Supporting Kids’ Smiles
School-based sealant programs are an excellent way to reduce dental caries among the youngest and most vulnerable populations.
Dental or pit and fissure sealants have a significant history in dentistry. Buonocore1 conducted numerous studies during his quest to create a dental sealant that could significantly reduce the prevalence of dental caries among America’s children. Although extensive research documents their efficacy, pit and fissure sealants remain one of the most underused dental materials—most likely due to cost and barriers to accessing dental care.2 The long-standing theory of watching a suspicious area on an occlusal surface on permanent molars is outdated, as the placement of pit and fissure sealants over the area can, at minimum, prevent further progression of the decay.
Because pit and fissure sealants are an evidence-based modality that can significantly reduce the risk of dental caries, school-based sealant programs have been used to treat children in disadvantaged and disenfranchised populations. Many communities and public health agencies across the United States have implemented school-based sealant programs to improve their efforts to prevent dental decay. Successful programs utilize the public health model of screening and surveillance to establish a need within a community for such programs, and also abide by guidelines set forth by the Association of State and Territorial Dental Directors (ASTDD).3
IMPLEMENTING SEALANT PROGRAMS
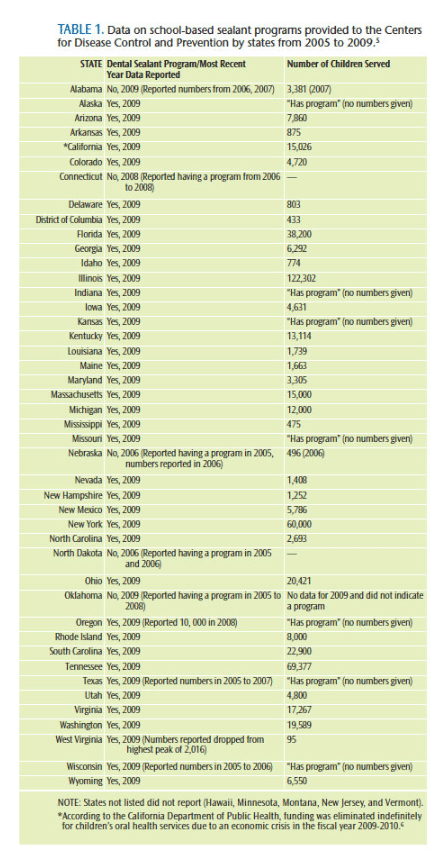 The first school-based sealant program began in Tennessee in the 1970s.4 Today, the exact number of school-based sealant programs operating in the US is unclear. Table 1 provides data on school-based sealant programs provided to the US Centers for Disease Control and Prevention (CDC) from 2005 to 2009.5,6
The first school-based sealant program began in Tennessee in the 1970s.4 Today, the exact number of school-based sealant programs operating in the US is unclear. Table 1 provides data on school-based sealant programs provided to the US Centers for Disease Control and Prevention (CDC) from 2005 to 2009.5,6
Guidelines for implementing school-based programs are not universal. The ASTDD lists a few best practices on its website (astdd.org).7,8 Several states, including Minnesota and Michigan, have published guidelines or manuals on how to start a school-based sealant program. Data collection on such programs is also substandard. According to the CDC, Indiana has a school-based sealant program, but data on the number of children served were not provided. This is problematic because the SEAL Indiana program is very successful. Founded in 2003 by Karen Yoder, RDH, PhD, MSD, SEAL Indiana has completed 24,840 examinations on low-income children throughout the state over the past 10 years. Utilizing Indiana University School of Dentistry faculty and fourth-year dental students, the program has placed sealants on more than 40,469 molar teeth and provided 20,507 fluoride treatments as of December 2013.9 The program is funded by the Indiana State Department of Health, the US Department of Health and Human Services, and corporate sponsors.10 Moi University School of Dentistry in Eldoret, Western Kenya, has modeled its school-based sealant program after SEAL Indiana to help decrease the country’s access-to-care problem, which is severe with only 700 dentists to serve 35 million people.10
States that have submitted updated data, from November 2013 to September 2014, to the CDC include: Arizona, Colorado (conducted a cost study of school-based sealant programs in the state), Georgia, Illinois, Kansas, Michigan, Nevada, New Mexico, Ohio, and Oregon. States looking to establish school-based sealant programs can use this information—which includes the dental director, state oral health plan, and data regarding the number of children seen—as a resource.5
FUNDING PROGRAMS
Several states offer grants that assist with starting or maintaining school-based sealant programs. In Illinois, the Illinois Department of Public Health, Division of Oral Health provides grants for such programs. At the 2007 debut of the State Oral Health Plan, 18 grants were awarded to agencies to serve various counties within the state, and more than 60 grants have been given to local agencies.11 New grantees are awarded funds for equipment (renewal applications do not receive funding for equipment), operational costs, and patient care. Grantees are reimbursed via the state Medicaid provider, DentaQuest, at the Medicaid reimbursement rate, but agencies treating children who are not Medicaid eligible are reimbursed at a state rate, which is less than the Medicaid rate. These reimbursement rates are only applicable to services provided to children in the targeted second and sixth grades. Grantees that treat children in other grades are reimbursed at the state rate, but only if sealants are placed. For example, if the agency serves a number of fourth graders, it will be reimbursed at the state sealant and exam rate. The state reimburses grantees for all second and sixth graders seen (who are ineligible for Medicaid) for exams, regardless of whether sealants are placed. The grantees are reimbursed via Medicaid rates for prophylaxis, fluoride application, exams, and sealant placement for eligible children, regardless of grade.
A unique feature of the school-based sealant program at Southern Illinois University Carbondale is that senior dental hygiene students place the sealants, provide the prophylaxis, and apply fluoride varnish.12 When looking at the cost-effectiveness of school-based sealant programs, utilizing nonpaid students who receive course credit for service-learning experience is one way to reduce the funds needed for salaries. Paid personnel include the supervising staff, which includes one dentist (or more, depending on the volume of children seen during the school year) and at least one licensed dental hygienist, who serves as the program manager and site coordinator. Additional costs to consider include the transportation of the equipment between sites, and supplies. The Illinois school-based sealant program receives free sealant material, fluoride varnish, etchant, and disposable mirrors from Oral Health America’s Smiles Across America® program, which provides funding, supplies, and technical assistance to organizations that provide oral disease prevention services for children who are uninsured and underserved due to issues of poverty—lack of resources, transportation barriers, low literacy, and language diversity. This significantly reduces costs. The program also provides children with an age-appropriate powered toothbrush, which is used in plaque removal during the prophylaxis. With these adjustments in supplies and personnel costs, time and resources are focused on treating children in the school setting. Each year, the program reports a sealant retention rate of more than 90%.
When analyzing cost effectiveness, Werner et al13 compared the school-based sealant program to a ratio used in a nonprofit dental clinic. They determined that the average time spent placing one sealant by one dental hygienist with a dental assistant took 18 minutes. A reduction in the time required for sealant placement to 11 minutes could create significant cost savings.13 In a 5-year review of a Michigan school-based program, Bagramian14 suggested that overall costs of program implementation will decline, as most of the initial funding goes toward mobile equipment that is transported between sites or costs associated with the purchase of a dental van. When sealants are placed on the molar teeth of children considered “high risk,” time, money, and resources are saved by avoiding secondary or more extensive treatment to remove and restore decayed surfaces.15
EXPANDING SEALANT PROGRAM REACH
The Pew Charitable Trusts—which applies a rigorous, analytical approach to improve public policy, inform the public, and invigorate civic life—seeks to expand the number of school-based sealant programs by working with dental public health experts. The organization reported in 2011, “Research has found that school-based programs, where dental hygienists or dentists travel to schools and screen and apply sealants to all students in the optimal age group, are effective in providing sealants. School-based programs are timely, reaching 7- and 8-year olds shortly after their first molars have come in. Bringing services into schools effectively reaches children who normally face significant obstacles in obtaining dental care.”16
 State health departments should partner with dental or dental hygiene schools, and seek corporate funding where available to help reduce the per-sealed tooth cost. Check with local dental professionals who are willing to volunteer their time at the onset of a new program, so that the funds remain focused on getting as many sealants placed on susceptible teeth—particularly among high-risk children whose first and only dental home may be a school-based sealant program.
State health departments should partner with dental or dental hygiene schools, and seek corporate funding where available to help reduce the per-sealed tooth cost. Check with local dental professionals who are willing to volunteer their time at the onset of a new program, so that the funds remain focused on getting as many sealants placed on susceptible teeth—particularly among high-risk children whose first and only dental home may be a school-based sealant program.
REFERENCES
- Buonocore MG. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res. 1955;34:849.
- Beauchamp J, Caufield PW, Crall JJ, et al. Evidence-based clinical recommendations for the use of pit-and-fissure sealants: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2008;139:259.
- Association of State and Territorial Dental Directors. Best Practice Approach Reports: School-based dental sealant programs. Available at: astdd.org/school-based-dental-sealant-programs/#three. Accessed October 21, 2014.
- National Maternal and Child Oral Health Resource Center and Ohio Department of Health. School-Based Dental Sealant Programs. Available at: ohiodentalclinics.com/curricula/sealant/mod1_1_2.html. Accessed October 21, 2014.
- Centers for Disease Control and Prevention. Synopses of State and Territorial Dental Public Health Problems. Available at: apps.nccd.cdc.gov/synopses/index.asp. Accessed October 21, 2014.
- California Department of Public Health. California Children’s Dental Disease Prevention Program. Available at: cdph.ca.gov/programs/Pages/CCDDPP.aspx. Accessed October 21, 2014.
- Association of State and Territorial Dental Directors. State and Community Best Practice Approach Examples. Available at: astdd.org/state-and-community-practice-examples/?bpareport=School-based%20Dental%20Sealant%20Programs. Accessed October 21, 2014.
- Association of State and Territorial Dental Directors. Best Practice Approaches for State and Community Oral Health Programs. Available at: astdd.org/bestpractices/BPASchoolSealantPrograms.pdf. Accessed October 21, 2014.
- Indiana University. Seal Indiana. Available at: dentistry.iu.edu/SealIndiana_Site/about/accomplishments.aspx. Accessed October 21, 2014.
- Indiana University School of Dentistry. Innovation with Impact: Eight years of Seal Indiana. Available at: dentistry.iu.edu/sealindiana_site/_pdf/Seal_Indiana_Anniversary_Report.pdf. Accessed October 21, 2014.
- IFLOSS Coalition. Oral Health Care in Illinois: Comprehensive Care for Children & Families. A Roadmap to the Future: The Illinois Oral Health Plan II. Compendium. 2007 Spring. Available at: ifloss.org/pdf/IOHP2/fullversion.pdf. Accessed October 21, 2014.
- Miller FY. The utilization of dental hygiene students in school-based dental sealant programs. J Dent Hyg. 2005;79:1–8.
- Werner CW, Pereira AC, Eklund SA. Cost-effectiveness study of a school-based sealant program. ASDC J Dent Child. 2000;67:93–97.
- Bagramian RA. A 5-year school-based comprehensive program in Michigan, USA. Community Dent Oral Epidemiol. 1982;10:234–237.
- Quinonez RB, Downs SM, Shugars D, Christensen J, Vann WF. Assessing cost-effectiveness of sealant placement in children. J Public Health Dent. 2005;65:82–89.
- Pew Charitable Trusts. Preventing Dental Disease: Water Fluoridation and Sealant Programs. Available at: pewtrusts.org/en/research-and-analysis/collections/2011/04/06/preventing-dental-disease. Accessed October 21, 2014.
From Dimensions of Dental Hygiene. November 2014;12(11):48,50,52.

