Navigating Dental Care for Patients With Ehlers–Danlos Syndromes
Oral health professionals are well positioned to support proper diagnosis and symptom management in order to improve quality of life for this patient population.
This course was published in the November/December 2025 issue and expires December 2028. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 149
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define Ehlers–Danlos syndrome (EDS).
- Discuss the clinical manifestations of EDS.
- Identify the role of dental hygienists in supporting the health of this patient population.
Ehlers-Danlos syndromes (EDS) are best described as a multifactorial group of connective tissue disorders. EDS are inherited with variations in genes primarily affecting collagen production. Collagen is necessary for many functions in the body, providing support and structure to the joints, tendons, ligaments, organs, blood vessels, bones, and dermis, including providing its elasticity.1,2
Clinical manifestations of EDS include hypermobility of the joints; instability or looseness of the ligaments, tendons, and joint capsules; hyperextensibility and frailty of the skin; delayed wound healing; skin or tissue scarring, and an increase in dislocation and subluxation of joints.2,3 In addition to dermatological and musculoskeletal manifestations, other organs or bodily systems are affected by EDS. Cardiovascular, visual or ocular, gastrointestinal, neurological, psychological, and oral health manifestations have all been well documented.2,4-8
These clinical manifestations can cause concern for dental patients with EDS. Defects in collagen synthesis can lead to an increase in the incidence of subluxation or dislocation of the temporomandibular joint (TMJ), compromised fragile mucosal tissue leading to increased bleeding and delayed wound healing, and elevated risk of periodontal conditions such as early onset periodontitis, recession, bone loss, and tooth mobility due to anomalous composition of the extracellular matrix (ECM).2,3
The ECM provides structural support and a framework for all cells. Improper development of the ECM can also hamper the effect of local anesthesia. Many patients with EDS feel no analgesic effect or a substantially shortened effect after the application of local anesthetics.2,9
Etiology
EDS are a hereditary conditions caused by alterations in the ECM, which directly affects collagen production.1-4 The ECM is a critical component of maintaining tissue homeostasis. The ECM contains macromolecules, including the proteins of collagen, elastin, fibronectin, and laminin, with collagen being a key component and the most abundant. It forms long, fibrous molecules that assemble into organized structures, providing tensile strength and resilience to tissues.2
Collagen fibers are interwoven with other ECM components, creating a complex network that supports and connects cells. When compromised, structural support, cell adhesion and migration, tissue development and repair, regulation of cell signaling, and barrier function of skin and tissues are greatly jeopardized.10 Collagen is a principal protein in the body and represents a key component of the skin, bones, tendons, and ligaments, all of which provide the body with structure and support.2
EDS are broken down into 13 subtypes with each having a unique pathological collagen component. The most common types are hypermobile (hEDS) and classic (cEDS).1 The difference between the two types lies within the fragility of the skin of individuals with cEDS; the skin is more apt to tear or split with negligible trauma, leading to increased scarring.
Hypermobile and classical types have an autosomal dominant inheritance pattern and affect women to a greater degree than men.2,4 Cardiac-valvular EDS and vascular EDS are less common; however, both have potential implications in dentistry. Cardiac-valvular EDS is characterized by irregularities with heart valves, leading to probable valve replacement surgery, while vascular EDS can cause fragility and rupture of blood vessels and organs, gastrointestinal perforation, and aneurysms.11
The genetic etiology of EDS is predominantly unknown, as links between a variety of different genetic mutations in EDS cases have been discussed throughout the literature.2 Diagnosis of EDS is primarily through clinical measures and molecular testing to determine subtype.1 Hypermobile and classical types affect approximately one in 10,000 to one in 15,000 and 20,000, respectively. However, these numbers are often viewed as an underestimation due to the potential of EDS to often share similar characteristics of other heritable connective tissue disorders, such as Marfan syndrome.4 It takes approximately 10 years for a diagnosis of EDS to be determined.12
Systemic Manifestations
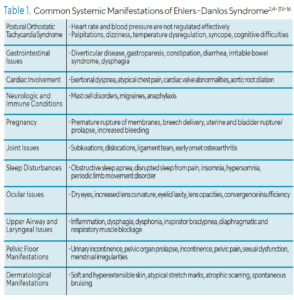
Individuals with EDS may present with significant systemic issues, including neurologic and immune related conditions, pregnancy and surgical-related complications, joint issues, sleep disturbances, ocular issues, respiratory involvement, and pelvic floor manifestations (Table 1, page 38).4,5,6,7,13,14 Some of the more prevalent risk factors associated with EDS are postural orthostatic tachycardia syndrome (POTS), gastrointestinal issues, skin manifestations, and cardiac involvement.2,4,5,6,7,13,15,16
Clinical Features
Hypermobile EDS (hEDS), the most common type of EDS accounting for most cases, is associated with joint hypermobility.1 Distal joints such as hands, wrists, fingers, ankles, and major joints including the hips and shoulder girdle are the most impacted by hEDS. Chronic headaches are also linked to problems with hypermobility of the cervical spine, atlantoaxial junction, meningeal fragility and TMJ dysfunction.17
Complications of joint hypermobility include injury, muscle weakness and tension, proprioceptive problems, and chronic pain.18 Weakness in upper and lower limbs, higher fat percentage, and increased physical impairment are more often seen in those with hEDS than the general population.19 Management of muscle weakness and hypermobility often include physical therapy, low impact exercise, bracing, dietary changes, and pharmacologic treatments.6
EDS can present in the oral cavity in a variety of ways. Characteristics may present differently from person to person, but certain traits are more commonly seen in patients with EDS. Defective collagen impacts teeth, gingiva, nerve tissue, bone, vascularity, and tendons and ligaments.8 This commonly leads to abnormalities in the surrounding oral tissues, dentition, and the TMJ, such as congenitally missing teeth, microdontia, high cusps, pulp stones, stunted roots, or dilacerations. Delayed eruption, hypodontia of permanent teeth, and dentin dysplasia are also common. Other dental pathologies can include crowding and vaulted palate. These abnormalities result from alterations in collagen production and organization.2,4,8
Gingival characteristics can include a lack of attached gingiva and the absence of lingual or inferior labial frenula. These signs may help with diagnosis and early treatment intervention and management of EDS. Increased bleeding and delayed wound healing are common due to the vascular fragility of the tissues and blood vessels. The abnormalities in the collagen lead to insufficient wound healing and the reopening of surgical incisions post-surgery. As a result, dental surgery poses a greater risk of complications. In addition, care must be taken when manipulating the tissues of the oral cavity, as sharp dental instruments or appliances can easily cause trauma to the surrounding tissues.2,4
Because the periodontal ligament is an example of a highly specialized connective tissue, there are periodontal concerns in patients with all forms of EDS. Due to the compromised formation of the ECM, cells cannot maintain homeostasis, leading patients at risk for bacterial pathogenesis and early onset periodontitis.2
Periodontal EDS is associated with a specific gingival phenotype leading to lack of attached gingiva, fragile mucosal tissue, recession, and tooth loss.20 This type can lead to early-onset periodontal diseases. Periodontal EDS manifests as significant progression of periodontal disease despite a lack of deep pockets, bleeding, and bacterial cause. The current major criterion of periodontal EDS is characterized by early onset periodontitis in children and adolescents, as disease progression can affect young people.20 Diagnosis can involve a comprehensive medical history, speaking to a parent or family member, or genetic analysis. As the genetic cause is autosomal dominant, the likelihood of a familial linkage is high.
TMJ dysfunction is another common concern in EDS. The fibrocartilage structures, ligaments, the disc, and retro discal tissues are all composed of collagen. As EDS compromises the development and formation of collagen, this can lead to increased orofacial pain, crepitus, and potential jaw locking.21 Because the joint is directly involved with cervical and pharyngeal functions of the head and neck, it is affected by other comorbidities of EDS, such as craniocervical instability, which is characterized by severe head and neck pain, lower cranial nerve deficits, cervical medullary syndrome and myelopathy.22
Pain and changes to the cervical spine can directly impact TMJ function.8 Those with hypermobility particularly struggle with dislocation and subluxation of joints, including the TMJ. This can lead to displacement of the disc, causing increased pain, bony destruction, and reduced mobility.21 Myofacial pain, headache, disc displacement, degenerative joint disease, arthralgia, and myalgia are all more common in patients with hEDS, which can contribute to reduced quality of life.
Chronic pain is common in EDS and is typically poorly controlled due to factors such as structural changes, neuropathic pain, and impaired proprioception. TMJ disorder contributes to pain and dysfunction in those with EDS, which may lead to overall poor oral health-related quality of life and psychological symptoms such as anxiety and depression.23
Anesthesia resistance is reported more frequently in those with EDS than in the general population. Resistance to local anesthesia is characterized by a failure to achieve expected pain relief from local anesthesia despite the appropriate administration and dose of the anesthetic. Retrospective survey data have demonstrated that overall, those with EDS report insufficiency with local anesthesia at three times the rate of those who do not have EDS.24,25
The mechanism of local anesthesia resistance in EDS is unknown. However, studies have indicated the potential cause as the inability of the ECM to correctly disperse the oxygen, nutrients, and other small molecules leading to complications with achieving profound anesthesia.2 Those with EDS also often have unstable mast cells and higher inflammation, which can affect vasodilation and diffusion of the drug. Finally, those with chronic pain may be experiencing what is referred to as wind-up pain. Prolonged release of neurotransmitters in pain pathways can lead to increased sensitivity and perception of pain to non-painful stimuli as well as hyperalgesia.24
Anesthesia resistance can vary from person to person and may not affect all types of EDS at the same rate. More research is needed as many patients with EDS report painful and traumatic dental experiences that have reduced their oral health-related quality of life. In a 2023 study, 52.6% of patients with hEDS stated they had experienced absence or reduction in effects of local anesthetics.26 Orofacial pain is noted as having the highest impact on quality of life, with many patients with EDS reporting pain often or very often.26 More studies are needed to evaluate the phenomenon of anesthesia resistance in EDS to better understand pain prevention in this population.
Role of the Dental Hygienist
Due to a lack of awareness among the medical community, diagnoses of EDS are often delayed. Physicians are taught to look for the most common explanation rather than the rare diagnosis due to the medical mantra “When you hear hoofbeats, think horses, not zebras.” This is why the zebra has become the symbol for EDS.2 Due to the multisystem nature of EDS, improving health outcomes for the EDS patient starts with interprofessional collaboration, including all clinical practitioners involved in the patient’s care.4 The dental team plays a vital role in understanding, meeting, and managing the needs of patients with EDS.
Dental hygienists must be knowledgeable on how EDS impacts day-to-day life and the challenges EDS present regarding dental treatment and care. A thorough medical history will uncover what type of EDS the patient has, any comorbid conditions, and medications and therapies surrounding current treatment. Asking follow-up questions to better understand the symptoms and concerns of the patient is of the utmost importance. Common concerns include orofacial pain, TMJ disorder, mucosal fragility, dental pain, and local anesthesia resistance.2,6,26 Patients may require referrals to specialists to address their needs.
Patients with EDS may require medication for comorbidities such as POTS; gastrointestinal, neurological, immune, and cardiac problems; sleep disturbances; and chronic pain, with subsequential polypharmacy potentially putting the patient at an increased risk for xerostomia.2,4,16 Additionally, modifications in patient positioning due to lightheadedness or craniocervical instability may be necessary, along with shorter visits or bite blocks for those with TMJ disorders. Discussions about physical therapy, massage, and ways to avoid overworking the TMJ, as well as referrals to specialists who deal with orofacial pain and TMJ disorders, may be indicated.8 Patients with EDS should be assessed for fragile mucosa20 and caution and care should be exercised during treatment to avoid trauma.
Pain management is a major concern of those with EDS in the dental office, as these patients have significantly more difficulty achieving analgesia than the general population.9 Adverse experiences and higher incidences of oral pain may lead many with EDS to develop dental anxiety, creating another potential barrier to care. Discussions with patients about what drugs have worked for them in the past are helpful. Regularly checking in with the patient to ensure that pain is controlled can put the patient at ease. Documentation of what has worked and not worked is also important in ensuring that the patient is comfortable during all future visits. Controlling pain and improving comfort are critical in improving the patient’s oral health quality of life.
Conclusion
EDS is a complex connective tissue disorder. While there is no cure, proper diagnosis and symptom management can improve quality of life. Increasing awareness and research are essential for better treatments, early diagnosis, and greater recognition of the condition. Seeking medical advice is crucial for those experiencing symptoms. The dental hygienist can make a difference in the oral health quality of life for a patient with EDS through education and support.
References
- Caliogna L, Guerrieri V, Annunziata S, et al. Biomarkers for Ehlers-Danlos syndromes: there is a role? Int J Mol Sci. 2021;22:10149.
- Gensemer C, Burks R, Kautz S, Judge DP, Lavallee M, Norris RA. Hypermobile Ehlers‐Danlos syndromes: Complex phenotypes, challenging diagnoses, and poorly understood causes. Dev Dyn. 2020;250:318-344.
- Rosita M, Alima IRN, Auerkari EI. Genetics of Ehlers Danlos syndrome. J Physics. 2021;1943:012092-012092.
- Miklovic T, Sieg VC. Ehlers Danlos syndrome. Available at ncbi.nlm.nih.gov/books/NBK549814/. Accessed October 28, 2025.
- Hamonet C, Brissot R, Amoretti R, Ducret L. Ehlers-Danlos and respiratory function. Clinical data on a cohort of 5,700 patients: oxygen therapy and physical rehabilitation medicine (P.R.M.). Neuroscience and Neurological Surgery. 2020;6(3):1-6.
- Hakim A. Hypermobile Ehlers-Danlos syndrome. Available at ncbi.nlm.nih.gov/books/NBK1279/. Accessed October 28, 2025.
- Fikree A, Chelimsky G, Collins H, Kovacic K, Aziz Q. Gastrointestinal involvement in the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175(1):181-187.
- Mitakides J, Tinkle BT. Oral and mandibular manifestations in the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175:220-225.
- Hakim AJ, Grahame R, Norris P, Hopper C. Local anaesthetic failure in joint hypermobility syndrome. J R Soc Med. 2005;98:84-85.
- Zhou H, Li W, Pan L, et al. Human extracellular matrix (ECM)-like collagen and its bioactivity. Regenerative Biomaterials. February 1, 2024.
- Byers PH. Vascular Ehlers-Danlos syndrome. Available at ncbi.nlm.nih.gov/books/NBK1494/. Accessed October 28, 2025.
- Wang Y, Shiva Jahani, Morel‐Swols D, Kapely A, Rosen A, Irman Forghani. Patient experiences of receiving a diagnosis of hypermobile Ehlers–Danlos syndrome. Am J Med Genet C Semin Med Genet. 2024;194:e63613.
- Cesare AE, Rafer LC, Myler CS, Brennan KB. Anesthetic management for Ehlers-Danlos syndrome, hypermobility type complicated by local anesthetic allergy: a case report. Am J Case Rep. 2019;20:39-42.
- Seneviratne SL, Maitland A, Afrin L. Mast cell disorders in Ehlers-Danlos syndrome. Am J Med Genet C Semin Med Genet. 2017;175:226-236.
- Catala-Pétavy C, Machet L, Georgesco G, Pétavy F, Maruani A, Vaillant L. Contribution of skin biometrology to the diagnosis of the Ehlers-Danlos syndrome in a prospective series of 41 patients. Skin Res Technol. 2009;15:412-417.
- Roma M, Marden CL, De Wandele I, Francomano CA, Rowe PC. Postural tachycardia syndrome and other forms of orthostatic intolerance in Ehlers-Danlos syndrome. Auton Neurosci. 2018;215:89-96.
- Song B, Yeh P, Harrell J. Systemic manifestations of Ehlers-Danlos syndrome. Proc (Bayl Univ Med Cent). 2020;34:49-53.
- Syx D, De Wandele I, Rombaut L, Malfait F. Hypermobility, the Ehlers-Danlos syndromes and chronic pain. Clin Exp Rheumatol. 2017;35 Suppl 107:116-122.
- Coussens M, Lapauw B, Thiberiu B, et al. Muscle strength, muscle mass and physical impairment in women with hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorder. J Musculoskelet Neuronal Interact. 2022;22:5-14.
- Lepperdinger U, Angwin C, Milnes D, et al. Oral characteristics in adult individuals with periodontal Ehlers‐Danlos syndrome. J Clin Periodontol. 2022;49:1244-1252.
- Bech K, Fogh FM, Lauridsen EF, Sonnesen L. Temporomandibular disorders, bite force and osseous changes of the temporomandibular joints in patients with hypermobile Ehlers‐Danlos Syndrome compared to a healthy control group. J Oral Rehabil. 2022;49:872-883.
- Henderson FC, Schubart JR, Narayanan MV, et al. Craniocervical instability in patients with Ehlers-Danlos syndromes: outcomes analysis following occipito-cervical fusion. Neurosurg Rev. 2024;47:27.
- Willich L, Bohner L, Köppe J, Jackowski J, Hanisch M, Oelerich O. Prevalence and quality of temporomandibular disorders, chronic pain and psychological distress in patients with classical and hypermobile Ehlers-Danlos syndrome: an exploratory study. Orphanet J Rare Dis. 2023;18:294.
- Schubart JR, Schaefer E, Janicki P, et al. Resistance to local anesthesia in people with the Ehlers-Danlos Syndromes presenting for dental surgery. J Dent Anesthes Pain Med. 2019;19:261.
- Honoré MB, Lauridsen EF, Sonnesen L. Oro‐dental characteristics in patients with hypermobile Ehlers‐Danlos syndrome compared to a healthy control group. J Oral Rehabil. 2019;46:1055-1064.
- Balke J, Bohner L, Köppe J, Jackowski J, Oelerich O, Hanisch M. Oral health-related quality of life in different subtypes of Ehlers-Danlos syndrome. Intl J Environl Res Public Health. 2023;20:2218-2218.
From Dimensions of Dental Hygiene. November/December 2025; 23(6):36-39.