iStock / Getty Images Plus

Obesity and Periodontal Diseases
Over the past decade, mounting evidence suggests obesity is also a risk factor for periodontal disease, independent of other factors, such as age, gender, race, and ethnicity. Furthermore, smoking and insulin resistance may help regulate this relationship. In a multicentered, randomized controlled trial that studied the effects of periodontal treatment on secondary prevention of cardiovascular disease, Offenbacher et al demonstrated that obesity may exert such a dominant influence that when obese individuals undergo periodontal therapy, its presence may nullify the effects of periodontal treatment on high-sensitivity C-reactive protein (hs-CRP), a sensitive marker of systemic inflammation. In other words, an obese patient who undergoes therapy for periodontitis may not be able to realize the full systemic benefits of that treatment.
Photo Credit: af_istocker / iStock / Getty Images Plus

Metabolic Syndrome
Since the 2004 paper by Pozharitskaia et al, numerous investigations have looked into the interrelationship between metabolic syndrome (MetS) and periodontitis. MetS is a group of specific metabolic abnormalities that, when combined, imparts a synergistic, enhanced risk for coronary artery disease, stroke, and cardiovascular mortality—an effect that is more pronounced than the individual metabolic components impart alone (eg, hypertension or abdominal obesity). Evidence of the association between MetS and periodontal disease has been consistent enough that a number of researchers have suggested periodontitis should be considered a component of MetS.
Photo Credit: TAGSTOCK1 / iStock / Getty Images Plus

Patient Education
Many individuals have undiagnosed MetS, and thus have not been counseled about the risks inherent to this condition. Given the frequency that patients see their oral health professionals, these clinicians are well positioned to identify patients who have central adiposity (a telling component of MetS) and initiate discussions about cardiometabolic risk. When a patient enters the operatory, the simple task of observing his or her physique can provide valuable clues in identifying whether that individual may be at risk for MetS.
Photo Credit: Aja Koska / E+
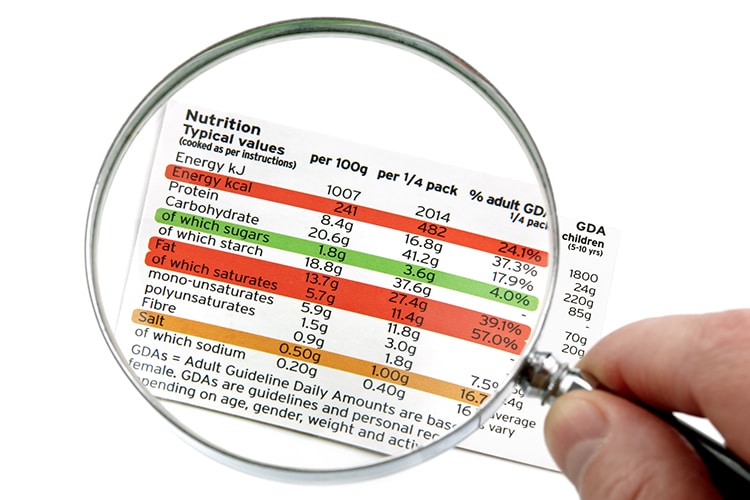
Take Action
Clinicians, health care educators, public health authorities, and policymakers need to be informed of the potential surge in oral health issues that will likely accompany increases in the population of obese individuals, and the concomitant risks associated with inflammatory priming in this population. Accordingly, the development of protocols and clinical tools that will direct care in the individualized management and prevention of oral diseases in patients with metabolic diseases is critical. Close monitoring of the periodontal parameters of obese patients is of obvious importance; however, protocols and clinical tools to assist clinicians in educating patients about the significance of lifestyle modification are essential. These include educational counseling, nutritional assessment, and dietary treatment planning to help reduce a hyperresponsive inflammatory trait, among other clinical measures.

