Diagnostic Screening for Human Immunodeficiency Virus
Multiple factors contribute to the transmission of human immunodeficiency virus (HIV).
Multiple factors contribute to the transmission of human immunodeficiency virus (HIV). Risk based on exposure from sexual behavior is predicated on sexual practices, yet the sexual practice with the greatest risk accounts for a risk probability of 138 in 10,000 exposures. The highest probability for transference of the virus is associated with behaviors in the parenteral group. Blood transfusion, for example, carries the greatest risk. But even needle-sharing (such as in drug use) and percutaneous needlestick carry a significantly higher risk than many subcategories of risk based on sexual behavior.
Photo Credit: Artem_Egorov / iStock / Getty Images Plus

Infection Status
An individual’s HIV infection status is initially determined by his or her CD4 cell count and viral load, which is the amount of HIV present in the blood. Viral load is a measure of HIV genetic material (RNA) in terms of the number of copies of the virus, and is also used to determine the effectiveness of antiretroviral therapy (ART). In terms of sexual practices, the risk of exposure to HIV varies. Transmission risk decreases when the viral load is low and increases when the viral load is high. Laboratories measure viral load in terms of the number of copies of the virus per milliliter of plasma. The use of ART can drop the viral load to an optimal level of between 20 copies/ml to 75 copies/ml, and it can also reduce it to very low or undetectable levels. Although individuals with undetectable or very low viral levels are unlikely to transmit HIV, transmission is still possible.
Photo Credit: porcorex / iStock / Getty Images Plus

Oral Manifestations
Common oral manifestations of HIV include:
- Erythematous candidiasis often presents on the dorsum of the tongue, but is also seen on the hard palate or soft palate. It is red and flat in appearance.
- Pseudomembranous candidiasis presents on the tongue and oral mucosa. It appears as white plaques and leaves a red or bleeding surface after being wiped off.
- Oral hairy leukoplakia is seen on the lateral borders of the tongue, and has a white corrugated appearance that cannot be wiped off.
- Kaposi’s sarcoma appears as a macular or nodular lesion. It may or may not be ulcerated. These lesions can be red or even purple, and older lesions are darker.
Photo Credit: watanyou / iStock / Getty Images Plus
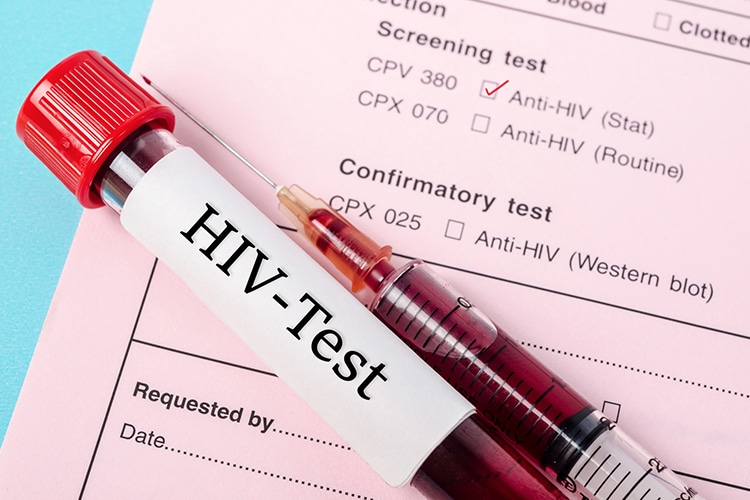
Testing in the Dental Setting
Rapid HIV screening can be completed in the dental office; salivary testing, for example, requires approximately 20 minutes to 30 minutes. Patients should receive a clear explanation that this is a screening tool, and the results are only preliminary. Any patient who tests preliminarily reactive should be linked to the next step in care. The provider should facilitate an appointment with a medical HIV specialist. This potentiality should be included in the informed consent document. If an appointment cannot be made at time of service, the oral health care provider must follow up within 48 hours.
Photo Credit: Gam1983 / iStock / Getty Images Plus
Rapid Testing
Testing for HIV can be done in three ways. A test can detect antibodies, antigens (together with antibodies), or the presence of nucleotides. Nucleotides are the molecular subunits of DNA and RNA, and for the latter include the bases adenine, guanine, uracil, and cytosine. Testing for these elements is complex and best accomplished by a diagnostic lab. Screening performed in dental settings tests for antibodies. This test has an exposure window of up to 3 months. It may not yield results for exposures occurring within the past 3 months because antibodies to HIV are not developed immediately. It may take up to 3 months before blood will show evidence of antibodies to the HIV antigen. If a shorter exposure window is desired, the individual should see a medical provider who can perform a nucleotide test, which has an exposure window of 9 days to 14 days.
Photo Credit: DKosig / iStock / Getty Images Plus

Who Should Get Tested?
The United States Preventive Services Task Force recommends that pregnant women and all individuals between the ages of 15 and 65 be screened for HIV. Patient consent is a consideration. In 2006, the CDC recommended that patients be informed verbally or in writing that HIV testing is part of the general treatment. Having received this information, the patient can refuse the test. According to this recommendation, a specific HIV testing consent is not required. This is a recommendation. Each state has the authority to make its own requirements regarding what defines informed consent, and consent regarding adolescent HIV testing differs between states.

