Expand the Reach of Early Childhood Caries Prevention
Educating parents/caregivers and implementing an interprofessional approach can bolster efforts to improve the oral health of young children.
This course was published in the January 2014 issue and expires Janaury 2017. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define early childhood caries (ECC) and identify those who are at greatest risk.
- Discuss the impediments to establishing a dental home.
- Explain the importance of oral health literacy.
- Identify the role of anticipatory guidance in ECC prevention.
- List the benefits of three state’s interprofessional programs to improve the oral health of children.
Although preventable, early childhood caries (ECC) continues to impact the oral health of infants and preschool-age children across the globe. While advancements in the prevention and treatment of dental caries abound, the most vulnerable children in society remain at great risk. Besides providing dental care services, oral health professionals are charged with educating both children and their parents/caregivers about the importance of oral health and how to achieve and maintain it. In addition, partnering with parents/caregivers and other health care providers to further the reach of caries prevention may prove to be another important strategy in caries prevention. By encouraging the establishment of a dental home, improving parents’/caregivers’ oral health literacy, and implementing an interprofessional approach, oral health professionals can significantly impact the prevalence of ECC.
EARLY CHILDHOOD CARIES
ECC is defined as the presence of one or more decayed, missing due to caries, or filled tooth surfaces among children age 71 months or younger (Figure 1).1 Severe-ECC is the presence of any smooth surface caries in children age 36 months or younger (Figure 2).1
Untreated ECC can cause pain, developmental problems, poor general health, and low self-esteem.2–4 Approximately 31% of American children preschool age and younger experience ECC. This number increases to 40% by kindergarten.5 One in 10 school children have, at one point, experienced oral pain due to ECC, and more than 9% of children in the US under the age of 5 have had “restricted activity days” due to dental pain. In addition, almost 4% of youth have had to refrain from normal daily activities due to severe oral pain.5
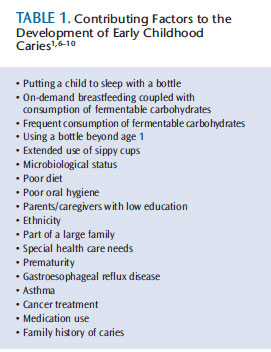
The demographic of children most at risk for ECC include those covered by Medicaid, those who have family members with dental decay, and those with extensive medical histories.5 Table 1 lists some additional contributing factors to the development of ECC.1,6–10 Parents of children with one or more of these risk factors may not understand the serious health consequences of ECC. Educating parents/caregivers, as well as those involved in community outreach, that ECC is preventable through proper diet, good self-care, and regular visits for professional dental care is key.
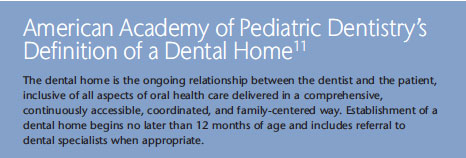
ESTABLISHING A DENTAL
HOME FOR CHILDREN
The American Academy of Pediatric Dentistry (AAPD), the American Academy of Pediatrics, and the American Dental Association (ADA) recommend that a dental home be established for infants prior to their first birthday (AAPD’s definition of a dental home appears above).11–13 Unfortunately, most children in the US do not receive their first dental appointment by age 1 or the eruption of their first tooth. In a study of 340 parents residing in Iowa, 2% reported taking their child to see a dentist by age 1, 11% by age 2, and 31% by age 3.14
 There are many factors that affect children’s ability to receive professional oral health care services. Children from families of low socioeconomic status often have limited access to dental care,15 or the parent/caregiver is unable to take the child to receive professional dental care because he or she cannot afford to miss a day of work or transportation is an issue. Parents’/caregivers’ experience with professional dental care also influences their willingness to ensure the child is treated.16
There are many factors that affect children’s ability to receive professional oral health care services. Children from families of low socioeconomic status often have limited access to dental care,15 or the parent/caregiver is unable to take the child to receive professional dental care because he or she cannot afford to miss a day of work or transportation is an issue. Parents’/caregivers’ experience with professional dental care also influences their willingness to ensure the child is treated.16
Another facet of the access to care problem is that 25% to 50% of general dentists do not treat children age 3 or younger.5 There is also a shortage of pediatric dentists, who typically treat more patients of low socioeconomic status than any other dental speciality.17,18 Approximately 70% of pediatric dentists participate in Medicaid.17 But with only 6,434 pediatric dentists practicing in the US, according to a 2012 ADA practice survey, there remains unmet need.
With the limited number of pediatric dentists practicing in the United States, the provision of oral health treatment for children needs to extend to general dentists and allied oral health professionals.
ORAL HEALTH LITERACY
 The level of parental understanding about dental health has a direct effect on a child’s oral disease status.19 Research also reveals that parents/caregivers are not always informed of the appropriate time to schedule the first dental visit.20 Isong et al21 did find that parents who had a firstborn child with ECC were more likely to make modifications to prevent ECC for subsequent children. This suggests that knowledge is integral to ECC prevention.
The level of parental understanding about dental health has a direct effect on a child’s oral disease status.19 Research also reveals that parents/caregivers are not always informed of the appropriate time to schedule the first dental visit.20 Isong et al21 did find that parents who had a firstborn child with ECC were more likely to make modifications to prevent ECC for subsequent children. This suggests that knowledge is integral to ECC prevention.
Lack of familiarity with the signs and symptoms of ECC may result in parents/caregivers ignoring complaints of oral pain and not seeking necessary dental care. Furthermore, many parents/caregivers believe that baby teeth, because they are temporary, are not as important as primary teeth and may be unaware of the long-term health consequences of ECC.21 Anticipatory guidance is one way to educate parents/caregivers about ECC, its causes, and its effects on oral and systemic health.
ANTICIPATORY GUIDANCE
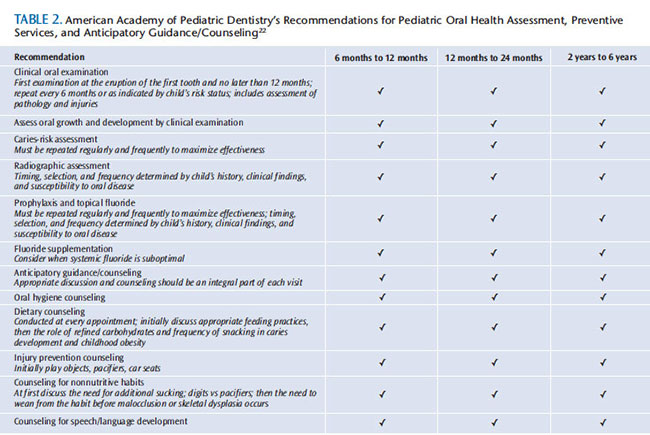
Anticipatory guidance is defined as the “counseling of parents by health providers about developmental changes that will occur in their children between health visits.”20 An anticipatory guidance program for oral health care may include oral health assessments, risk assessments, counseling sessions with parents/caregivers, and preventive treatment (eg, application of topical fluoride).22 The AAPD provides recommendations for pediatric oral health assessment, preventive services, and anticipatory guidance/counseling for children age 6 months to 12 years and older. Table 2 includes the recommendations for children age 6 and younger.23
Research suggests that anticipatory guidance used with first-time parents decreases the rate of severe-ECC.15 In 2007, Plutzer and Spencer15 conducted a study in Australia on 649 expectant mothers. The test group, which included 327 nulliparous women, received education on severe-ECC before giving birth, when their infant was 6-months old, and, finally, when the child was 12-months old. The control group, which included 322 expectant mothers, received no education on severe-ECC. Results showed that the incidence of severe-ECC among the children of the test group was 1.7%, whereas the rate among the children of the control group was 9.6%—a statistically significant difference.15

An Austrian study conducted by Wagner et al24 investigated the effects of an early oral health promotion program on caries prevalence. Immediately following birth, a test group of mothers was visited in the hospital by a qualified dental health educator. They were provided with instruction regarding oral health and oral hygiene, including effective toothbrushing technique and nutritional counseling using motivational interviewing (patient-centered approach that encourages participants to address their ambivalence about implementing positive behavior change) and anticipatory guidance techniques. Five years later, follow-up was conducted on 471 children through a dental examination, half of whose mothers had received the oral health education and half whose mothers had not. The children whose mothers had received the oral health education demonstrated significantly lower caries rates than the children whose mothers had not received any intervention.24
A 2003 American Academy of Pediatrics policy statement recommended that pediatricians include oral health education in their practice, and that they complete an oral health assessment by the time their patients are 6-months old.25 Pediatricians are essential in the early detection of caries because they see children about 12 times during their first 3 years of life.5

Unfortunately, pediatricians do not receive much oral health education in their course of study, and they may be ill prepared to educate their patients’ parents/caregivers. Approximately 70% of medical schools provide less than 4 hours of oral health education in their curriculum, and 10% do not include oral health in their course of study at all.26
Schlute and Druyan27 found that 30% of pediatricians did not know which teeth were more likely to be affected by ECC. In the same study, almost all of the pediatricians surveyed agreed that parents’/caregivers’ lack of understanding about oral health contributed to the prevalence of dental caries, but only 61% provided dietary analysis and 65% offered oral health education.27 Evidence suggests, however, that parents/ caregivers will seek oral health assessments for their children during the first year from their primary care physician as opposed to an oral health professional.21
White spot lesions are the first symptoms of early childhood caries.28 Although they can be effectively treated and the caries process potentially arrested, some pediatricians are unable to recognize white spot lesions, and only 4% of pediatricians apply topical fluoride to the dentition of their pediatric patients.29,30 The exposure to, and application of, fluoride can help remineralize the white spot lesions and hinder further progression into a caries lesion.28
Pediatricians need to provide anticipatory guidance on oral health to parents/caregivers. This includes application of topical fluoride to promote remineralization. The use of anticipatory guidance in oral health promotion within a medical practice setting may improve the oral health status of the patient, as well as the entire family, while decreasing the risk of ECC.31 Pediatricians can improve their knowledge of oral health through continuing education courses and reading literature reviews in order to best help their patients prevent ECC.32
INTERPROFESSIONAL APPROACH
The implementation of an interprofessional approach to caries prevention can make a significant difference in the health of young patients. Some states have already implemented interprofessional programs to reduce ECC. In North Carolina, the Into the Mouth of Babes Program—designed for Medicaid-enrolled patients who do not have access to dental care—provides reimbursement to primary care physicians who provide oral health assessments, apply topical fluoride, and deliver parental counseling on oral health.33 In order to participate in this program, physicians must attend a continuing education course, upon completion of which they are able to describe ECC and its causes; conduct risk assessments for infants and toddlers with regards to dental disease; identify variations of normal; apply fluoride varnish; and, when necessary, counsel parents/caregivers.33 Children with active ECC or those considered at high risk for ECC can then be referred to an oral health professional for further care. To date, this program has proven successful in reducing caries-related treatments for Medicaid-enrolled infants and children.33
Washington state’s county-level program Access to Baby and Childhood Dentistry (ABCD) is designed to increase the number of preventive dental visits within the Medicaid population before age 1. In partnership with the University of Washington School of Dentistry in Seattle, the Washington Dental Service Foundation, Medicaid, public health department, and dental society, dentists involved with the ABCD program receive Medicaid reimbursement for their services upon completion of training geared toward dental treatment for children. The program focuses on outreach, family education, and referral to an ABCD-enrolled dentist. Evidence shows that children in the counties with the ABCD program are 30% more likely to have a preventive dental visit than those residing in nonABCD counties, and the number of dentists treating Medicaid-enrolled children more than doubled.34,35
Columbia University in New York has also developed an interprofessional approach to reduce ECC. My Smile Buddy (MSB) is a tool used to assess risk for ECC, educate parents/caregivers, and create an individualized goal for patients. It was designed to help community health care workers better educate and assess the risk of ECC. An iPad is used to collect data during interviews with parents/caregivers regarding their child’s oral health status, dates of last dental visits, basic dietary questions, and oral health behaviors. After a risk assessment is completed, the parents/caregivers are then educated on the topic, and goals are set for the parents/caregivers and child. Seventy-five percent of the mothers who participated in the program reported that they had been able to accomplish each goal set forth by My Smile Buddy and the health care team.36
CONCLUSION
Addressing the problem of ECC is integral to improving the health of infants and toddlers. Several interprofessional programs have proven successful in increasing access to care and reducing the incidence of ECC. The nationwide expansion and implementation of such programs may help increase awareness and decrease the risk of this common, but preventable childhood disease. Establishing relationships between oral health professionals and their medical colleagues may help foster a more collaborative approach to fighting ECC. Educators may also explore the possibility of creating continuing education courses for medical professionals in their area, so they are up-to-date on the current science and prevention efforts. This interdisciplinary approach, in conjunction with the provision of anticipatory guidance, may help further educate parents/caregivers on the risks of ECC—both short- and long-term—and support ongoing efforts to reduce the incidence of caries among all children.
REFERENCES
- American Academy of Pediatric Dentistry. Definition of Early Childhood Caries. Available at: aapd.org/assets/1/7/D_ECC.pdf. Accessed January 1, 2014.
- Ismail AI. Prevention of early childhood caries. Community Dent Oral Epidemiol. 1998;26(Suppl 1):49–61.
- Department of Health and Human Services. Oral Health In America: A Report of the Surgeon General. Available at: 2.nidcr.nih.gov/ sgr/sgrohweb/home.htm. Accessed December 19, 2013.
- Davies GN. Early childhood caries—a synopsis. Community Dent Oral Epidemiol. 1998;26(Suppl 1):106–116.
- Berg JH, Stapleton FB. Physician and dentist: new initiatives to jointly mitigate early childhood oral disease. Clin Pediatr. 2012;51:531–537.
- Reisine S, Douglass JM. Psychosocial and behavioral issues in early childhood caries. Community Dent Oral Epidemiol. 1998;26(Suppl 1):32–34.
- Tinanoff N. Introduction to early childhood caries conference: Initial description and current understanding. Community Dent Oral Epidemiol. 1998;26(suppl):5-7.
- Erickson PR, Mazhari E. Investigation of the role of human breast milk in caries development. Pediatr Dent. 1992;21:86–90.
- Berkowitz RJ. Causes, treatment and prevention of early childhood caries: a microbiologic perspective. J Can Dent Assoc. 2003;69:304–307.
- Nelson T. Prevent early childhood caries. Dimensions of Dental Hygiene. 2013;11(1):19–22.
- American Academy of Pediatric Dentistry. Definition of Dental Home. Available at: aapd.org/media/Policies_Guidelines/D_DentalHome.pdf. Accessed December 27, 2013.
- American Academy of Pediatrics. Children’s Oral Health. Available at: aap.org/oralhealth. Accessed on December 19, 2013.
- American Dental Association. 2013 Mouth Healthy. Available at: mouthhealthy.org/en/ babies-and-kids. Accessed December 19, 2013.
- Slayton RL, Warren JJ, Levy SM, Kanellis MJ, Islam M. Frequency of reported dental visits and professional fluoride applications in a cohort of children followed from birth to age 3 years. Pediatr Dent. 2002;24:64–68.
- Plutzer K, Spencer AJ. Efficacy of an oral health promotion intervention in the prevention of early childhood caries. Community Dent Oral Epidemiol. 2008;36:335–346.
- Kelly SE, Binkley CJ, Neace WP, Gale BS. Barriers to care-seeking for children’s oral health among low-income caregivers. Am J Public Health. 2005;95:1345–1351.
- American Academy of Pediatric Dentistry. 2012 Legislative Fact Sheet. Available at: aapd.org/assets/1/7/2012_Childrens_Oral_Health_Legislative_Issues.pdf. Accessed December 27, 2013.
- American Academy of Pediatric Dentistry. Membership Statistics. Available at: aapd.org/about/stats. Accessed December 27, 2013.
- Akpabio A, Klausner CP, Inglehart MR. Mothers’/guardians’ knowledge about promoting children’s oral health. J Dent Hyg. 2008;82:12.
- Brickhouse TH. Family oral health education. Gen Dent. 2010;58:212–229.
- Isong IA, Luff D, Perrin JM, Winickoff JP, Ng MW. Parental perspectives of early childhood caries. Clin Pediatr. 2012;51:77–85.
- Ramos-Gomez F, Jue B, Bonta CY. Implementing an infant oral care program.J Calif Dent Assoc. 2002;30:752–761.
- American Academy of Pediatric Dentistry. Recommendations for Pediatric Oral Health Assessment, Preventive Services, and Anticipatory Guidance/Counseling. Available at: aapd.org/assets/1/7/Periodicity-AAPDSchedule.pdf. Accessed January 1, 2014.
- Wagner Y, Greiner S, Heinrich-Weltzien R. Evaluation of an oral health promotion program at the time of birth on dental caries in 5-year-old children in Vorarlberg, Austria. Community Dent Oral Epidemiol. 2013 Sep 4. Epub ahead of print.
- Hale KJ, American Academy of Pediatrics Section on Pediatric Dentistry. Oral health risk assessment timing and establishment of the dental home. Pediatrics. 2003;111:1113–1116.
- Institute of Medicine of the National Academies. Improving access to oral health care for vulnerable and underserved populations. Available at: iom.edu/Reports/2011/ Improving-Access-to-Oral-Health-Care-for-Vulnerable-and-Underserved-Populations.aspx. Accessed December 19, 2013.
- Schulte JR, Druyan ME, Hagen JC. Early childhood tooth decay. Pediatric interventions. Clin Pediatr. 1992;31:727–730.
- Featherstone JD. The science and practice of caries prevention. J Am Dent Assoc. 2000;131:887–899.
- Balaban R, Aguiar CM, da Silva Araujo AC, Dias Filho EB. Knowledge of paediatricians regarding child oral health. Int J Paediatr Dent. 2012;22:286–291.
- Lewis CW, Boulter S, Keels MA, et al. Oral health and pediatricians: results of a national survey. Academic Pediatrics. 2009;9:457–461.
- Ramos-Gomez FJ, Crystal YO, Domejean S, Featherstone JD. Minimal intervention dentistry: part 3. Paediatric dental care–prevention and management protocols using caries risk assessment for infants and young children. Br Dent J. 2012;213:501–508.
- Kagihara LE, Niederhauser VP, Stark M. Assessment, management, and prevention of early childhood caries. J Am Acad Nurse Pract. 2009;21:1–10.
- Rozier RG, Stearns SC, Pahel BT, Quinonez RB, Park J. How a North Carolina program boosted preventive oral health services for low-income children. Health Aff. 2010;29:2278–2285.
- Lewis C, Teeple E, Robertson A, Williams A. Preventive dental care for young, Medicaid-insured children in Washington state. Pediatrics. 2009;124:120–127.
- Nagahama SI, Fuhriman SE, Moore CS, Milgrom P. Evaluation of a dental society-based ABCD program in Washington state. J Am Dent Assoc. 2002;133:1251–1257.
- Chinn C, Levine J, Matos S, Findley S, Edelstein B. An interprofessional collaborative approach in the development of a caries risk assessment mobile tablet application. J Health Care Poor Underserved. 2013;24:1010–1020.
From Dimensions of Dental Hygiene. January 2014;12(1):59–63.



