Pain Management for the Anxious Patient
One of the most important aspects of working with anxious patients is communication.

Pain Management for the Anxious Patient
One of the most important aspects of working with anxious patients is communication. Fearful patients need the oral health professional to hear and understand their concerns, as well as respond in a meaningful way. Rather than a quick dismissive response, the clinician must build trust by listening carefully to understand the nature of the patient’s anxiety and acknowledge his or her concerns. Another helpful tip is to put patients in control by giving them the option of a hand raise on the side opposite the clinician if they need to have a pause in treatment. It is critical to stop if they raise their hand in order to build trust. By taking time to understand patients’ fears and giving them control of the situation, anxiety can be greatly reduced.
Photo Credit: asiseeit / E+
Topical Options for Scaling and Root Planing
There are two combination topical anesthetics commonly used for scaling and root planing. One is a 2.5% lidocaine/2.5% prilocaine combination that is delivered subgingivally using a blunt-tipped applicator. Once delivered into the sulcus, the liquid undergoes a thermosetting process becoming a gel form, and provides approximately 20 minutes of pain control. Onset is approximately 1 minute, and the maximum dose per appointment is five cartridges. The second formulation is a combination of 14% benzocaine, 2% butamben, and 2% tetracaine. It is also applied subgingivally, and will provide 30 minutes to 45 minutes of soft tissue anesthesia. Onset is approximately 30 seconds, and the maximum recommended dose is 0.4 mL.
Photo Credit: Ekaterina79 / iStock / Getty Images Plus

Mouthrinse and Nasal Mist
Dyclonine hydrochloride (HCl) is a ketone-based topical anesthetic rinse that provides widespread topical anesthesia throughout the oral cavity. Dyclonine is not necessarily a good option if periodontal pockets are deep. Because it is delivered as a rinse, subgingival anesthesia is not profound, so this is a better option for a patient with gingivitis or mild periodontitis.
In 2016, the FDA approved an intranasal mist for maxillary anesthesia. The mist is a combination of 3% tetracaine HCl and 0.05% oxymetazoline HCl. The intranasal mist is used to provide anesthesia for teeth #4 to #13 and A through J in patients weighing more than 88 lbs. This provides the clinician with the ability to treat maxillary teeth anterior to the molars with a needleless approach. This method provides pulpal anesthesia, which may be better suited than topical options if the patient has dentin hypersensitivity. Successful pulpal anesthesia is attained more often in the anterior teeth (88%) compared with premolars (60% to 66%), which may be due to the absence of the middle superior alveolar nerve in 28% of patients.
Photo Credit: SweetyMommy / iStock / Getty Images Plus

Communication Is Key
Communication prior to and during the injection can reduce anxiety about the injection. The clinician should maintain a calm and quiet voice, and should structure any communication about possible discomfort using a positive sentence structure. For patients with severe anxiety, behavioral management techniques can be helpful. These include deep breathing, progressive relaxation, and guided imagery, performed with the patient’s eyes closed.
Photo Credit: Cecilie_Arcurs / E+

Distraction and Speed
Distraction methods are also helpful in delivering a comfortable injection. Vibration has been suggested as an effective method of distraction. There are dental syringe vibrators and vibrating retractors available to make this distraction technique simple. Some of the discomfort associated with local anesthetic injection is due to the rate at which the clinician delivers the anesthetic. If the speed of the anesthetic delivery is too fast, then the injection burns due to the pH difference between the local anesthetic agent (acidic) and the body tissues (close to neutral). Computer-controlled local anesthesia delivery (CCLAD) devices can reduce patient discomfort during injections. These devices use a computer to control the rate at which the anesthetic agent is injected, and have demonstrated improved patient comfort compared to a traditional syringe.
Photo Credit: ayo888 / iStock / Getty Images Plus

Buffering
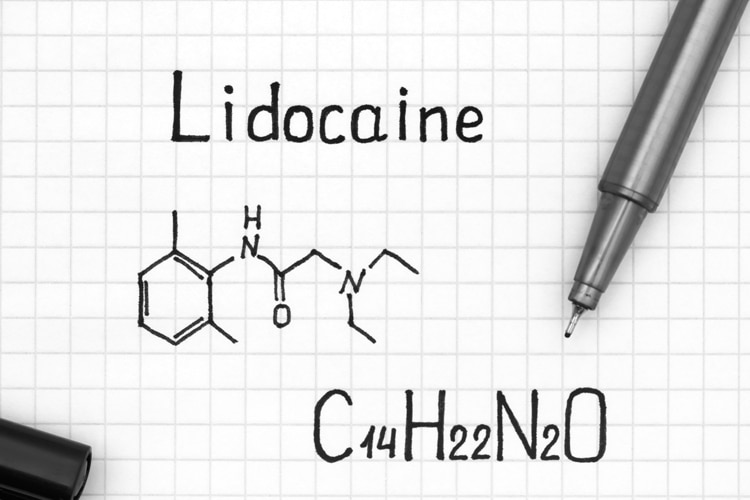
Buffering can reduce the pain of an injection, as the addition of sodium bicarbonate to the anesthetic solution raises the acidic pH to a more physiologic range. Buffering systems include buffering solutions and mixing devices. With one system, the clinician uses a mixing pen to add sodium bicarbonate to a traditional dental cartridge. Another system uses large vials of lidocaine and sodium bicarbonate that are mixed in a cartridge contained inside a dispenser.
Photo Credit: diego_cervo / iStock / Getty Images Plus

Nitrous Oxide
Some patients may be candidates for sedation. In many states, dental hygienists can administer nitrous oxide/oxygen sedation (N2O/O2). This method is effective for patients with mild to moderate anxiety. Nitrous oxide also has the ability to increase the pain threshold, which can be very effective during the administration of local anesthesia injections. Patients who are truly phobic often do not benefit from N2O/O2. Correct administration technique is critical to a positive experience. Titration to the appropriate baseline concentration of nitrous oxide is the best approach to ensure anxiety reduction without progressing to oversedation.


Great articles. This goes to Junk and not to my email. I don’t know why!!!!