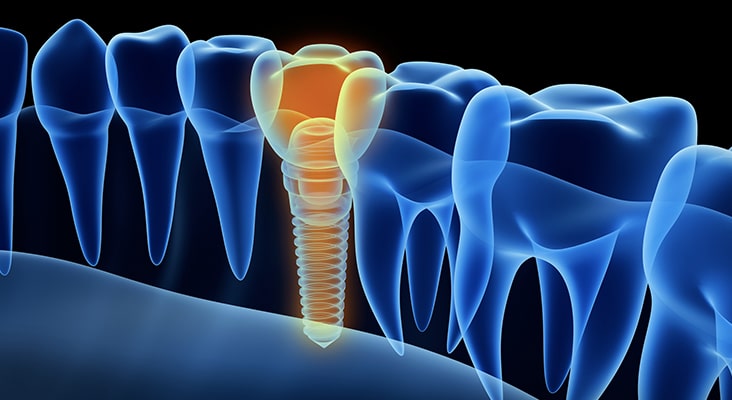
Oral Hygiene for Implants
While current guidelines for maintaining implant-supported prosthetics are poorly defined, periodic evaluation by a dental professional is suggested for the preservation of healthy peri-implant tissues.

Dental Hygienists Lead the Charge
While current guidelines for maintaining implant-supported prosthetics are poorly defined, periodic evaluation by a dental professional is suggested for the preservation of healthy peri-implant tissues. With dental hygienists at the forefront of oral disease prevention and detection, knowing how to assess and treat peri-implant diseases is part of the dental hygiene standard of care. Complicating factors in this endeavor include the multifaceted structure of implant-supported prostheses and anatomical challenges that can make plaque control difficult.
Photo Credit: BakiBG / iStock / Getty Images Plus

Type of Implants
A removable prosthesis or overdenture includes a removable full set of prosthetic teeth that may be supported by two implants to four implants, depending on its location (maxilla or mandible). For example, an overdenture supported by two implants in the mandible snaps onto the supporting implants. These attachments have male and female components: one attaches to the implant body, and the other attaches to the inside of the overdenture. Depending on the design, the components can be magnets, clips, locators, or ball attachments. The components located on the inside of the overdenture can be removed and/or changed as needed.Hybrid dentures, also known as fixed detachable dentures, are a mixed design that combine the benefits of a fixed replacement with the advantages of a removable denture. This prosthesis is a cross between a traditional denture and a fixed bridge that does not require daily removal because it is screw retained into the implants. This means it can be detached by the dentist. Depending on the shape and size of the jaw, this prosthesis may be supported by four implants to eight implants.
Photo Credit: george tsartsianidis / iStock / Getty Images Plus

Attachment Apparatuses
Various methods are used to attach hybrid dentures to implants. One approach connects the dental implants to the denture through abutments that are screwed into a metal framework known as an implant bar. The bar is screwed into the dental implants, and the prosthesis is screwed into the implant bar. Other examples of hybrid dentures are the “all-on-four” and fixed dentures supported by five to six implants. These designs typically have a metal substructure that is attached to the implants. “All-on-four” is a fixed denture mounted on four implants. This is a minimal design that may be appropriate for patients with less-than-optimal bone levels. The prosthesis is screwed directly into the implant abutments. When five implants to six implants are used, an overdenture with a metal substructure is fixed to the implant extensions. Implant-supported overdentures with six implants provide optimum support, making this an ideal option for hybrid dentures.
Photo Credit: RossHelen / iStock / Getty Images Plus

Fixed Implant-Supported Bridge
Another option for the edentulous patient is a fixed implant-supported bridge, which is a conventional bridge made of porcelain or other ceramic material and supported by six implants to eight implants. A bridge design is suitable for patients with minimal or no loss of bone and gingiva, as the bridge only replaces the crown aspect (ie, there is no denture base). Fixed implant-supported bridges closely resemble the look and feel of natural dentition. The fixed implant-supported bridge is customized for each case and cannot be removed by the patient. Extensions are attached to the dental implants, and the bridge is fixed onto the implants.
Photo Credit: CreVis2 / iStock / Getty Images Plus

Oral Hygiene Challenges
Clinically, when performing implant hygiene and assessment, the critical areas include the surfaces around the attachments for fixed or hybrid overdentures, and the gingiva/implant interface of implant-supported fixed bridges. Often, anatomical challenges may be present that make oral hygiene care difficult for the patient and clinician. With removable implant-supported dentures, the implant superstructures are easily accessible once the denture is removed. The prosthesis should be evaluated for retention, surface damage, and cleanliness. The soft tissues of the oral cavity should be examined for signs of inflammation, including denture irritation and peri-implant diseases around the attachments. Patients should be advised to remove the denture overnight, or at least for several hours each day, to prevent denture stomatitis. Fixed hybrid overdentures cannot be removed by the patient, which limits access to the implant superstructures and restoration surfaces. Because they cannot be removed, hybrid dentures are designed to allow space between the prosthesis and jawbone. This provides access underneath the denture for ease of cleaning. A potential downside to this design is the risk of food impaction and inflammation.
Photo Credit: GuidoVrola / iStock / Getty Images Plus

Buccal and Labial Flanges
Another anatomical challenge of fixed dentures is presented by buccal and labial flanges. Denture flanges extend into the vestibule areas to help support the lips and cheeks—although this makes the buccal and labial surfaces of the implant superstructures inaccessible for hygiene care.
Photo Credit: ugurhan / iStock / Getty Images Plus

Biofilm Management
A correct fit and complete seating of implant components—as well as superstructures—must be ensured to minimize niches that promote biofilm adherence. With a fixed conventional full-arch bridge, anatomical challenges present when the pontic’s emergence profile does not mimic the natural tooth (emergence profile describes the contour of a crown as it emerges from the gingiva). Poorly shaped implant crowns can create inaccessible undercuts; in turn, this results in embrasure spaces and abutments that are unreachable from all surfaces. An improper emergence profile can also create embrasure spaces that allow food impaction, or small, tight embrasures that are difficult to access with oral hygiene aids. Clinicians should be aware that implant placement at a submucosal level (to hide crown margins) may raise the risk of infection. This can compromise professional and self-care efforts to remove biofilm and food debris, making the patient vulnerable to peri-implant infections.
Photo Credit: ayo888 / iStock / Getty Images Plus
Importance of Self-Care
In all implant cases, effective self-care is imperative to successful long-term outcomes—and this is particularly true for patients with full-arch, implant-supported prostheses. Research indicates that 3 weeks of ineffective or poor oral hygiene practice will contribute to peri-implant mucositis. Professional plaque control should include regular oral hygiene instructions tailored to a patient’s individual needs. Appropriate interproximal cleaning methods should be recommended, such as the use of interdental brushes with plastic-coated wires, soft picks, rubber tip stimulators, air flossers, and/or water flossers. Emerging evidence suggests the use of dental floss may be a possible risk factor for the development of peri-implant diseases. In an observational study of 10 patients with progressive peri-implantitis, remnants of dental floss were found around the neck and coronal portion of dental implants. Brushing with a power toothbrush in conjunction with the use of an antimicrobial was found to be safe and effective for self-care maintenance of implant-supported prostheses.

