Treating Periodontitis Systemically
The use of systemic antibiotics can be a helpful adjunct in the treatment of periodontal diseases.
The prevalence of periodontitis and gingivitis is exceedingly high both nationally and around the globe.1,2 According to data from the National Health and Nutrition Examination Survey, nearly half (47%) of American adults have some form of periodontal disease, while 30% have moderate periodontitis, and 8.5% have severe periodontitis.2
Periodontal diseases are active when the host defends against invading putative periodontal pathogens such as Porphyromonas gingivalis (Figure 1), Actinobacillus actinomycetemcomitans (Figure 2), Tannerella forsythensis, and spirochetes (Figure 3).3
While most patients with periodontitis respond well to conventional mechanical therapy (scaling and root planing), others do not or experience a relapse of disease. When treating patients whose disease does not improve with regular maintenance appointments, additional strategies, such as the use of systemic antibiotics, should be implemented.3–11
WHEN TRADITIONAL TREATMENTS ARE NOT EFFECTIVE
Mechanical debridement is not always successful in arresting periodontal diseases due to a number of factors. In some cases, microbial pathogens invade the periodontal connective tissues.3,6,7,12 When this occurs, the mechanical removal of pathogens may need to be supplemented with antibiotics to help fight the bacterial component.3,6–8,13 Pathogens also may reside in anatomical tooth structures that are inaccessible to periodontal instrumentation.3,5,8,10 Complete calculus removal is challenging in teeth with pocket depths ?3 mm and when furcation involvement and abnormal morphology are present.14–16 If the host posts a poor defense against the microbial invaders, mechanical means alone may not stabilize the infection.3
Specific forms of periodontitis that do not respond well to traditional therapy benefit most from systemic antibiotics, including refractory forms of periodontitis, recurrent periodontitis, aggressive periodontitis, and periodontitis associated with diabetes or other immunosuppressive diseases.3–7,11,17–19
The use of antibiotics in the treatment of periodontitis is not new, but local antibiotics are more commonly utilized than systemic therapies. There are several benefits to implementing systemic antibiotics in conjunction with mechanical therapy. First, they are easy to administer compared to locally-applied antibiotics.3 They also reduce the total amount of bacteria and pathogens present in the oral cavity, decreasing the risk of recurrent periodontitis and gingival inflammation. Table 1 provides a list of potential benefits of systemic antibiotic use in patients with periodontitis.3–10,12,13
Some systemic antibiotics attain high levels of concentrations in the infected periodontal epithelial and connective tissues, which helps reduce the total amount of pathogenic bacteria. Additionally, systemic antibiotics are able to target specific pathogens, reducing the number of good bacteria eliminated in the process.3,20 Some types of antibiotics may stimulate the host’s immune response, aiding in the healing process.12,13
RISKS OF SYSTEMIC ANTIBIOTIC THERAPY
When determining whether the use of systemic antibiotics is appropriate, the patient’s medical history must be closely considered as their use is not without risks and limitations. Systemic antibiotics do not offer increased concentrations within gingival crevicular fluid like locally applied antibiotics.3,5,20 The risk of drug interactions also is present, as is gastrointestinal distress.7 Additionally, the incorrect and/or overuse of systemic antibiotics increases the spread of antibiotic-resistant bacteria. Thus, systemic antibiotic regimens should be conservatively prescribed.
When pathogenic bacteria become resistant to antibiotics, they are increasingly difficult to eliminate.3 Systemic antibiotics also rely heavily on the patient adhering to the recommended regimen for taking the drug. If patient compliance is not achieved, the efficacy of treatment suffers, and the risk of furthering antibiotic resistance is increased. This is why clinicians must determine which antibiotics best target the pathogenic bacteria involved before prescribing an antibiotic therapy.3,20
Allergic reaction to antibiotics is another concern. The most commonly used antibiotics, such as penicillins and sulfonamides, are more likely to initiate allergies. Women, older adults, and individuals who have frequently used antibiotics are at greatest risk for allergy development.21
Antibiotics also can increase the number of antibiotic-resistant, benign, and beneficial bacteria present in the oral cavity. The weakening of pathogenic bacteria can result in the overgrowth of the normal microbiota. When this proliferation of bacteria includes Streptoccus mutans, the risk of dental caries may significantly increase.3
MICROBIAL TESTING
There are many variables to recommending a course of treatment for patients with periodontitis. When adding an adjunct to mechanical debridement, such as systemic antibiotic therapy, patients need to understand that the new treatment is not an elixir and effective self-care remains a top priority.3,9 Systemic antibiotics should not be routinely prescribed along with mechanical debridement, but rather a conservative and selective approach is appropriate.3 Microbial testing through outside laboratories can help clinicians determine the specific pathogens involved in an individual’s periodontitis and choose the best antibiotic(s) to target those pathogens.3,22
There are two types of testing provided by laboratories: salivary diagnostics and genetic testing. Microbial testing labs help oral health professionals customize treatment plans for patients with periodontitis by determining which bacterial pathogens are causing periodontal breakdown.22 In a study by Beikler et al,20 results showed that among 776 subjects with periodontitis, 46 different complex pathogen groupings were found. This finding confirms that periodontitis is a multibacterial, complex disease that should be treated with a personalized approach.
Salivary diagnostic labs identify pathogens from the patient’s saliva sample and then recommend antibiotics that may best target the involved microbial pathogens. The antibiotics or treatment modalities recommended in this type of testing are merely suggestions; it is up to the clinician to chart the course of treatment for the patient. Periodontal pathogens vary in their sensitivities to antibiotics, making the recommendation of the best drug challenging. The goal is to administer an antibiotic(s) that specifically targets the pathogenic bacteria while reducing the amount of good bacteria that are eliminated in the process.20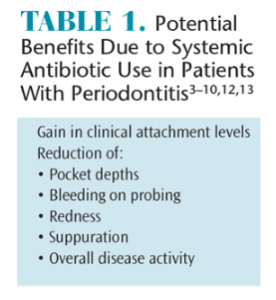
Genetic testing labs provide a one-time screening test that helps ascertain whether a patient is at increased risk of periodontal diseases. This test, which is performed with a saliva sample, looks for a patient’s genetic predisposition to a hyper-response to inflammatory stimuli or interleukin polymorphism.22 This approach may be appropriate for patients with a family history of periodontal diseases or those who present with risk factors. If desired, genetic testing can be performed on any patient to see if he or she is genetically predisposed to periodontal diseases. Genetic testing and microbial testing can both be utilized to determine risk for periodontitis and/or a proper course of therapy. However, they provide different information. Genetic testing is a one-time assessment while microbial testing can be repeated, if needed.
The use of microbial testing is not widespread, mainly due to lack of knowledge about the services offered, increased cost to patients, and the extra steps it creates for clinicians. These tests, however, do offer important information for both patients and clinicians, and their use may increase as techniques evolve.
SEQUENCING OF SYSTEMIC ANTIBIOTIC THERAPY
The American Academy of Periodontology (AAP) recommends a practical approach to the sequencing of periodontal systemic antibiotic therapy. Before beginning initial therapy, the AAP suggests that microbial testing may be justified if systemic antibiotics are indicated. Initial periodontal therapy includes mechanical debridement followed by periodontal surgery to create access, if necessary. Antibiotics may be prescribed based on the clinical need for further treatment, results of the microbial testing, and the patient’s medical status and current medication usage.3
The AAP recommends a periodontal re-evaluation 1 month to 3 months after mechanical therapy. At this point, the treatment team decides whether additional treatment is needed or if the patient can enter a maintenance program. If the periodontitis has progressed or the inflammation has not resolved, a microbial exam of the subgingival microbiota might be needed to determine which periodontal pathogens are remaining. A microbial test may also be able to verify whether the targeted periodontal pathogens have been eliminated and to screen for possible superinfecting organisms. If indicated, systemic antibiotics may then be prescribed.3
After the periodontal infection is resolved, the patient should be put on a customized maintenance program. Supragingivial plaque control may help prevent recolonization by periodontal pathogens. Recurrence of disease symptoms may prompt repeated microbial testing and antibiotic therapy targeted at the specific pathogens found. If periodontitis recurs, mechanical therapy should be recommended in conjunction with the systemic antibiotic regimen.3
CONCLUSION
More research that investigates the efficacy of systemic antibiotics in the treatment of periodontitis is needed. Most of the studies currently available followed patients for only 1 year to 5 years, which is not long enough to determine if the periodontitis resolved. Longer and larger studies are needed to determine whether systemic antibiotics will be needed multiple times throughout a patient’s life and, if so, what effects this will have on antibiotic resistance.3,7,8,13,23 Additional studies are needed to identify the optimal dose for systemic antibiotics in order to reduce the risk of antibiotic resistance.24 Further research also should investigate whether the use of multiple antibiotics is effective in treating a single periodontal infection.3,18
Most studies have shown that the use of systemic antibiotics in addition to mechanical therapy improves outcomes in treating periodontitis.3–19,11,13 With the increasing concern of bacterial resistance, the use of antibiotics should be reserved for patients who do not respond to mechanical therapy alone.3,11 If antibiotics are indicated, the use of microbial testing may be helpful. Treatment of periodontitis should always be customized to patient needs. As new research becomes available, oral health professionals need to stay abreast of what this may add to the body of evidence surrounding periodontal treatment.
REFERENCES
- Eke PI, Dye BA, Wei L, et al. Update on prevalence of periodontitis in adults in the United States: NHANES 2009–2012. J Periodontol. Feb 17, 2015:1-18. Epub ahead of print.
- Eke PI, Dye BA, Wei L, et al. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res. 2012;91:914–920.
- Slots J, Research, Science, and Therapy Committee. Position paper: systemic antibiotics in periodontics. J Periodontol. 2004;75:1553–1565.
- Walker C, Gordon J. The effect of clindamycin on the microbiota associated with refractory periodontitis. J Periodontol. 1990;61:692–698.
- Burrell RC, Walters JD. Distribution of systemic clarithromycin to gingiva. J Periodontol. 2008;79:1712–1718.
- Iskandar I, Walters JD. Clarithromycin accumulation by phagocytes and its effect on killing of Aggregatibacter actinomycetemcomitans. J Periodontol. 2011;82:497–504.
- Pradeep AR, Kathariya R. Clarithromycin, as an adjunct to non surgical periodontal therapy for chronic periodontitis: A double blinded, placebo controlled, randomized clinical trial. Oral Biology. 2011;56:1112–1119.
- Shara R, Medvescek M, Skaleric U. Periodontal disease and diabetes metabolic control: a full-mouth disinfection approach. J Int Acad Periodontol. 2006;8:61–66.
- Serino G, Rosling B, Ramber P, Hellstrom MK, Socransky SS, Lindhe J. The effect of systemic antibiotics in the treatment of patients with recurrent periodontitis. J Clin Periodontal. 2001;28:411–418.
- Rudiger S, Petersilka G, Flemmig TF. Combined systemic and local antimicrobial therapy of periodontal disease in Papillon-Lefevre syndrome. J Clin Periodontol. 1999; 26:847–854.
- Madinier IM, Fosse TB, Hitzig C, Charbit Y, Hannoun LR. Resistance profile survey of 50 periodontal strains of Actinobacillus actinomycetemcomitans. J Periodontol. 1999;70: 888–892.
- Brook I, Lewis MAO, Sandor GKB, Jeffcoat M, Samaranayake LP, Rojas JV. Clindamycin in dentistry: More than just effective prophylaxis for endocarditis? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:550–558.
- Basegmez C, Berber L, Yalcin F. Clinical and biochemical efficacy of minocycline in nonsurgical periodontal therapy: a randomized controlled pilot study. J Clin Pharmacol. 2011;51:915–922.
- Serino G, Rosling B, Ramberg P, Socransky SS, Lindhe J. Initial outcome and long-term effect of surgical and non-surgical treatment of advanced periodontal disease. J Clin Periodontol. 2001;28:910–916.
- Kepic TJ, O’Leary TJ, Kafrawy AH. Total calculus removal: an attainable objective? J Periodontol. 1990;61:16–20.
- Sherman PR, Hutchens LH Jr, Jewson LG, et al. The effectiveness of subgingival scaling and root planing. I. Clinical detection of residual calculus. J Periodontol. 1990;61:3–8.
- Piccolomini R, Catamo G, Bonaventura GD. Bacteriostatic and bactericidal in vitro activities of clarithromycin and erythromycin against periodontopathic Actinobacillus Actinomycetemcomitans. Antimicrobial Agents and Chemotherapy. 1998;42:3000–3001.
- Rams TE, Dujardin S, Sautter JD, Degener JE, Van Winkelhoff AJ. Spiramycin resistance in human periodontitis microbiota. Anaerobe. 2011;17:201–205.
- Grossi SG, Genco RJ. Periodontal disease and diabetes mellitus: a two-way relationship. Ann Periodontol. 1998;3:51–60.
- Beikler T, Prior K, Ehmke B, Flemmig TF. Specific antibiotics in the treatment of periodontitis—a proposed strategy. J Periodontol. 2004;75:169–175.
- Macy E. A practical drug allergy update: what you need to know about drug allergies but did not learn in medical school. Perm J. 2009;13:64–67.
- Miller CS, Foley JD, Bailey AL, et al. Current developments in salivary diagnostics. Biomark Med. 2010;4:171–189.
- Cunha-Cruz J, Hujoel PP, Maupome G, Saver B. Systemic antibiotics and tooth loss in periodontal disease. J Dent Res. 2008;87:871–876.
- Rodvold, KA. Clinical pharmacokinetics of clarithromycin. Clin Pharmacokinet. 1999;37:385–398.
From Dimensions of Dental Hygiene. May 2015;13(3):16–18,21–22.

