
Promoting a Cycle of Remineralization
A variety of strategies, from silver diamine fluoride to chitosan, are available to support enamel health.
Oral health professionals have been trying to educate patients about protecting their teeth from dental caries for decades. However, tooth decay remains the number one disease commonly found in children.1 Frequently, diet and lifestyle choices are to blame for the increased incidence of caries.
Today, caries risk assessment is more focused on preventing caries, not just among children and adolescents, but also adults. Chairside, dental hygienists are educating patients that enamel breakdown can be managed by promoting a cycle of remineralization, allowing the enamel to naturally repair damage caused by cariogenic bacteria.1
Remineralization is the process of replacing lost minerals in the enamel to lower the likelihood of a carious lesion developing. This process happens when calcium and phosphate build on existing crystal remnants of dissolved tooth minerals, allowing the tooth to repair itself.1-4 Repairing the enamel with remineralization can only occur when carbohydrates and acidic pH levels are controlled and limited. Saliva and supplemental products can help aid the remineralization process. Without remineralization, bacteria would constantly attack and penetrate the enamel layer of a tooth.1-4
Patients may first notice a demineralized area in the smile line and inquire about it during the recare appointment. A dental professional should first be able to identify that the demineralization process has occurred, as well as the factors in a patient’s lifestyle that have contributed to the demineralization process.
Theoretically, a tooth may develop a white spot lesion once it has been demineralized. This is because calcium and phosphate minerals have dissolved away from the surface of the enamel. Typically, this white spot appears after numerous episodes of demineralization have been repeated. A noticeable change in enamel appearance may not always be obvious to indicate that demineralization is happening.1-4
Depending on the severity of demineralization, the tooth may exhibit color changes and eventually become soft to the touch with a dental instrument. If the enamel has softened, it no longer has the same mineral composition, and oral cariogenic bacteria can easily penetrate it because the demineralization process has weakened the enamel. To repair the tooth, a dental restoration will be needed to arrest the caries. Early detection of demineralization by dental hygienists is crucial to protect both patients and their dentition — intervening before the enamel surface progresses to cavitation.1,4,5
Caries Risk Assessment
Dental professionals have numerous options when it comes to remineralizing products. To determine a patient’s caries risk, a caries risk assessment is necessary. The caries risk assessment is an interview-like process in which detailed questions are asked to better to understand a patient’s lifestyle and dietary habits.1 Once the risk factors have been identified, education and product recommendations can be tailored to the patient’s specific needs.
When patients are younger than age 5, their parent/caregiver should perform the caries risk assessment with the oral health professional.1 After assessing and diagnosing a patient’s needs, a tailored plan for remineralization that fits the patient’s needs is created. Including the patient in the plan increases compliance and improves the patient’s understanding of caries risk factors and preventive therapies.
Fluoride
Fluoride is one of the most effective approaches for remineralizing the teeth. Fluoride is a naturally occurring element found in mineral sources of both various foods and water. Additionally, supplemental fluoride sources can be applied professionally and over the counter in various topical forms, including gels, foams, varnishes, and liquids.
Fluoride ions bond to calcium and phosphate ions found in saliva to create a fluorapatite crystal. This crystal matrix occurs in the demineralized areas of the tooth, making it better protected against future acid attacks. Additionally, it disrupts the metabolism of cariogenic bacteria, interfering with their ability to produce acid that destroys the enamel layer.
Fluoride is not recommended for anyone who cannot spit out a topical application, such as children younger than age 5.1 For years, many states have used community water fluoridation as a public health measure to address caries management. However, the practice of adding 0.7 milligrams of fluoride per liter of public drinking water has become controversial, with Utah and Florida banning community water fluoridation outright.1-8
Over-the-counter fluorides are dispensed in toothpastes, liquids, or gels at a lower concentration than those used in professionally applied methods. Most over-the-counter dentifrices contain fluoride at 1,000 to 1,100 parts per million (ppm), while the liquids contain 220 ppm.1 High-risk patients may be better served with a prescription fluoride product, which offers higher concentrations — ranging from 900 for a prescription mouthrinse to 22,600 ppm for a prescription varnish — than what is available over the counter.1
Professionally applied fluoride methods offer a range of treatment options, including gels, dentifrices, varnishes, foams, and rinses, enabling clinicians to select the most suitable approach for patients based on their oral health assessment.
Silver
Silver ions, delivered through silver diamine fluoride (SDF) and silver nanoparticles (AgNP), are bactericidal to cariogenic bacteria and support the remineralization of the dentition.1,9 While both therapeutic measures contain silver in their chemical composition, they differ in their other main ingredients, thus, their mechanisms of action for remineralization are slightly different.
SDF is composed of silver ions, fluoride, and ammonia and is applied by a dental professional in a clinic or operatory in a 38% concentration (see sidebar for application instructions).1,9 SDF stops demineralization due to its bacteriostatic properties and then remineralizes any weak areas of the tooth with its fluoride properties.
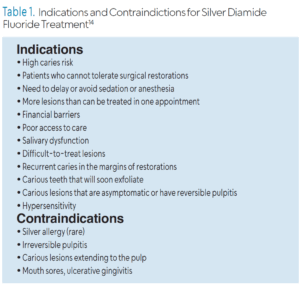
SDF is recommended for patients at high caries risk, especially children who need to bolster their oral health before undergoing more invasive restorative treatment, those who may struggle undergoing traditional dental care, patients covered by government health insurance programs, and older adults.10,11 Table 1 lists indications and contraindications for SDF.
 SDF is highly effective at arresting caries lesions. A review by Jabin et al12 looked at the effectiveness of SDF in caries arrest in the primary dentition. It found four randomized controlled trials that showed 38% SDF application was effective in arresting caries in the primary dentition. In a review by Chan et all3 results showed that SDF (38%) prevented and arrested root caries in older adults.14
SDF is highly effective at arresting caries lesions. A review by Jabin et al12 looked at the effectiveness of SDF in caries arrest in the primary dentition. It found four randomized controlled trials that showed 38% SDF application was effective in arresting caries in the primary dentition. In a review by Chan et all3 results showed that SDF (38%) prevented and arrested root caries in older adults.14
A drawback to SDF is the staining that results after application due to the oxidation of ionic silver.1,9 This can impact patient compliance. However, the use of potassium iodide, potassium fluoride, silver nitrate, and glass ionomer cement in combination with SDF may reduce the resultant discoloration.15
AgNP is made up of nanoscale-sized silver particles that occasionally contain fluoride. AgNP enhances the remineralization process by killing oral pathogens that promote demineralization.9 AgNP is not only bactericidal but also antifungal and antiviral.9 AgNP stops the demineralization process by killing off these microorganisms that would otherwise penetrate the enamel. While a study by Tirupathi et al9 found that SDF and AgNP offer similar remineralization benefits, more research is necessary to support the use of AgNP.
Hydroxyapatite
Hydroxyapatite is a natural mineral found in human bone, but more specifically, it makes up much of the teeth’s enamel. Some consider this mineral substance one of the more natural alternatives for tooth remineralization. Hydroxyapatite is attracted to the demineralized, weak bonds in the enamel matrix and repairs them by bonding with calcium, phosphorus, hydrogen, and oxygen.16,17
Hydroxyapatite can remineralize the enamel on its own; it does not require saliva to activate this process. And because hydroxyapatite is naturally found in the body, it has no toxicity level, making it an effective remineralization treatment option for all populations. As scientists have studied the benefits of hydroxyapatite, remineralization products containing at least 10% nanohydroxyapatite particles are most effective for remineralization.16,17 Furthermore, research has shown that hydroxyapatite cut into nanosized pieces can be absorbed by the tooth’s dentin tubules, not just the enamel.16,17
Casein Phosphopeptide-Amorphous Calcium Phosphate
Derived from the milk protein casein, casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) is used to remineralize tooth enamel. CPP-ACP promotes a saturation of calcium and phosphorus, which helps accelerate the remineralization process with the help of saliva.1,4 The saliva ensures a higher pH concentration, which in turn provides a more stable and steady release of calcium and phosphate ions.1,4 The saturation of these two minerals reduces the risk of demineralization occurring on the enamel.2
CPP-ACP is combined not only to help deliver calcium and fluoride to the tooth, but also to exhibit bacteriostatic properties, which enhance the likelihood of remineralization.2,4,18 CPP-ACP is one of the most widely recognized methods for remineralizing teeth, alongside traditional fluoride, because it can be used in both professional and over-the-counter applications.1 Oral health professionals may prescribe a prescription-strength dentifrice containing CPP-ACP. Additionally, CPP-ACP can be incorporated into mouthrinses, lozenges, chewing gums, and dentifrices. The percentage of CPP-ACP in over-the-counter products is lower than that of prescription-strength products.1,4 CPP-ACP is not recommended for those with dairy allergies. Fluoride can be combined with CPP-ACP to promote an effective measure of remineralization.1,2,4,18
Tricalcium Phosphate
Tricalcium phosphate (TCP) is a calcium phosphate compound used for enamel remineralization. Similar to fluoride, TCP requires calcium and phosphorus in the saliva to initiate remineralization. Studies show that while TCP is effective at remineralization, the presence of fluoride and a more acidic pH level in the oral cavity is required for optimal uptake.2 When TCP is added to a fluoride product, it increases the remineralization uptake compared to using a single fluoride product alone. TCP is found in dentifrices and varnish treatments.1,2,4
Chitosan
Chitosan is derived from the natural carbohydrate complex of chitin, which is found in the skeletons of crustaceans.19 It has both antimicrobial properties and the ability to remineralize enamel by facilitating the binding of calcium and phosphate ions, thereby strengthening the enamel matrix. Chitosan exhibits both bacteriostatic and bactericidal properties against Streptococcus mutans, as well as other oral bacteria.20 Because it deactivates bacteria, chitosan lowers the risk of further demineralization when applied to the tooth. Furthermore, chitosan helps deliver calcium and phosphate ions back into the enamel matrix, supporting the remineralization process.
Chitosan is often distributed in a gel-like substance to be applied to the dentition. Some products contain both chitosan and fluoride to increase the remineralization uptake.19-21 Ongoing research is needed to determine whether patients with shellfish allergies can safely use chitosan-based remineralizing products.19,20
Arginine
Arginine is an amino acid that may be used to remineralize teeth, as it is a component of proteins and peptides. Arginine helps to maintain the mouth’s overall pH level, which weakens plaque biofilm’s ability to penetrate the enamel, and the accumulation of noncariogenic oral bacteria is promoted. Disrupting the bacteria ultimately arrests the demineralization effects because the bacteria cannot penetrate when the pH is not acidic.1,22 By preventing the mouth from becoming excessively acidic, arginine also provides more opportunities for calcium and phosphate ions to accumulate in demineralized areas of the dentition, thereby initiating remineralization.
Arginine is often added to dentifrices to help with the remineralization process. Some dentifrices contain arginine and fluoride to enhance remineralization, as both ingredients work uniquely to remineralize teeth. Research shows that dentifrices containing arginine and fluoride, as opposed to those containing only fluoride, reduce caries and remineralize at a higher rate. 2,4,22 Arginine is commonly found in individual lozenges or dentifrices for patients to use when needed.22
Other Alternatives
Ongoing scientific research continues to reveal alternative therapies that may be utilized in the future to promote remineralization, such as antimicrobial therapies, lasers, ozone, probiotics, theobromine, and herbal compounds. Hopefully with time, dental practitioners and patients will have even more options. However, novel approaches still need further studies to determine the effectiveness and limitations regarding enamel remineralization.2,3,9,23,24
Conclusion
Even when patients believe they have a healthy diet, the process of demineralization and remineralization of tooth enamel is continuously occurring. Oral health professionals should examine a patient’s teeth for areas of demineralization. Once identified, the process of remineralization-demineralization should be explained so patients can make informed choices. During the planning phase of the dental hygiene care process, oral health professionals can help patients decide on what approach to take to remineralize their teeth. A variety of options should be provided and a discussion of which is best suited for individual patient needs is prudent.
References
- Pieren JA, Gadbury-Amyot C. Darby and Walsh Dental Hygiene: Theory and Practice. 6th ed. St. Louis: Elsevier; 2025: 269-285.
- Shah A, Kissel D. Tips to boost remineralization. Dimensions of Dental Hygiene. 2023;21(4):18-21.
- Szalma P, Yoon S. Enhance remineralization. Dimensions of Dental Hygiene. 2013;11(5):42-46.
- Anil AI, Ibraheem WA, Meshni A, et al. Demineralization and remineralization dynamics and dental caries. Available at intechopen.com/chapters/82497. Accessed June 11, 2025.
- Bachand WR, Fraser OL, and Park JL. Maintaining the balance between remineralization and demineralization. Dimensions of Dental Hygiene. 2024;22(1):42-45.
- United States Centers for Disease Control and Prevention. About Community Water Fluoridation. Available at cdc.gov/fluoridation/about/index.html. Accessed June 10, 2025.
- Anderson O. What is the future of community water fluoridation. Available at adanews.ada.org/ada-news/2025/march/what-is-the-future-of-community-water-fluoridation. Accessed June 10, 2025.
- Sequeira R. Fluoride in public water has slashed tooth decay, but some states may end mandates. Available at stateline.org/2024/03/07/fluoride-in-public-water-has-slashed-tooth-decay-but-some-states-may-end-mandates/?utm_source=chatgpt.com. Accessed June 10, 2025.
- Tirupathi S, Svsg N, Rajasekhar S, et al. Comparative cariostatic efficacy of a novel Nano-silver fluoride varnish with 38% silver diamine fluoride varnish a double-blind randomized clinical trial. J Clin Exp Dent. 2019;11:).
- Farrar S, Rainchuso. Current evidence on the efficacy of SDF. Dimensions of Dental Hygiene. 2024;22(1):18-21.
- Crystal YO, Niederman R. Evidence-based dentistry update on silver diamine fluoride. Dent Clin North Am. 2019;63:45-68.
- Jabin Z, Vishnupriya V, Agarwal N, Nasim I, Jain M, Sharma A. Effect of 38% silver diamine fluoride on control of dental caries in primary dentition: a systematic review. J Fam Med Prim Care. 2020;9:1302-1307.
- Chan AKY, Tamrakar M, Jiang CM, Tsang YC, Leun KCM, Chu CH. Clinical evidence for professionally applied fluoride therapy to prevent and arrest dental caries in older adults: A systematic review. J Dent. 2022;125:104273.
- MacLean J. A practical guide to silver diamine fluoride. Available at dimensionsofdentalhygiene.com/article/a-practical-guide-to-silver-diamine-fluoride. Accessed June 10, 1015.
- Stanceviciene E, Miskeviciute-Austin R. Strategies for reducing staining after silver diamine fluoride treatment. Dimensions of Dental Hygiene. 2023;21(8):14-17.
- Erdilek AD, Burke S, Şahin M, et al. Effects of homemade nano-hydroxyapatite and olive oil paste on remineralization of early caries lesions. Trop Health Med Res. 2022;4:1–9.
- Enax J, Fabritius HO, Fabritius-Vilpoux K, et al. Modes of action and clinical efficacy of particulate hydroxyapatite in preventive oral health care – state of the art. Open Dent J. 2019;13:274-287.
- Wang J, Mo, Y, Liu Y. Research progress of CPP-ACP promoting enamel remineralization. International Journal of Frontiers in Medicine. 2022;4(9):12-17.
- Qu S, Ma X, Yu S, Wang R. Chitosan as a biomaterial for the prevention and treatment of dental caries: antibacterial effect, biomimetic mineralization, and drug delivery. Front Bioeng Biotechnol. 2023;11:1234758.
- Abd El-Hack ME, El-Saadony MT, Shafi ME, et al. Antimicrobial and antioxidant properties of chitosan and its derivatives and their applications: A review. Int J Biol Macromol. 2020;1:2726-2744.
- Montoya C, Roldan L, Yu M, et al. Smart dental materials for antimicrobial applications. Bioact Mater. 2002;9:1–19.
- Goyal V, Damle S, Puranick MP, et al. Arginine: A new paradigm in preventative oral care. Int J Clin Pediatr Dent. 2023;16:698-706.
- Farhad F, Kazemi S, Bijani A, et al. Efficacy of theobromine and sodium fluoride solutions for remineralization of initial enamel caries lesions. Front Dent. 2021;18:10.
- Malcangi G, Patano A, Morolla R, et al. Analysis of dental enamel remineralization: A systematic review of technique comparisons. Bioengineering. 2023;10:472.
From Dimensions of Dental Hygiene. July/August 2025; 23(4):14-19.

