
A Comprehensive Approach to Implant Soft Tissue Management
A complex soft tissue defect around a maxillary implant was successfully treated using a modified coronally advanced tunnel technique with a connective tissue graft. By combining precise surgical and prosthetic protocols, clinicians achieved optimal tissue stability and a natural emergence profile, fulfilling the patient’s esthetic goals.
Managing soft tissue recession around dental implants presents a unique challenge, requiring both surgical expertise and prosthetic precision. This case study highlights an advanced approach to correcting a soft tissue defect on a maxillary implant using a carefully staged treatment plan that prioritized tissue health, stability, and esthetics.
Provisional Prosthetic Phase. The implant crown restoration was removed 2 weeks before the surgery. As no parts were available, the already existing abutment was modified to diminish its buccal inclination. Then a properly contoured provisional polymethyl methacrylate (PMMA) crown was fabricated and cemented with temporary cement. This would remain in place for several months to allow the buccal and interproximal soft tissue time to fill the space previously occupied by the existing porcelain crown.
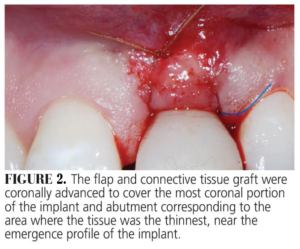
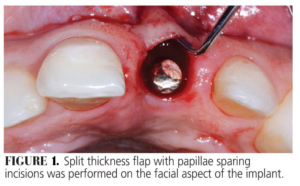 Surgical Protocol. The soft tissue defect was treated with a modified coronally advanced tunnel technique including a connective tissue graft (CTG) harvested from the tuberosity. Following local anesthesia, a poach was created with a modified orban knife on the facial aspect of the implant abutment, preserving the interdental papillae. The flap was raised in a split thickness approach in a coronal apical direction to permit the coronal displacement. Careful dissection was performed to avoid thinning of the buccal flap (Figure 1). The connective tissue was harvested from the tuberosity via a table-top technique and inserted into the pouch. The graft and the flap were stabilized with sling sutures around the cingulum of the temporary crown (Figure 2).
Surgical Protocol. The soft tissue defect was treated with a modified coronally advanced tunnel technique including a connective tissue graft (CTG) harvested from the tuberosity. Following local anesthesia, a poach was created with a modified orban knife on the facial aspect of the implant abutment, preserving the interdental papillae. The flap was raised in a split thickness approach in a coronal apical direction to permit the coronal displacement. Careful dissection was performed to avoid thinning of the buccal flap (Figure 1). The connective tissue was harvested from the tuberosity via a table-top technique and inserted into the pouch. The graft and the flap were stabilized with sling sutures around the cingulum of the temporary crown (Figure 2).
 Post-surgical Infection Control. The patient was prescribed antibiotics (amoxicillin plus clavulanic acid 875/125 mg) starting 1 hour before the surgery and for the next 7 days. In addition, one tablet of Ibuprofen (800 mg) and 8 mg of dexamethasone were given 1 hour before the surgery to mitigate any edema in the surgical area (due to the patient’s position working with clients). The anti-inflammatory medication (ibuprofen, 600 mg) was recommended every 6 hours for 5 days, while the dexamethasone was given as directed for 3 days.
Post-surgical Infection Control. The patient was prescribed antibiotics (amoxicillin plus clavulanic acid 875/125 mg) starting 1 hour before the surgery and for the next 7 days. In addition, one tablet of Ibuprofen (800 mg) and 8 mg of dexamethasone were given 1 hour before the surgery to mitigate any edema in the surgical area (due to the patient’s position working with clients). The anti-inflammatory medication (ibuprofen, 600 mg) was recommended every 6 hours for 5 days, while the dexamethasone was given as directed for 3 days.
 The patient was instructed to avoid brushing the surgical site but to rinse with 0.12 % chlorhexidine solution three times a day. The sutures were removed 3 weeks after the surgery. Plaque control was maintained by continuing the use of chlorhexidine rinse for another 2 weeks. After this period, the patient was instructed to start mechanical plaque control with a ultrasoft surgical brush in a roll technique for another month. The patient was then scheduled for a recare prophylaxis every 3 months.
The patient was instructed to avoid brushing the surgical site but to rinse with 0.12 % chlorhexidine solution three times a day. The sutures were removed 3 weeks after the surgery. Plaque control was maintained by continuing the use of chlorhexidine rinse for another 2 weeks. After this period, the patient was instructed to start mechanical plaque control with a ultrasoft surgical brush in a roll technique for another month. The patient was then scheduled for a recare prophylaxis every 3 months.
Prosthetic Protocol. Five months after the surgery, the patient underwent orthodontic treatment on the maxillary arch only, which lasted for 6 months. The healed surgical site soft tissue was consistent in color and texture with the surrounding area (Figure 3). After completion of the orthodontic treatment, the original abutment was scanned and new hybrid zirconia coping was made to fit over it, transforming it to a hybrid abutment (Figure 4).
 A new PMMA temporary crown was made to fit over this hybrid abutment. The increase in the size of the hybrid zirconia abutment compressed the soft tissue between the implant abutment and the adjacent teeth, providing a new finish line for a provisional crown. At the same time, per the patient’s request, two no-prep veneers were made for the lateral incisors to give his smile more of a square look. The change in the emergence profile, together with the newly resorted contact points, provided support for the interdental papillae.
A new PMMA temporary crown was made to fit over this hybrid abutment. The increase in the size of the hybrid zirconia abutment compressed the soft tissue between the implant abutment and the adjacent teeth, providing a new finish line for a provisional crown. At the same time, per the patient’s request, two no-prep veneers were made for the lateral incisors to give his smile more of a square look. The change in the emergence profile, together with the newly resorted contact points, provided support for the interdental papillae.
Final prosthetic treatment was completed 1 year after the periodontal surgery. A new impression was taken and a new lithium disilicate restoration was used to rehabilitate the patient to the new correct emergence profile. At the patient’s request, a small diastema was created between the two maxillary central incisors (Figure 5).
 Through a combination of surgical refinement, orthodontic alignment, and customized prosthetic restoration, this case demonstrates the power of a multidisciplinary approach in achieving long-term functional and aesthetic success. The patient’s enhanced smile and stable tissue integration underscore the importance of meticulous planning and execution in complex implant cases.
Through a combination of surgical refinement, orthodontic alignment, and customized prosthetic restoration, this case demonstrates the power of a multidisciplinary approach in achieving long-term functional and aesthetic success. The patient’s enhanced smile and stable tissue integration underscore the importance of meticulous planning and execution in complex implant cases.
This information originally appeared in Boeriu S, Hottel TL, Chirla C, Chirla P. Recession defects on a maxillary single tooth implant. Decisions in Dentistry. March 2024;10(2):16-19.

